Chapter 4
Orthodontics
Contents
Relevant pages in other chapters Surgical management of CLP, p. 472; abnormalities of eruption, p. 62; supernumerary teeth, p. 64; orthognathic surgery, p. 474.
Further reading BOS 1996 Young Practitioners Guide to Orthodontics. T.M. Graber et al. 2005 Orthodontics—Current principles and techniques (4e), Elsevier Mosby. K.G. Isaacson et al. 2008 Orthodontic Radiographs—Guidelines, BOS. L. Mitchell 2007 An Introduction to Orthodontics (3e) OUP. W. R. Proffit et al. 2007 Contemporary Orthodontics (4e), Mosby.
It has been said that orthodontists forget to ask the patient to open wide, thus missing any dental pathology, whilst generalists forget to ask the patient to close together, thus missing any malocclusion! The aim of this chapter is to help ensure that this is not true. A problem-orientated approach has been used (rather than by classification) for simplicity.
What is orthodontics?
Orthodontics has been defined as that branch of dentistry concerned with growth of the face, development of the dentition, and prevention and correction of occlusal anomalies.1
Prevalence of malocclusion
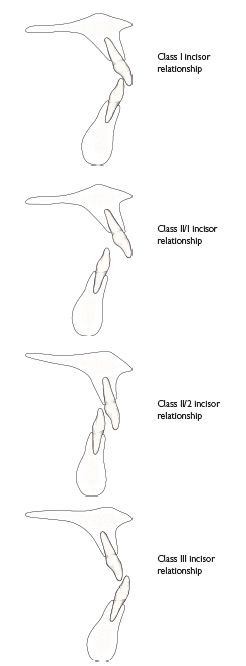
Crowding approx. 60%; Class II/1 ~15–20%; Class II/2 ~10%; Class III ~3% (Figure 4.1).
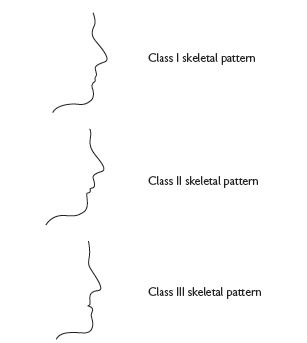
Fig. 4.1
Why do orthodontics?
Research shows that individual motivation has more effect upon the presence of plaque than alignment of the teeth, therefore, the main indications for orthodontic Rx are aesthetics and function. Functional reasons for Rx include deep traumatic overbite; ↑ overjet especially if the lips are incompetent (↑ risk of trauma), and labial crowding of a lower incisor (as this reduces periodontal support labially). While it is accepted that severe malocclusion may affect self-esteem and psychological well-being, the impact of more minor anomalies and, indeed, perceived need, are influenced by social and cultural factors. The Index of Orthodontic Treatment Need (IOTN) has been developed to try to standardize and quantify this difficult issue (p. 122).
It is important that patients realize that orthodontic Rx is not without its disadvantages. Even with good OH, a small loss of periodontal attachment is common and with poor OH this will be ↑. Decalcification (decay) will occur if there are frequent sugar intakes between meals and around 1–2mm of root resorption is associated with fixed appliance Rx and in at-risk patients (shortened/blunt root shape) this may be ↑. Therefore, the potential benefits to the patient must be sufficient to counter-balance these risks.
Who should do orthodontics?
All dentists should be concerned with growth and development. Unless anomalies are detected early and any necessary steps taken at the appropriate time, then provision of the best possible outcome for that patient is less likely. Most orthodontic Rx in Europe is now carried out by trained specialist orthodontic practitioners. In the UK the hospital consultant service acts as a source of advice and a referral point for more complex and multidisciplinary problems.
When should we do orthodontics?
This depends upon the particular anomaly. In the early mixed dentition, Rx is only indicated to correct incisor and/or posterior Xbites with displacement. Functional appliance Rx may be started in the mixed dentition to coincide with the pubertal growth spurt; however, the majority of orthodontic Rx is not started until the 2° dentition. Rx during the early teens is preferable because the response to orthodontic forces is more rapid, appliances are better tolerated, and, most importantly, growth can be utilized to help effect sagittal or vertical change. In adults, lack of growth; ↑risk of periodontal disease; worn, damaged and missing teeth and slower tooth movement and will limit the type of malocclusion that can be tackled by orthodontics alone. The proportion of adult orthodontic patients is ↑.
