Measuring Progress in Oral Health
Jane E.M. Steffensen, RDH, BS, MPH, CHES
Upon completion of this chapter, the student will be able to:
• Discuss the national Healthy People initiatives.
• Describe the oral health objectives of Healthy People 2010 and 2020.
• Discuss measures used to assess oral health in populations.
• Compare and contrast the procedures and methods used in oral health surveys.
Opening Statement
National 2010 Objectives for Leading Health Indicators*
| •Increase access to health insurance | •100% of children and adults (younger than 65 years) have health insurance |
| •Increase access to personal health care | •96% of children and adults have a source of ongoing primary health care |
| •Increase access to prenatal care | •90% of pregnant women receive prenatal care during the first trimester |
| •Immunizations | •80% of young children (aged 19 to 35 months) are fully immunized |
| •Increase physical activity | •50% of adults are physically active on a regular basis |
| •Decrease obesity | •15% of adults are obese |
| •Decrease tobacco use | •12% of adults smoke cigarettes |
| •Decrease substance abuse | •89% of adolescents do not use alcohol or illicit drugs during the past month |
| •Increase access to mental health services | •50% of adults with recognized depression receive treatment |
| •Reduce deaths caused by motor vehicle crashes | •9.2 deaths per 100,000 population due to motor vehicle crashes |
| •Improve environmental quality | •0% of Americans are exposed to harmful air pollutants |
| •Increase responsible sexual behavior | •0.7 deaths per 100,000 population due to HIV/AIDS |
Oral Health Assessment: Essential in Monitoring Community Health
HIV, Human immunodeficiency virus; AIDS, acquired immunodeficiency syndrome.
To ensure that a comprehensive profile of a community’s health is depicted, oral health should be included in a community health assessment. When the health of a community is assessed, oral health is often found to be an important concern for children, adults, and the elderly.1,2 Common oral and craniofacial diseases and conditions that can be assessed include the following:
Multiple determinants influence oral health in populations.1,3 The etiology and pathogenesis of diseases and disorders affecting craniofacial structures are multifactorial and complex. They involve the interplay among social, cultural, behavioral, environmental, and biologic dimensions.1,3 These factors contribute to the development and progression of oral diseases, conditions, and injuries.1,3 In addition, various factors affect the access of population groups to community preventive services (e.g., community water fluoridation) and clinical dental services. Community preventive services can prevent oral diseases at a community level and improve population oral health. Clinical preventive dental services can prevent oral problems among individuals with access to dental clinics or dental offices. Also, oral health practices and healthy behaviors by individuals can impact oral health outcomes. In a community oral health assessment, it is important to evaluate key determinants that influence oral health status and access to services. Appendix E outlines oral conditions and factors influencing oral health that have been assessed in oral health surveys. The national health objectives outlined in Healthy People provide an important framework for the development of oral health assessments at the state and local levels.
Healthy People
Health promotion and disease prevention are important concepts in the United States. Therefore the nation has developed plans for the prevention of diseases and the promotion of health, embodied in the initiative known as Healthy People.4 These national health objectives shape the health agenda in the United States and guide health improvements. Each decade since 1980, the US Department of Health and Human Services (DHHS) has released a comprehensive set of national public health objectives.4,5 Healthy People provides national 10-year health targets aimed at improving the health of all Americans. It is grounded in the notion that establishing objectives and providing benchmarks to track and monitor progress over time can motivate, guide, and focus action.
The Healthy People initiative has been the nation’s blueprint for disease prevention and health promotion beginning in the 1980s.5 The initiative originated in a 1979 report by the Surgeon General that established the precedent for setting national health objectives and monitoring progress over an interval of a decade.4,5 Healthy People 2000 and Healthy People 2010 set measurable national targets to be achieved by the years 2000 and 2010, respectively.4,5 Healthy People 2020, the fourth generation of national benchmarks, was launched in 2010 and established national objectives to be reached by the year 2020.4
Healthy People 2020 is the outcome of an extensive collaborative process that has relied on input from a diverse array of individuals and organizations, both within and outside the federal government, with a common interest in improving the nation’s health.4,6
The Secretary of Health and Human Services’ Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020 and the Federal Interagency Workgroup (FIW) on Healthy People 2020 guided the development of Healthy People 2020.4,6 The Healthy People 2020 FIW oversaw and managed the development of Healthy People 2020, using input from the Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020 and other Healthy People stakeholders. Representatives from agencies within the DHHS served on the FIW. Federal agencies outside of DHHS also served on the FIW, in support of the Healthy People 2020 framework, which embraces the social determinants of health approach to advanced health improvements.
