Chapter 4
Radiology of the Periodontal Tissues
Aim
To give a concise summary of how to image the periodontal tissues and to provide a comprehensive description of the radiological signs that must be identified for diagnosis of periodontal diseases.
Introduction
The primary diagnostic methods in the assessment of the periodontal tissues are history and clinical examination. Radiology thus serves as an adjunct to clinical assessment. Its principal functions are shown in Table 4-1. As discussed in Chapter 1, any radiograph is a “snapshot” in time; it only serves to provide evidence of the effects of past periodontal disease and does not give meaningful information about current disease activity.
| Identification of bone loss | present or absent? |
| Characterisation of bone loss | localised generalised horizontal pattern vertical defects furcation involvement apical disease bone density/quality loss of lamina dura widening of periodontal membrane space |
| Quantification of bone loss | absolute measurement ratio of CEJ to alveolar crest / CEJ to apex (approximation of % bone loss) bone loss over time |
| Identifying local aggravating factors | calculus poorly contoured restorations tilted teeth caries |
| Other associated features | evidence of occlusal trauma bone sclerosis as a response to disease maxillary sinus changes root resorption hypercementosis |
Radiography of periodontal bone is surprisingly challenging. The three-dimensional shape of the bony supporting tissues of teeth is represented by a two-dimensional image. Thus, localised defects may be masked by superimposed bone. Where irregular defects are recognised, radiography alone cannot portray the three-dimensional shape.
Periodontal Disease Classification
This chapter deals with the general principles of interpretation of the periodontal tissues on radiographs. The gingival diseases are not included for the simple reason that they rarely have any radiological manifestations. Occasionally gingival hypertrophy may be visible radiographically and the thickness of gingivae assessed, particularly where there is a gap between teeth (Fig 4-1). However, as a generalisation, it is reasonable to say that radiology only serves a role in the management of the periodontal diseases. These diseases can be summarised as:
-
plaque-induced periodontal diseases
-
aggressive periodontitis
-
localised
-
generalised
-
recurrent
-
-
chronic periodontitis
-
localised (< 30% sites)
-
generalised (> 30% sites)
-
recurrent
-
refractory periodontitis
-
-
-
systemic diseases affecting periodontal tissues (e.g. pre-pubertal diseases such as hypophosphatasia, Papillon-Lefèvre syndrome).
-
necrotising periodontitis
-
lateral periodontal abscess
-
periodontal-endodontic lesions.
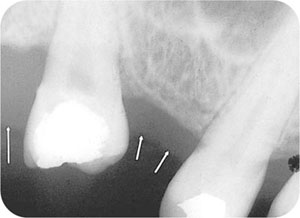
Fig 4-1 Radiograph of 17 and 15 showing gingival outline (arrowed).
All of these share the common feature of bone loss; their differences are in disease pattern and extent, age of onset, speed of progression and management. Details of these specific types of periodontal diseases can be found in textbooks of periodontology. Our role here is to highlight the job of interpreting the common radiological features.
Choice of Radiographs
In 1998, the Faculty of General Dental Practitioners’ publication “Selection Criteria for Dental Radiography” established guidelines for radiography of periodontal diseases. While the strategy of the panel producing these guidelines was to assume an evidence-based approach, they emphasised that there was a paucity of good evidence to produce them. A revision of these guidelines has recently been carried out and the new guidelines are shown in Table 4-2.
| Clinical findings | Radiographs |
| Uniform pocketing < 6 mm and little or no recession | Horizontal posterior bitewings. |
| Uniform pocketing 6 mm or greater | Vertical posterior bitewings, supplemented by periapical radiographs using the parallel ing technique at sites where alveolar bone image is not included. |
| Irregular pocketing | Bitewing radiographs (horizontal or vertical depending on pocket depth), supplemented if necessary by periapical radiographs taken using the paralleling technique. |
| Based upon a history and the clinical examination, the category of 6 mm or greater is equivalent to a basic periodontal examination (BPE) sextant score of Code 4 (assuming no recession). However, remember that the BPE does not assess recession and therefore the GDP cannot rely on the BPE to record attachment loss: a 5 mm pocket adjacent to 4 mm recession is 9 mm attachment loss. | |
| A dental panoramic radiograph (DPR) of optimal quality may offer a dose advantage over large numbers of intraoral radiographs and may be considered as an alternative if available. This may be the case when there are concurrent problems for which radiography is indicated – for example, symptomatic third molars, multiple existing crowns/heavily restored teeth and/or multiple endodontically treated teeth in a patient new to a practice. However, in view of the limitations in fine detail on DPRs, supplementary intraoral radiographs may be necessary for selected sites. | |
The guidelines represent a pragmatic approach suitable for the general dental practitioner and are based upon the foundation of good quality posterior bitewing radiographs. For a dentate patient, bitewing radiographs should be taken at the first visit for caries diagnosis and repeated at appropriate intervals (see Chapter 3). These radiographs demonstrate the periodontal bone in the posterior regions, doing so using an optimal geometry. Thus, for patients with generalised regular bone loss no other radiographs may be needed. Vertical bitewing film holders are available commercially (Fig 4-2) for patients with clinical attachment loss greater than 6 mm. Of course, for many patients you will need to take two films for each side to cover all the posterior teeth using the vertical technique (Fig 4-3).
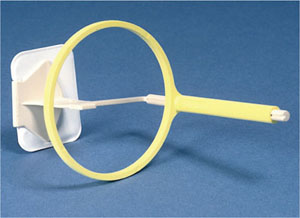
Fig 4-2 Vertical bitewing holder.

Fig 4-3 Vertical bitewing radiograph.
A traditional method of assessing the periodontal bone is the full-mouth periapical survey. This undoubtedly provides comprehensive coverage and allows calculation of residual bone support that facilitates prognostic decision-making. The full mouth survey requires many individual radiographs, however, adding to the radiation dose. Where periapical radiographs are taken, it is essential to use the paralleling technique. With the bisecting angle technique, particularly in the upper jaw, the angulation of the x-ray beam will project the buccal plate of bone coronally, masking periodontal bone loss (Fig 4-4).

Fig 4-4 On the left is part of a bisecting angle technique radiograph, while on the right is part of a paralleling technique radiograph of t/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