 If in doubt, refer a patient for advice earlier rather than later, especially in cases with marked skeletal discrepancies.
If in doubt, refer a patient for advice earlier rather than later, especially in cases with marked skeletal discrepancies.
The Index of Orthodontic Treatment Need
The IOTN was developed to quantify and standardize an individual patient’s need for orthodontic Rx, so that the potential benefits can be weighed against the possible disadvantages.1 The Index consists of two components:
The dental health component
was developed from an index used by the Swedish Dental Health Board (which was used to determine the amount of financial help that would be given by the State towards Rx costs). The Dental Health Component of IOTN (reproduced by kind permission of University of Manchester) has five categories of Rx need, ranging from little need to very great need. A patient’s grade is determined by recording the single worst feature of their malocclusion. MOCDO is helpful when assessing dental health component as it provides a hierarchy of severity—Missing teeth; Overjet; Crossbite; Displacement; Overbite.
The aesthetic component
is based on a series of 10 photographs of the labial aspect of different class I or class II malocclusions, which are ranked according to their attractiveness. A patient’s score is determined by the photograph, which is deemed to have an equivalent degree of aesthetic impairment.
The Index of Orthodontic Treatment Need
(Copyright © University of Manchester)
Grade 1 (None)
Grade 2 (Little)
| 2a | Increased overjet 3.6–6mm with competent lips. |
| 2b | Reverse overjet 0.1–1mm. |
| 2c | Anterior or posterior crossbite with up to 1mm discrepancy between retruded contact position and intercuspal position. |
| 2d | Displacement of teeth 1.1–2mm. |
| 2e | Anterior or posterior openbite 1.1–2mm. |
| 2f | Increased overbite 3.5mm or more, without gingival contact. |
| 2g | Pre-normal or post-normal occlusions with no other anomalies. Includes up to half a unit discrepancy. |
Grade 3 (Moderate)
| 3a | Increased overjet 3.6–6mm with incompetent lips. |
| 3b | Reverse overjet 1.1–3.5mm. |
| 3c | Anterior or posterior crossbites with 1.1–2mm discrepancy. |
| 3d | Displacement of teeth 2.1–4mm. |
| 3e | Lateral or anterior openbite 2.1–4mm. |
| 3f | Increased and complete overbite without gingival trauma. |
Grade 4 (Great)
| 4a | Increased overjet 6.1–9mm. |
| 4b | Reversed overjet greater than 3.5mm with no masticatory or speech difficulties. |
| 4c | Anterior or posterior crossbites with greater than 2mm discrepancy between retruded contact position and intercuspal position. |
| 4d | Severe displacement of teeth, greater than 4mm. |
| 4e | Extreme lateral or anterior openbites, greater than 4mm. |
| 4f | Increased and complete overbite with gingival or palatal trauma. |
| 4h | Less extensive hypodontia requiring pre-restorative orthodontic space closure to obviate the need for a prosthesis. |
| 4l | Posterior lingual crossbite with no functional occlusal contact in one or both buccal segments. |
| 4m | Reverse overjet 1.1–3.5mm with recorded masticatory and speech difficulties. |
| 4t | Partially erupted teeth, tipped and impacted against adjacent teeth. |
| 4x | Supplemental teeth. |
Grade 5 (Very great)
| 5a | Increased overjet greater than 9mm. |
| 5h | Extensive hypodontia with restorative implications (more than one tooth missing in any quadrant) requiring pre-restorative orthodontics. |
| 5i | Impeded eruption of teeth (with the exception of third molars) due to crowding, displacement, the presence of supernumerary teeth, retained deciduous teeth, and any pathological cause. |
| 5m | Reverse overjet greater than 3.5mm with reported masticatory and speech difficulties. |
| 5p | Defects of cleft lip and palate. |
| 5s | Submerged deciduous teeth. |
Definitions
Ideal occlusion
Anatomically perfect arrangement of the teeth. Rare.
Normal occlusion
Acceptable variation from ideal occlusion.