In addition, the Healthy People initiatives were developed through the involvement of the Healthy People Consortium, a public-private alliance of national organizations and state, territorial, and tribal public health, mental health, substance abuse, and environmental agencies.4,5 These national efforts have brought together national, state, and local agencies; nonprofit, voluntary, and professional organizations; businesses; communities; and individuals to focus on improvements in the health of all Americans. Organizations with an interest in improving oral health have participated actively in the Healthy People Consortium and advocated for oral health to be integrated into the Healthy People initiative.
The national objectives have served as a basis for the development of state and community plans to improve health for three decades.4 Many states and localities have used the Healthy People frameworks to guide the development of health improvement plans and performance standards. Several resources based on the national health objectives have been developed to guide these planning initiatives (see Additional Resources in Chapter 3 and Appendix E).
Healthy People 2020 Framework
The Healthy People 2020 framework consists of a vision statement, mission statement, overarching goals, and graphic model4 (Box 4-1). The framework embraces the determinants of health as an approach to health improvement and promotes the integration of policies that advance health. Also, the framework is informed by a perspective of risk factors as a guide to improvements in health and builds on past iterations of Healthy People. The vision, mission, and overarching goals provide structure and guidance for achieving the Healthy People 2020 objectives. Although the framework is general in nature, it offers a specific focus on important areas of emphasis in which action must be taken if the United States is to achieve better health by the year 2020. The framework provides the foundation for explicit objectives and strategies to attain them. The development process culminated in 2010 with the launch of the national health objectives for 2020 that outlined baseline measures and targets to be reached by 2020. Developed under the leadership of a FIW, the Healthy People 2020 framework is the product of a collaborative process among the DHHS and other Federal agencies, public stakeholders, and the Secretary’s Advisory Committee on Health Promotion and Disease Prevention Objectives for 2020.4
The Healthy People 2020 initiative includes a vision of a society in which all people live long, healthy lives.4 The Healthy People 2020 vision statement outlines the focus for the overall initiative. The mission statement—a framework element that has not been included in previous iterations of Healthy People—is meant to summarize what Healthy People 2020 does for the nation and how the public can use it. It reflects the view that Healthy People 2020 offers practical guidance on using data and knowledge, as well as education and other actions to improve population health in communities.
The overarching goals for Healthy People 2020 provide a general direction for the development of a set of objectives that will measure progress in population health within a specified time period.4 These overarching goals continue the tradition of earlier Healthy People initiatives by advocating for improvements in the health of every person in the country. They address the environmental factors that contribute to collective health and illness by calling for healthy places and supportive public policies, placing particular emphasis on the determinants of health.
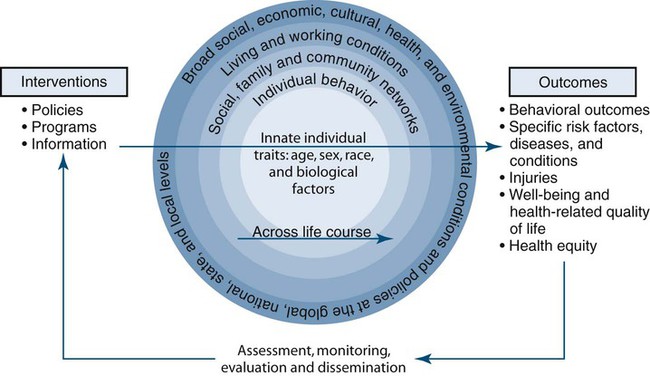
The Action Model to Achieve Healthy People 2020 Goals is graphically displayed in Box 4-1. The figure shows a feedback loop of intervention, assessment, and dissemination that would enable achievement of the Healthy People 2020 overarching goals.4 Also, this figure illustrates the Institute of Medicine’s (IOM) model of the multiple determinants of health. The model is represented by an inner circle and four outer circles. Within the innermost circle are innate individual traits: age, sex, race, and biologic factors related to the biology of health and disease. The first circle outside the center circle represents individual behavior; the next circle represents social, family, and community networks; and the next circle represents living and working conditions. The figure defines living and working conditions as including psychosocial factors, employment status and occupational factors, socioeconomic status (e.g., income, education, occupation, etc.), the natural and built environments, public health services, and health care services. The built environment includes transportation systems, water and sanitation systems, housing, and other dimensions of community planning. The outermost circle represents broad social, economic, cultural, health, and environmental conditions and policies at the global, national, state, and local levels. Social conditions include economic inequality, urbanization, mobility, cultural values, attitudes, and policies related to discrimination and intolerance on the basis of race, gender, and other differences. Other conditions at the national level include major sociopolitical shifts such as recession, war, and governmental collapse.
The figure displays an action model showing the impact of interventions (e.g., policies, programs, and information) on the determinants of health at multiple levels across the lifespan to achieve the overarching goals of Healthy People 2020.4 Results of such interventions are demonstrated through assessment, monitoring, and evaluation. Through application of evidence-based practices, the findings can be used to inform intervention planning and implementation of effective strategies.
Healthy People 2020 Focuses On Eliminating Health Disparities And Promoting Health Equity
Eliminating health disparities and promoting health equity is a focus of Healthy People 2020 and requires actions to address all important determinants of health disparities that can be influenced by institutional policies and practices.4 Disparities can include disparities in health care but also in other health determinants, such as living and working conditions, as well as social, economic, cultural, community, and environmental conditions that are needed for health. Social policies related to education, income, transportation, and housing are powerful influences on health because they affect factors such as the types of foods that can be purchased, the quality of the housing and neighborhoods in which individuals can live, and access to quality education and health care.
The concepts of health equity and health disparity are inseparable in their practical implementation. Policies and practices aimed at promoting the goal of health equity do not immediately eliminate all health disparities, but they can provide a foundation for moving closer to that goal. There are a variety of definitions of health disparity and health equity. The Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020 defined theses terms for the purposes of Healthy People 2020.4
The general public usually understands the term health disparity as referring to any difference in health. However, in the public health community and as defined by the Advisory Committee, the term refers to a particular type of health difference between individuals or groups that is unfair because it is caused by social or economic disadvantage. A health disparity is a particular type of health difference that is closely linked with social or economic disadvantage. Health disparities adversely affect groups of people who have systematically experienced greater social or economic obstacles to health based on their racial or ethnic group, religion, socioeconomic status, gender, mental health, cognitive, sensory or physical disability, sexual orientation, geographic location, or other characteristics historically linked to discrimination or exclusion.4
Health equity is a desirable goal and standard that entails special efforts to improve the health of those who have experienced social or economic disadvantage.4 The Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020 states the following requirements are needed for health equity: (1) continuous efforts focused on elimination of health disparities, including disparities in health care and in the living and working conditions that influence health, and (2) continuous efforts to maintain a desired state of equity after particular health disparities are eliminated.4 Health equity is oriented toward achieving the highest level of health possible for all groups. The Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020 recommended the following short- and long-term actions to achieve health equity:
• Particular attention to groups that have experienced major obstacles to health associated with being socially or economically disadvantaged.
• Promotion of equal opportunities for all people to be healthy and to seek the highest level of health possible.
• Distribution of the social and economic resources needed to be healthy in a manner that progressively reduces health disparities and improves health for all.
• Attention to the root causes of health disparities, specifically health determinants, a principal focus of Healthy People 2020.
National Objectives for Improving Health
The national health objectives developed for Healthy People over the years have called for action to promote healthy behaviors and healthy and safe communities; improve systems for personal health and public health; and prevent diseases, injuries, disabilities, and disorders.4–6 Healthy People 2010 contained 467 objectives, grouped in 28 focus areas; each focus area had a specific overall goal.5 Also, ten Leading Health Indicators were designated in Healthy People 2010 as key measures for national report cards on population health.5
Healthy People 2020 continues the mechanisms for monitoring and tracking health status, health risks, protective factors, and use of services.4,6 The Healthy People 2020 Health Objectives integrate the determinants of health that encompass the combined effects of individual and community physical and social environments. Also, the objectives consider policies and interventions used to promote health; prevent diseases, injuries, and disabilities; and ensure access to effective personal and public health services. The ultimate measure of success in any health improvement effort will be gains in health status of specific populations.
Thirty-eight topic areas have been proposed for Healthy People 2020.6 The proposed Healthy People 2020 National Health Objectives were developed by Topic Area Workgroups led by various agencies within the Federal government.6 They were reviewed by the FIW on Healthy People 2020.6 The final set of Healthy People 2020 objectives were developed with input from public comments collected at public meetings and in writing via a public comment website.6 Also, the final national health objectives for 2020 were refined through further deliberations of the Topic Area Workgroups, FIW on Healthy People 2020, and Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020.
National Oral Health Objectives
The national oral health objectives have defined the nation’s oral health agenda and served as a road map for national benchmarks since the early 1980s. Oral health is a specific topic area in Healthy People 2020.4 Also, oral health is integrated into other topic areas in the Healthy People 2020 Objectives for the nation.
Table 4-1 summarizes the topics included in Healthy People 2010 Oral Health Objectives and the proposed Healthy People 2020 Oral Health Objectives. Table 4-2 outlines selected health objectives with related oral health topics from those proposed in Healthy People 2020. Also, Appendix D provides additional information about measure used to monitor the objectives and the key data sources.
Table 4-1
Healthy People 2010 and 2020: Oral Health Objectives
Healthy People 2010 oral health goal: To prevent and control oral and craniofacial diseases, conditions, and injuries and improve access to related services.
| Healthy People 2010 National Health Objective Number (Healthy People 2020 Proposed National Health Objective Number)* | Topic of Healthy People 2020 Proposed National Health Objective† |
| HP2010–21-1 (OH HP2020–6) | Reduce dental caries experience |
| HP2010–21-2 (OH HP2020–7) | Reduce untreated dental decay |
| HP2010–21-3 and HP2010–21-4 (OH HP2020–8) | Reduce permanent tooth loss and complete tooth loss |
| HP2010–21-5a | Reduce periodontal disease: Gingivitis (2010 objective achieved not included in Healthy People 2010) |
| HP2010–21-5b (OH HP2020–9) | Reduce periodontal disease: Destructive periodontal disease |
| HP2010–21-6 (OH HP2020–1) | Early detection of oral and pharyngeal cancers |
| HP2010–21-7 (OH HP2020–16) | Increase annual examinations for oral and pharyngeal cancer |
| HP2010–21-8 (OH HP2020–10) | Increase dental sealants |
| HP2010–21-9 (OH HP2020–2) | Increase community water fluoridation |
| HP2010–21-10 (OH HP2020–3) | Increase use of oral health care system |
| HP2010–21-11 (OH HP2020–11) | Increase use of oral health care system by residents in long-term care facilities |
| HP2010–21-12 (OH HP2020–4) | Increase dental services for low-income children |
| HP2010–21-13 (OH HP2020–12) | Increase school-based health centers with oral health component |
| HP2010–21-14 (OH HP2020–13) | Increase local health departments and Federally Qualified Health Centers (FQHCs) with an oral health component |
| HP2010–21-15 (OH HP2020–14) | Increase number of states and the District of Columbia with a system for recording and referring infants and children with cleft lips and cleft palates to craniofacial anomaly rehabilitative teams |
| HP2010–21-16 (OH HP2020–5) | Increase number of states and the District of Columbia with an oral and craniofacial health surveillance system |
| HP2010–21-17 (OH HP2020–15) | Increase the number of health agencies that have a public dental health program directed by a dental professional with public health training |
| Newly proposed Healthy People 2020 oral health objective (OH HP2020–17) | Increase patients that receive oral health services at Federally Qualified Health Centers each year |
*Numbers refer to the chapter and objective as referenced in Healthy People 2010. For example, 21-12 is Chapter 21, Objective 12. Numbers in parentheses refer to objective as referenced in Proposed Oral Health Objectives for Healthy People 2020. For example, OH HP2020-14 is Chapter 1, Proposed Objective 14 in the oral health chapter in Healthy People 2020.
†The Healthy People 2020 health objectives were proposed; see the Healthy People 2020 website for the final objectives to be achieved by 2020.
Adapted from Department of Health and Human Services (DHHS). Healthy People 2020: Public Meetings 2009 Draft Objectives. Washington, DC: DHHS; 2009. Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington, DC: DHHS; 2000.
Table 4-2
Healthy People 2010 and 2020: Selected Health Objectives Related to Oral Health
| Healthy People 2010 National Health Objective Number (Healthy People 2020 Proposed National Health Objective Number)* | Topic of Healthy People 2020 Proposed National Health Objective† |
| Access to Quality Health Services: HP2010–1-6 (Access to Health Services: AHS HP2020–7) | Reduce individuals experiencing difficulties or delays in obtaining necessary medical care, dental care, or prescription medicines |
| Access to Quality Health Services: HP2010–1-8 (Public Health Infrastructure: PHI HP2020–11) | Increase degrees awarded in the health professions to members of underrepresented racial and ethnic groups, including dentistry |
| Cancer: HP2010–03-6 (Cancer: C HP2020–6) | Reduce oropharyngeal cancer deaths |
| Cancer: HP2010–3-10 a, b, c (Tobacco Use: TU HP2020–17) | Increase tobacco cessation counseling in health care settings, including in dental care settings |
| Newly Proposed Healthy People 2020 Health Objective Tobacco Use: TU HP2020–19 | Increase tobacco screening in health care settings, including dental care settings |
| Diabetes: HP2010–05-15 (Diabetes: D HP2020–9) | Increase annual dental examination for persons with diabetes |
| Newly Proposed Healthy People 2020 Health Objective Educational and Community-Based Programs: ECBP HP2020–12 | Increase number of preschools and Head Start programs that provide health education to prevent health problems, including unintentional injury; violence; tobacco use and addiction; alcohol and drug use, unhealthy dietary patterns; and inadequate physical activity, dental health, and safety |
| Newly Proposed Healthy People 2020 Health Objective: Older Adults: OA HP2020–6 | Increase health care workforce with geriatric certification, including dentists |
*Numbers refer to the chapter and objective as referenced in Healthy People 2010. For example, 03-6 is Cancer Chapter 3, Objective 6. Numbers in parentheses refer to objective as referenced in Proposed Oral Health Objectives for Healthy People 2020. For example, Cancer: C HP2020–6 is Cancer Chapter 6 and Proposed Objective 6 for Healthy People 2020.
†The Healthy People 2020 health objectives were proposed; see the Healthy People 2020 website for the final objectives to be achieved by 2020.
Adapted from Department of Health and Human Services (DHHS): Healthy People 2020: Public Meetings 2009 Draft Objectives. Washington, DC: DHHS; 2009. Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington, DC: DHHS; 2000.4
Oral Health Surveillance Systems
A comprehensive public health surveillance system integrates oral health and is essential for programmatic activities to improve oral health. Several agencies and national organizations have stressed the importance of oral health surveillance systems to routinely collect data on oral health outcomes, risk factors, and intervention strategies for the whole population or representative samples of the population.7,8 Oral health surveillance systems are not only oral health data collection systems but also involve timely communication of oral health findings to responsible parties and to the public. Also, it involves using oral health data to initiate and evaluate public health measures to prevent and control oral diseases.7,8 An oral health surveillance system should contain at a minimum a core set of oral health measures that describe the status of important oral health conditions to serve as benchmarks for assessing progress in achieving oral health improvements.
Steps have been taken in the United States at the national, state, and local levels to formulate a systematic approach for oral health data collection and reporting. The focus of these collaborative efforts among organizations and agencies was to promote oral health assessment and monitoring that could be applied in a wide range of environments. These efforts also stressed the importance of oral health program evaluation in light of contemporary public health principles. An important aim of these efforts has been the dissemination of procedures for collecting comparable data to assess oral health. A long-term goal includes an approach for continuous monitoring of oral health at the national, state, and community levels, as well as an expansion of indicators in oral health surveillance systems. Results of these endeavors included the development of standard ways to monitor the national oral health objectives, an oral health needs assessment model, and documentation of uniform methods to measure community oral health.7–13 Several resources have been developed to provide guidance to national, state, territorial, tribal, and local oral health programs in planning and implementing oral health surveillance systems.
The Association of State & Territorial Dental Directors (ASTDD) has developed and updated several resources that provide guidance on oral health surveillance. The ASTDD has developed a best practices report that provides a review of oral health assessment measures, methods, and standards.8 The Basic Screening Survey (BSS) has established standards for oral health screenings for preschool and school children.9 The ASTDD has also developed the BSS for assessing oral health among adults and elderly individuals.
The National Oral Health Surveillance System (NOHSS) is an important oral health data system. NOHSS is a collaborative effort between the Centers for Disease Control and Prevention (CDC), Division of Oral Health, and the ASTDD. It is designed to help public health programs monitor the burden of oral disease, use of the oral health care delivery system, and status of community water fluoridation on both a state and a national level. NOHSS includes indicators of oral health from national and state data sources, information on state oral health programs, and links to sources of oral health information. NOHSS has been developed to track basic oral health indicators.8 NOHSS includes a minimal set of standard oral health indicators, to be expanded in the future, based on data sources and surveillance capacity available to most states. A functioning state oral health surveillance system should enable the state to submit data for inclusion in the NOHSS. Box 4-2 outlines the indicators currently included in NOHSS.8
The Dental, Oral, and Craniofacial Data Resource Center (DRC) is another important source of information for oral health surveillance and oral health assessments. The DRC is cosponsored by the National Institute for Dental and Craniofacial Research (NIDCR), National Institutes for Health (NIH), and the Division of Oral Health, CDC. The DRC serves as a resource on dental, oral, and craniofacial data for oral health educators, researchers, clinical practitioners, public health planners, policymakers, advocates, and the general public. Key resources related to oral health assessment are available from the DRC and include the (1) Catalog of Oral Health Surveys and Archive of Procedures Related to Oral Health and (2) Oral Health Survey Questions: A Compilation of Dental and Oral Health Questions Included on National Health Surveys. Appendix D includes information on the NOHSS, DRC, and other oral health data systems and data sources.
Measuring Oral Health and Its Determinants in Populations
This chapter focuses on measurements of oral health used in population-based oral health surveillance systems and oral health surveys. The text highlights common measures used to assess population oral health, specifies oral health indicators included in Healthy People 2010 and 2020, and provides an overview of clinical and nonclinical data collection methods related to oral health assessment. Measures and methods used for assessment of individual patients in clinical settings or in clinical studies (including clinical trials) are not emphasized in this chapter. Other books review clinical evaluation techniques or clinical research methods.14
1. Information of interest (e.g., types of conditions and factors to be assessed)
2. Social and demographics of the population and community
3. Purpose of the assessment (e.g., how data collected are to be used after assessment)
Common nonclinical measures include face-to-face personal interviews, telephone interviews, a self-administered questionnaire, and a computer-assisted personal interview, although other nonclinical methods can be used to assess different factors influencing oral health.11 The topics of oral health questions that can be used in oral health surveys are outlined in Appendix E.
Clinical methods include basic screenings and epidemiologic examinations.9,11,12,15,16 Basic screenings involve the use of direct observation techniques established for visual detection and identification of gross dental and oral lesions in the oral cavity with a tongue blade, a dental mirror, and appropriate lighting. Epidemiologic examinations entail the use of detailed visual-tactile assessment of the oral cavity with dental instruments and a light source in an oral health survey.
Basic screenings and epidemiologic examinations do not constitute a thorough clinical examination9,11; they do not involve making a clinical diagnosis that would result in a treatment plan. Surveys are cross-sectional when they look at a population at a point in time. Surveys are descriptive because they allow for oral health determinants to be ascertained and oral health status to be estimated for a defined population.
Common dental indexes are used for clinical measures in oral health surveys. A dental index is an abbreviated measurement of the amount or condition of oral disease in a population. An index is based on a graduated numeric scale with defined upper and lower limits. It is an aid in data collection, allowing for comparisons among population groups that are classified by the same criteria and methods. The attributes of a good index are reviewed in Box 4-3.
Types of Measurements
Measurements of Dental Caries
Permanent Dentition
Dental caries can occur in primary or permanent teeth. General types of tooth decay include coronal (occurring on the crowns of teeth) and root surface (occurring on the roots of teeth). In surveys of populations, coronal and root surface caries can be assessed by a systematic evaluation through epidemiologic examination or screening procedures.9,12,15–20 The status of decayed, missing, and filled teeth (DMFT) or decayed, missing, and filled surfaces (DMFS) is commonly recorded by a basic screening or oral epidemiologic examination.9,12,15,16
The conventional decayed, missing, and filled (DMF) Indexes are used to count coronal caries of permanent teeth (DMFT) or surfaces (DMFS). Although the DMF Index has been used extensively in oral health surveys and has been a standard measurement in many countries, it is limited in its ability to measure thoroughly the characteristics of dental caries.15,16 As patterns of dental caries change, technology develops, and the goals of oral health surveys shift toward more situational analyses in communities, different approaches for the measurement of dental caries may emerge in the future.9,11,20
For the DMF Index, each tooth space is scored as to whether it is sound or is diseased and whether there is evidence of treated or untreated clinical caries.18,19 The DMF Index can be based on 28 or 32 permanent teeth in surveys of population. If ever diseased, the tooth must show one of three conditions:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses