CHAPTER 4. Pulpitis, apical periodontitis, resorption and hypercementosis
PULPITIS → Summaries pp. 66, 448
Pulpitis is the most common cause of dental pain and loss of teeth in younger persons. The usual cause is caries penetrating the dentine, but there are other possibilities (Box 4.1). Pulpitis, if untreated, is followed by death of the pulp and spread of infection through the apical foramina into the periapical tissues. This in turn causes periapical periodontitis.
Box 4.1
Causes of pulpitis
• Dental caries
• Traumatic exposure of the pulp
• Fracture of a crown or cusp
• Cracked tooth syndrome
• Thermal or chemical irritation
Dental caries is by far the most common cause and is usually obvious unless it is concealed beneath a restoration.
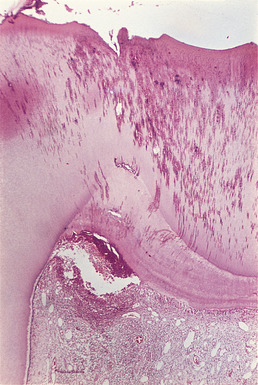
Exposure during cavity preparation allows bacteria to enter the pulp and also damages it mechanically (Fig. 4.1).
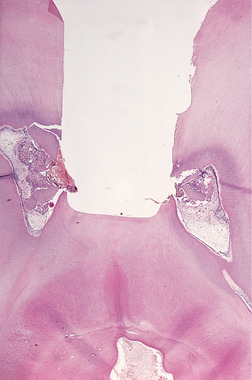 |
| Fig. 4.1
Traumatic exposure. The pulp has been exposed during cavity preparation and dentine chippings and larger fragments have been driven into the pulp. The tooth was extracted before a strong inflammatory reaction has had time to develop, but it is clear that some inflammatory cells have already localised around the debris which will have introduced many bacteria to the pulp.
|
Fracture may either open the pulp chamber or leave so thin a covering of dentine that bacteria can enter.
A tooth, particularly a restored premolar, may split, usually under masticatory stress (Fig. 4.2). These minute cracks are often invisible, but allow bacteria into the pulp chamber. The affected tooth may sometimes be identified by applying pressure to the occlusal fissure with a ball-ended burnisher to open up the crack. Pulp pain usually then results. Alternatively, the crack may be made visible with oblique transillumination or, possibly more easily, by wetting the crown of the tooth with a dye such as fluorescein and visualising it with ultraviolet light.
 |
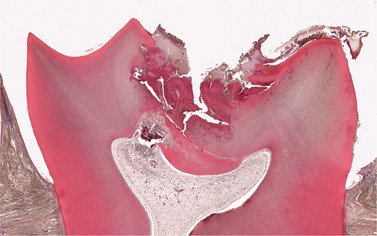
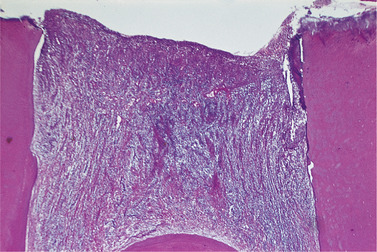
| Fig. 4.2
Cracked tooth. The pulp died beneath this crack which was undetected clinically but which has opened up after decalcification of the tooth.
|
Insufficient cooling during cavity cutting, especially of deep cavities, can cause immediate damage to the pulp. Large unlined metal restorations may also allow continuous low-grade thermal stimuli to damage the pulp over a longer period. Some restorations without a protective lining, particularly in the past, were sufficiently irritant to kill the pulp.
Clinical features
The pulps of individual teeth are not precisely represented on the sensory cortex. The pulp pain is therefore poorly localised and may be felt in any of the teeth of the upper or lower jaw of the affected side. Rarely, pain may be referred to a more distant site such as the ear. Pulp pain is not provoked by pressure on the tooth. The patient can chew in comfort unless there is a large open cavity allowing fragments of food to press on the pulp through the softened dentine.
Acute pulpitis
In the early stages the tooth is hypersensitive. Very cold or hot food causes a stab of pain which stops as soon as the irritant is removed. As inflammation progresses, pain becomes more persistent and there may be prolonged attacks of toothache. The pain may start spontaneously, often when the patient is trying to get to sleep.
The pain is partly due to the pressure on the irritated nerve endings by inflammatory infiltrate within the rigid pulp chamber and partly due to release of pain-producing substances from the damaged tissue. The pain at its worst is excruciatingly severe, sharp and stabbing in character. It is little affected by simple analgesics.
The outcome of acute pulpitis is unpredictable. Acute pulpitis may be deemed irreversible on the basis of constant severe pain or the persistence of pain after a hot or cold stimulus but, even then, the pulp may survive. Though pulp death is the likely outcome, acute pulpitis may progress to chronic pulpitis and treatment can still preserve pulp vitality. Diagnosis of irreversible pulpitis is considered an indication for extirpation of the pulp, but it must be recognized that the criteria are poorly defined.
Chronic pulpitis
Chronic pulpitis may develop with or without episodes of acute pulpitis. However, many pulps under large carious cavities die painlessly. The first indication is then development of periapical periodontitis, either with pain or seen by chance in a radiograph. In other cases, there are bouts of dull pain, brought on by hot or cold stimuli or coming on spontaneously. There are often prolonged remissions and there may be recurrent acute exacerbations.
Pathology
Pulpitis may result from a variety of causes (see Box 4.1). Pulpitis caused by caries results from penetration of acid and bacterial products through the dentine and, later, from a mixed bacterial infection penetrating to the pulp.
Acute closed pulpitis
Histologically, there is initial hyperaemia limited to the area immediately beneth the irritant (Fig. 4.3). Infiltration by inflammatory cells and destruction of odontoblasts and adjacent mesenchyme follow. A limited area of necrosis may result in formation of a minute abscess, localised by granulation tissue (Fig. 4.4, Fig. 4.5, Fig. 4.6 and Fig. 4.7). Later, inflammation spreads until the pulp is obliterated by dilated blood vessels and acute inflammatory cells (Fig. 4.8). Necrosis follows.
 |
| Fig. 4.3
Pulpal hyperaemia. While bacteria are still some distance from the pulp, acid permeating along the dentinal tubules gives rise to hyperaemia, oedema and a light cellular inflammatory infiltrate in the pulp.
|
 |
| Fig. 4.4
Acute pulpitis. Low-power view showing occlusal caries penetrating to the pulp through a layer of reactionary dentine. There is acute inflammation localised to the pulp horn.
|
 |
| Fig. 4.5
Acute pulpitis. Beneath the carious exposure (top right) a dense inflammatory infiltrate is accumulating. More deeply, the pulp is intensely hyperaemic.
|
 |
| Fig. 4.6
Acute pulpitis. Infection has penetrated the reactionary dentine causing inflammation to spread down the pulp and pus to form in the corner.
|
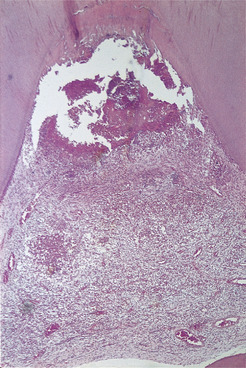 |
| Fig. 4.7
Acute caries and pulpitis. Infection has penetrated to the pulp. Part of the pulp has been destroyed and an abscess has formed, containing a bead of pus.
|
 |
| Fig. 4.8
Acute pulpitis – terminal stage. The entire pulp has been destroyed and replaced by inflammatory cells and dilated vessels.
|
Chronic closed pulpitis
The main features are a predominantly mononuclear cell infiltrate and a more vigorous connective tissue reaction. A small area of pulpal necrosis and pus formation may be localised by a well-defined wall of granulation tissue and a minute abscess may thus form. The remainder of the pulp may then appear normal.
Rarely, inflammation may be well localised beneath an exposure so that a partial calcific barrier forms beneath the lesion, or considerable amounts of reactionary dentine continue to form round the opening. Such changes are particularly likely to follow pulp capping. Calcific barriers (seen radiographically as ‘dentine bridges’) are frequently poorly formed and inflammation progresses beneath them (Figs 4.9 and 4.10). However, in successful cases, formation of a complete barrier of tubular reactionary dentine may allow preservation of the remainder of the pulp.
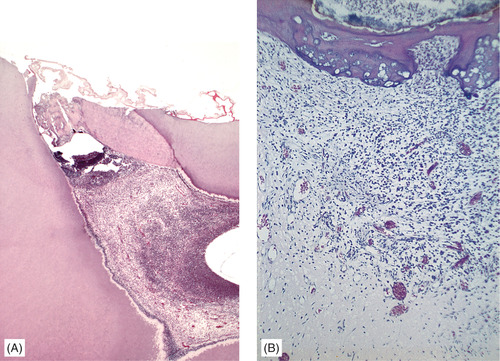 |
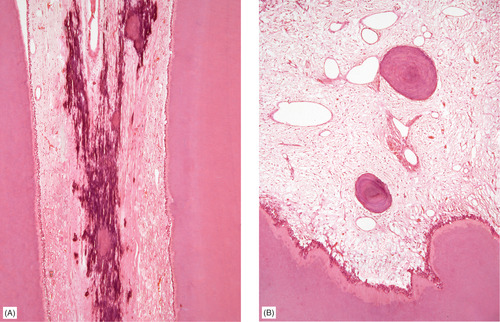
| Fig. 4.9
Calcific barriers. (A) Another pulpitis and formation of a thick calcific barrier, but with an abscess immediately below it. The rest of the pulp is inflamed. (B) This higher-power view of another barrier induced by pulp capping shows the calcific barrier in more detail, in particular its irregular structure and failure to hold back the infection.
|
 |
| Fig. 4.10
Pulp capping. The procedure has allowed the pulp to survive until reactionary dentine has proliferated greatly beside the exposure. Failure of the procedure is indicated by the inflammatory cells concentrated below the opening.
|
The chief factor hampering pulpal survival is its enclosure within the rigid walls of the pulp chamber and, in fully formed teeth, the limited aperture for the apical vessels. In acute inflammation, these vessels can readily be compressed by inflammatory oedema and thrombose. The blood supply of the pulp is thus cut off and it dies. This may be rapid in the case of acute pulpitis, or delayed in chronic lesions. The relatively prolonged survival of chronically inflamed pulps is shown by the persistence of symptoms over a long period. However, pulp death is the end result unless treatment is successful.
Open pulpitis
Occasionally the pulp survives but is chronically inflamed, beneath a wide exposure, despite the heavy infection (Fig. 4.11). This is traditionally believed to be associated with open apices which allow an adequate blood supply.
 |
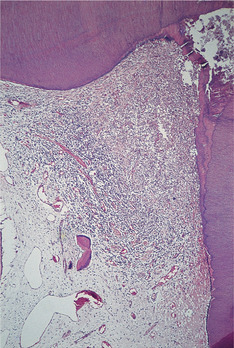
| Fig. 4.11
Open pulpitis. Beneath the wide exposure the pulp has survived in the form of granulation tissue with the most dense inflammatory infiltrate beneath the open surface.
|
Chronic hyperplastic pulpitis (pulp polyp)
Rarely, despite wide exposure and heavy infection, the pulp not merely survives but proliferates through the opening. This may even happen in fully formed teeth.
Clinically, a pulp polyp appears as a dusky red or pinkish soft nodule protruding into the cavity. It is painless but may be tender and bleed on probing. It should be distinguished from proliferating gingival tissue extending over the edge of the cavity by tracing its attachment (Fig. 4.12).
 |
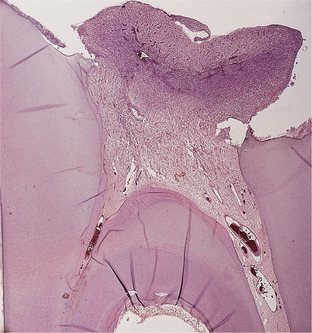
| Fig. 4.12
Pulp polyp. An inflamed nodule of granulation tissue can be seen growing from the pulp chamber of this broken down first permanent molar.
|
Histologically, few odontoblasts survive and the pulp becomes replaced by granulation tissue (Fig. 4.13). As this mass grows out into the cavity in the tooth it can become epithelialised and covered by a layer of well-formed stratified squamous epithelium. This protects the mass and allows inflammation under it to subside and fibrous tissue to replace the granulation tissue. This degree of pulpal proliferation can occasionally be seen in teeth with fully formed roots (Fig. 4.14).
 |
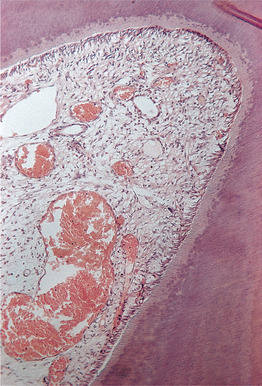
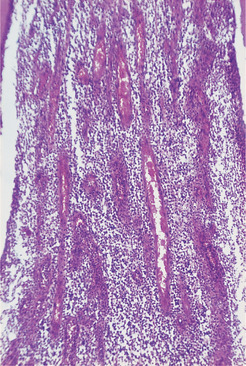
| Fig. 4.13
Pulp polyp. A hyperplastic nodule of tissue is growing out through a wide exposure of the pulp. The masses of inflammatory cells and the many new vessels are characteristic of granulation tissue.
|
 |
| Fig. 4.14
Pulp polyp. In this broken down molar, granulation tissue is proliferating from the pulp cavity and has acquired an epithelial covering over much of its surface. Note also the internal resorption (left) as a result of pulpal inflammation.
|
Management
The chances of survival of an inflamed pulp are poor and treatment options are limited (Box 4.2).
Box 4.2
Treatment options for pulpitis
• If fractured or cracked, stabilise fracture and seal pulp temporarily
• Removal of caries, obtundent or steroid dressing
• Removal of caries and pulp capping
• Pulpotomy in deciduous teeth
• Endodontic treatment
• Extraction
• Analgesics are largely ineffective
Open pulpitis is usually associated with gross cavity formation and it is rarely possible to save the tooth, despite the vitality of the pulp.
Key features of pulpitis are summarised in Box 4.3 and the sequelae of pulpitis are shown in Summary chart 4.1.
Box 4.3
Key features of pulpitis
• Pulpitis is caused by infection or irritation of the pulp, usually by caries
• Severe stabbing pain in a tooth, triggered by hot or cold food or starting spontaneously, indicates acute irreversible pulpitis
• Pulp pain is poorly localised
• Chronic pulpitis is often symptomless
• Untreated pulpitis usually leads to death of the pulp and spread of infection to the periapical tissues
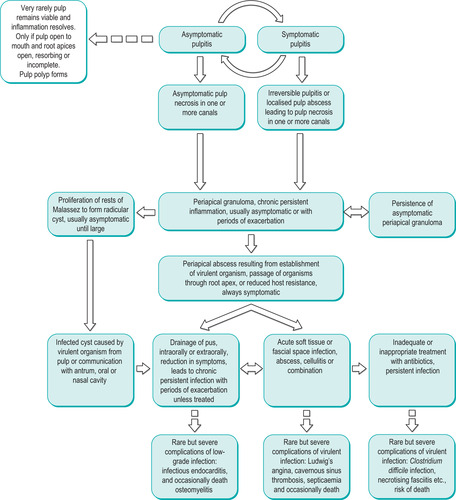 |
| Summary chart 4.1
Sequelae of pulpitis.
|
PULP CALCIFICATIONS
Pulp stones
Rounded masses of dentine may form within the pulp and can be seen in radiographs as small opacities. In the past, they were thought to cause symptoms but are developmental anomalies. For unknown reasons, they are common in the teeth of patients with Ehlers–Danlos (floppy joint) syndrome, a genetic defect of collagen formation.
Histologically, pulp stones consist of dentine which may show complete or incomplete tubule formation (Fig. 4.15). A distinction used to be drawn between free and attached pulp stones. However, this is frequently an illusion caused by a plane of section which fails to pass through the connection between the pulp stone and the pulp wall.
 |
| Fig. 4.15
Pulp stones. (A) The dystrophic pulp mineralisations often found as an age change. (B) Rounded nodules of calcified tissue, in this case resembling bone rather than dentine.
|
Diffuse calcification
Amorphous dystrophic calcifications may sometimes be seen histologically in the pulp and are thought to be an age-related degenerative change.
Pulp stones and diffuse calcification are of no clinical significance except insofar as they may obstruct endodontic treatment. Otherwise they can be ignored.
PERIAPICAL PERIODONTITIS → Summary p. 66
Periapical inflammation is usually due to spread of infection following death of the pulp (Box 4.4). It characteristically causes tenderness of the tooth in its socket. Local (periapical) periodontitis must be distinguished from chronic (marginal) periodontitis in which infection and destruction of the supporting tissues spread from chronic infection of the gingival margins (Ch. 5).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