Competent lips
Lips meet together at rest.
Incompetent lips
Lips do not meet together at rest.
Frankfort plane
Line joining porion (superior aspect of external auditory meatus) with orbitale (lowermost point of bony orbit).
Class I
The lower incisor edges occlude with, or lie immediately below the cingulum of upper incisors (Figure 4.2).
Class II
The lower incisor edges lie posterior to the cingulum of the upper incisors. Division 1 the upper central incisors are upright or proclined and the overjet is ↑ (Figure 4.3). Division 2 the upper central incisors are retroclined and the overjet is usually ↓ but may be ↑ (Figure 4.4).
Class III
The lower incisor edges lie anterior to the cingulum of the upper incisors and the overjet is ↓ or reversed (Figure 4.5).
Bimaxillary proclination
Both upper and lower incisors are proclined.
Overjet
Distance between the upper and lower incisors in the horizontal plane.
Overbite
Overlap of the incisors in the vertical plane.
Complete overbite
The lower incisors contact the upper incisors or the palatal mucosa.
Incomplete overbite
The lower incisors do not contact the upper incisors or the palatal mucosa.
Anterior open bite
There is no vertical overlap of the incisors when the buccal segment teeth are in occlusion.
Crossbite
A deviation from the normal bucco-lingual relationship. May be anterior/posterior &/or unilateral/bilateral.
Buccal crossbite
Buccal cusps of lower premolars or molars occlude buccally to the buccal cusps of the upper premolars or molars.
Lingual crossbite
Buccal cusps of lower molars occlude lingually to the lingual cusps of the upper molars.
Dento-alveolar compensation
The position of the teeth has compensated for the underlying skeletal pattern, so that the occlusal relationship between the arches is less severe.
Leeway space
The difference in diameter between C, D, E, and 3, 4, 5. Greater in lower than upper arch.
Mandibular deviation
Path of closure starts from a postured position of the mandible.
Mandibular displacement
When closing from the rest position, the mandible displaces (either laterally or anteriorly) to avoid a premature contact.
Orthodontic assessment
Equipment
A mirror, probe, a SS ruler and ‘sharp’ eyes.
Brief screening procedure
The purpose of this is to ensure early detection and Rx of any abnormality, prepare the patient for any later Rx and influence the management of any teeth of poor prognosis.
At every visit
Once the 2° incisors have erupted and until 2° dentition is established (if in doubt refer).
From age 9yrs and until they erupt, palpate for  in the buccal sulcus. A definite hollow &/or asymmetry warrants further investigation.
in the buccal sulcus. A definite hollow &/or asymmetry warrants further investigation.
Detailed orthodontic examination
Should be carried out in a logical sequence so that nothing is missed.
EO examination (with Frankfort plane horizontal)
 and how the patient achieves an oral seal (? lip to lip; lip to tongue; or by the lower lip being drawn up behind the incisors). Note also the length of the upper lip, the amount of
and how the patient achieves an oral seal (? lip to lip; lip to tongue; or by the lower lip being drawn up behind the incisors). Note also the length of the upper lip, the amount of  seen, and lip tonicity.
seen, and lip tonicity.IO examination
 .
. .
.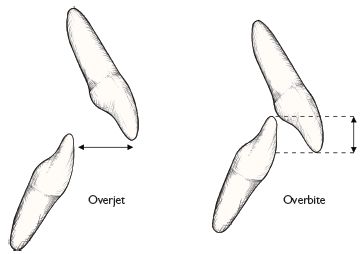
Fig. 4.6
X-rays
Usually a DPT is taken and, if not clearly visible on the DPT, an intraoral of the  . A lateral skull view is indicated if the patient has a skeletal discrepancy or A–P movement of the incisors is anticipated.
. A lateral skull view is indicated if the patient has a skeletal discrepancy or A–P movement of the incisors is anticipated.
Summary
Should include a description of the patient’s incisor relationship and skeletal pattern, and the main points of the malocclusion, e.g. crowding, Xbites. This gives a ‘problem list’ from which the aims of Rx can be derived (p. 132).
Study models
are not obligatory, but are advisable to facilitate treatment planning (at leisure); medico-legally; to provide evidence as to the justification for treatment; for measuring the progress and outcome of treatment and also for those bodies commissioning & paying for treatment. Study models should be trimmed so that they occlude correctly on a flat surface.
Cephalometrics
Cephalometric analysis is the interpretation of lateral skull radiographs (Figure 4.7). It is not obligatory for orthodontic ∆ and where the incisor position is not to be changed significantly, the X-ray exposure may not be justified for the information gained. However, where A–P movement is required, a lateral skull radiograph will back-up the clinical assessment of skeletal pattern, and help to determine the degree of difficulty and type of appliance indicated. Serial lateral skulls aid assessment of growth.
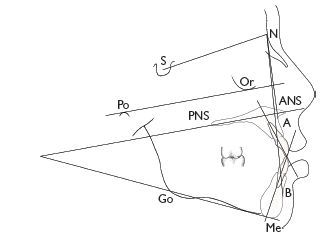
Fig. 4.7 Most commonly used cephalometric points:
| S | = | Sella: mid-point of sella turcica. |
| N | = | Nasion: most anterior point on fronto-nasal suture. |
| Or | = | Orbitale: most inferior anterior point on margin of orbit (take average of two images). |
| Po | = | Porion: uppermost outermost point on bony external auditory meatus. |
| ANS | = | Anterior nasal spine. |
| PNS | = | Posterior nasal spine. |
| Go | = | Gonion: most posterior inferior point on angle of mandible. |
| Me | = | Menton: lowermost point on the mandibular symphysis. |
| A | = | A point: position of deepest concavity on anterior profile of maxilla. |
| B | = | B point: position of deepest concavity on anterior profile of mandibular symphysis. |
| Frankfort plane | = | Po–Or. |
| Maxillary plane | = | PNS–ANS. |
| Mandibular plane | = | Go–Me. |
Tracing/digitizing
Although this has been done using grease-proof paper and a TV as background illumination (yes, really!), the quality of diagnostic information so obtained is limited. Tracing paper (secured to the film with masking tape), a sharp pencil (a 0.5mm propelling-pencil is ideal), and good background illumination are essential. Digital images can be digitized directly. Spotting orthodontic landmarks is infinitely easier if carried out in a darkened room. If a point is hard to see, block off the rest of the film so that only that area is illuminated. If this fails, try holding the film up to a bright spotlight, but if still not clear, make a guesstimate! Due to the slight magnification (7–8%), two images of the mandibular border are usually seen. Both should be traced and an average taken for gonion. By convention, the most prominent image should be traced, i.e. the most anterior in the face so that the difficulty of Rx is not underestimated.
Pitfalls
Lower facial height (LFH)
is the distance from anterior nasal spine to menton as a percentage of the total face height (from nasion to menton).
More cephalometrics
Analysis and interpretation
The analysis of lateral skull tracings is carried out by comparing a number of angular measurements and proportions with average values for the population as a whole. Normal values for Caucasians (UK),1 standard deviations in parentheses:
| SNA | = 81°(±3) |
| SNB | = 79°(±3) |
| ANB | = 3°(±2) |
 -Max -Max |
= 109°(±6) |
| 1-Mand | = 93°(±6) or 120 minus MMPA |
| MMPA | = 27°(±4) |
| Facial proportion | = 55% (±2) |
| Inter-incisal angle | = 133° (±10) |
When interpreting a tracing bear in mind the following rules of thumb:
It is important to remember that the ANB difference is not an infallible assessment of skeletal pattern as it assumes (incorrectly in some cases) that there is no discrepancy in the cranial base and that A and B are indicative of basal bone position. When a cephalometric tracing seems at odds with your clinical impression it is worth doing another analysis which avoids reliance on the cranial base, such as a Wits analysis.
Before deciding on a Rx plan it is helpful to consider what factors have contributed to a particular malocclusion, e.g. in a patient with a Class II/1 incisor relationship on a Class I skeletal pattern, the prognosis for Rx is much better if the ↑ o/j is due to proclination of the upper rather than retroclination of the lower incisors. The relative contribution of the maxilla and mandible to the skeletal pattern may indicate possible lines of Rx; e.g. if an ↑ o/j is due to a retrusive mandible, a better aesthetic result may be achieved by use of a functional appliance.
As a rough guide can assume that there is ~2.5° of angular movement for every millimetre of linear movement of the incisor edge.
Wits analysis
Used to assess antero-posterior skeletal pattern (Figure 4.8).
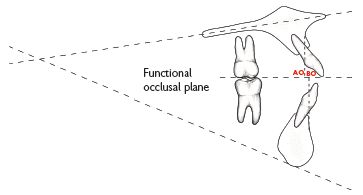
Fig. 4.8 Wits analysis.
Method:
In Class I AP relationship:
Males: BO is 1mm (±1.9mm) ahead of AO
Females: BO=AO (±1.77mm)
Treatment planning
Problem list
Following assessment of the patient a summary should be made of the main features of the malocclusion (p. 127). The problem list can then be drawn up; e.g.
Aims of Rx
This is derived from the above problem list; e.g.
Plan lower arch
The lower arch lies in a zone of stability between the lips, cheeks, and tongue; therefore, it is safer to consider it as immutable. This gives a starting point around which to plan Rx. The first step is to decide if the lower arch is sufficiently crowded to warrant extractions. If the crowding is likely to ↑ (patient in early teens), then extractions may be indicated (p. 136). In Class 11/2 cases it may be advisable to accept a little crowding (p. 147). If in doubt refer for advice.
Plan upper arch
In most cases planning will be to a Class I incisor and buccal segment relationship. Therefore, it may be helpful, in the mind’s eye, to correct the upper canine into a Class I relationship with  (in corrected position if LLS crowded). This will give an indication of the space required and the amount and type of movement necessary. In the upper arch, space for retraction of
(in corrected position if LLS crowded). This will give an indication of the space required and the amount and type of movement necessary. In the upper arch, space for retraction of  can be gained by (i) extractions, (ii) expansion (only indicated if a Xbite exists), (iii) distal movement of the upper buccal segments (p. 138). (iv) a combination of these. Should extractions be indicated in both arches, mechanics are often easier if the same tooth is extracted in the upper as in the lower. However, in Class II cases it may be advantageous to extract further forward in the upper arch and vice versa in Class III.
can be gained by (i) extractions, (ii) expansion (only indicated if a Xbite exists), (iii) distal movement of the upper buccal segments (p. 138). (iv) a combination of these. Should extractions be indicated in both arches, mechanics are often easier if the same tooth is extracted in the upper as in the lower. However, in Class II cases it may be advantageous to extract further forward in the upper arch and vice versa in Class III.
Final Rx plan
The next step is to plan what tooth movements need to be carried out, including which appliances are to be used and in what sequence. E.g. if distal movement of  is to be carried out it may be wise to fit the headgear first and review in the light of progress before embarking on extractions. To every force there is an equal and opposite reaction. In orthodontic treatment the resistance to unwanted tooth movement is called anchorage and also needs to be considered when planning Rx. Retention of the final result should be included in the Rx plan and the need for compliance with wearing retention appliances explained to the patient.
is to be carried out it may be wise to fit the headgear first and review in the light of progress before embarking on extractions. To every force there is an equal and opposite reaction. In orthodontic treatment the resistance to unwanted tooth movement is called anchorage and also needs to be considered when planning Rx. Retention of the final result should be included in the Rx plan and the need for compliance with wearing retention appliances explained to the patient.
The practicalities of providing Rx also warrant consideration. In some cases more than one Rx plan can be offered to the patient, with a hierarchy of complexity and finished result. If a compromise plan is chosen by the patient this should be recorded in the consent process.
The final plan for the example above may be:
Prognosis
Will the proposed Rx be stable? Beware of o/j reduction in a patient with grossly incompetent lips, or proclination of upper incisors in a Class III where there is no o/b to hold the corrected position.
Consent
The risks and benefits of the proposed plan should be carefully explained to the patient/parent. It is advisable to get written consent, including specific details of the Rx and associated risks.
 Beware if the malocclusion under consideration contains one of the following features:
Beware if the malocclusion under consideration contains one of the following features:
Rx planning is the most important, and most difficult, part of orthodontics. All but the trained orthodontist are advised to seek specialist advice.
Management of the developing dentition
See also delayed eruption, p. 62.
The way in which mixed dentition problems are approached will often affect the ease or difficulty of subsequent Rx.
Normal development of dentition
The 1° incisors are usually upright and spaced. If there is no spacing warn the parents that the 2° incisors will probably be crowded. Overbite reduces throughout the 1° dentition until the incisors are edge to edge. All 2° incisors develop lingual to their predecessors, erupt into a wider arc, and are more proclined. It is normal for  to erupt with a median diastema which reduces as
to erupt with a median diastema which reduces as  erupt. Later, pressure from the developing canines on the roots of
erupt. Later, pressure from the developing canines on the roots of  results in their being tilted distally and spaced. This has been called the ‘ugly duckling stage’, but it is better to describe it as normal development to parents. As the
results in their being tilted distally and spaced. This has been called the ‘ugly duckling stage’, but it is better to describe it as normal development to parents. As the  erupts the
erupts the  upright and the spaces usually close.
upright and the spaces usually close.
The majority of Es erupt so that their distal edges are flush. The transition to the normal stepped (Class I) molar relationship usually occurs during the 2° dentition as a result of greater mandibular growth &/or the leeway space.
Development of dental arches
In the average (!) child, the size of the dental arch is more or less established once the deciduous dentition has erupted, except for an increase in inter-canine width (2–3mm up to age 9yrs) which results in a modification of arch shape.
Retained deciduous teeth
—if deflecting eruption of 2° tooth, extract.
Infraoccluded deciduous molars
Prevalence 8–14%. Provided there is a successor, an infraoccluded 1° molar will probably be exfoliated at the same time as the contralateral tooth.1 Extraction is only indicated if there is no successor or the infraoccluded molar is likely to disappear below the gingival margin.
Impacted upper first permanent molars
Prevalence 2–6%. Indicative of crowding. Spontaneous disimpaction rare after 8 yrs. Can try dislodging  by tightening a piece of brass wire round the contact point with
by tightening a piece of brass wire round the contact point with  over several visits. Otherwise just observe, extracting
over several visits. Otherwise just observe, extracting  if unavoidable and dealing with resultant space loss in 2° dentition.
if unavoidable and dealing with resultant space loss in 2° dentition.
Habits
Effects produced depend upon duration of habit and intensity. It is best not to make a great fuss of a finger-sucking habit. If parents concerned, reassure them (in presence of child) not to worry, as only little girls/boys suck their fingers. Appliances to break the habit may help, but most children will stop when they are ready. However, this is no reason to delay the start of Rx for other aspects of the malocclusion.
Effects of premature loss of deciduous teeth
Unfortunately, when a child attends with toothache, in the rush to relieve pain it is all too easy to extract the offending tooth without consideration of the consequences. The major effect of early deciduous tooth loss is localization of crowding, in crowded mouths. The extent to which this occurs depends upon the patient’s age, degree of crowding, and the site. In a crowded mouth the adjacent teeth will move round into the extraction space, therefore, unilateral loss of a C (and to a lesser degree a D) will result in a centre-line shift. This is also seen when a C is prematurely exfoliated by an erupting 2. As correction of a centre-line discrepancy often involves fixed appliances, prevention is better than cure, so loss of Cs should always be balanced. If Es are lost the 6 will migrate forward. This is particularly marked if it occurs before eruption of the permanent tooth, so if extraction of an E is unavoidable try to defer until after the 6s are in occlusion and do not balance or compensate.
The effect of early loss of 1° teeth on the eruption of the permanent successor is variable.
Timely loss of Cs is indicated for
 erupting palatally due to crowding. Extraction of
erupting palatally due to crowding. Extraction of  as the
as the  erupting may allow the tooth to escape labially and prevent a Xbite.
erupting may allow the tooth to escape labially and prevent a Xbite. when a lower incisor is being crowded labially will help to ↓ loss of periodontal support.
when a lower incisor is being crowded labially will help to ↓ loss of periodontal support.
Balancing extraction
Extraction of the same (or adjacent) tooth on the opposite side of the arch to preserve symmetry.
Compensating extraction
Extraction of the same tooth in the opposing arch.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses