Chapter 4
Material Considerations. Which Material Today Doctor?
Aim
Practitioners are frequently uncertain as to which material to use in a given clinical situation. The aim of this chapter is to give the practitioner clear guidelines as to the situations in which dental materials can be used to both the patient’s and operator’s best advantage. The science behind the materials will only be discussed where it relates to the use of the material. Readers are referred to textbooks on dental materials for more detailed information.
Outcome
On reading this section practitioners will be familiar with the dental materials currently recommended for use in contemporary operative dentistry along with their respective advantages, disadvantages, indications and contraindications for use.
Introduction
There continues to be uncertainty as to which materials practitioners should use to achieve predictable results when direct restorations are being placed. This situation is not helped by materials being subject to constant change and with new materials often introduced with little information in the form of data from well-conducted clinical trials to assist practitioners in making informed decisions.
There is a move towards greater use of tooth-coloured direct restorative materials, which many believe has largely been driven by patient demand. Generally, the results achieved with these materials have been suboptimal. This is probably due to one or more of the following:
-
lack of appropriate instruction
-
incorrect material selection
-
inappropriate clinical use – for example, using resin composite as a “white” amalgam
-
not using the materials according to the directions for use especially with respect to curing depth, time of cure, application of dentine-bonding agents and with inadequate moisture control at placement
-
aggressive finishing and a lack of in-service maintenance.
To assist practitioners in making appropriate decisions when selecting materials, it is helpful to review the materials currently available. The following materials and their principal advantages, disadvantages, indications and contraindications will be considered in the following section:
-
amalgam
-
resin composite
-
compomers
-
resin-modified and traditional glass ionomer cements
-
ormocers
-
giomers.
Common problems associated with the use of these materials and how these can best be avoided will also be addressed. It is to be remembered that no restorative material is ideal, let alone universal.
Amalgam
Introduction
Amalgam has a proven longevity with over 160 years of clinical use. Systematic reviews have claimed that amalgam has both a low cost coupled with improved longevity when compared with other materials, especially resin composite. The validity of these reviews has been questioned because the research on which these conclusions have been based relates to outdated formulations of resin composites placed using techniques that are now deprecated. Developments in the clinical application of resin composites and simultaneous developments in dentine bonding systems have shortened treatment times considerably, making the conclusions of these reviews less meaningful. Concurrently, research has also demonstrated improved longevity for resin-composite restorations above that of similar-sized amalgam restorations. There is no doubt that amalgam is a low-cost restorative material, which performs well in large preparations in premolar and permanent molar teeth, especially under occlusal loading. It is also apparent that most practitioners can readily and speedily use amalgam to good effect. Patients, however, whose needs and expectations are paramount, are increasingly dissatisfied with the continuing routine use of amalgam.
Advantages
The advantages of amalgam include:
-
Ease of placement.
-
Low technique sensitivity.
-
Durable material with low wear rate.
-
Low cost.
-
Proven longevity.
Disadvantages
Amalgam has many disadvantages as a restorative material, notably:
-
It is not tooth coloured.
-
Undercut is required to retain the restoration (although amalgam can be bonded to teeth with dentine-bonding agents, which can reduce the need for undercuts). Bonded amalgams have proven longevities of up to two years but are much more expensive to place. It is suggested, therefore, that bonded amalgams have a place in complex or compound preparations in permanent molar teeth where the placement of dentine pins may be avoided.
-
The need for undercut and to remove all unsupported enamel makes preparations for amalgam restorations necessarily more destructive of tooth tissue. Consequently, amalgam cannot be recommended for the initial management of lesions of caries and where minimal intervention is indicated.
-
It is difficult to manipulate to good effect in conservative preparations.
-
There is the possibility of lichenoid reactions when amalgam restorations have intimate frictional contact with adjacent mucosa – for example, cervical restorations in lower permanent molar teeth.
Indications
Amalgam is currently recommended in the following situations:
-
Large compound or complex preparations in permanent molar teeth. Should additional retention be required it is preferable to bond the amalgam and/or use boxes, slots or circumferential grooves in preference to the use of dentine pins (a pin having been shown inherently to weaken the restored unit). It is likely that teeth with such extensive coronal damage are better restored with an adhesive core material rather than amalgam, followed by a full-coverage restoration such as a gold shell crown.
-
Repair of fractured amalgam restorations where repair is not feasible with an adhesive material.
-
As a core material – specifically as a Nayaar core in non-vital teeth – although research would seem to suggest that tooth-coloured restorative materials are equally effective in this clinical situation.
Contraindications
Current recommendations suggest that amalgam should not be used in the following situations:
-
Initial lesion management where minimal operative intervention is indicated.
-
In small to moderate occlusal or proximal preparations in premolar and permanent molar teeth where an adhesive material would be more appropriate (Fig 4-1).

Fig 4-1 Distal aspect of 44 restored with amalgam where resin composite was indicated.
-
Large occlusal and proximal preparations in premolar teeth.
-
All cervical restorations.
-
For retrograde root canal therapy.
-
In pregnant women.
It is suggested that the continued use of amalgam is difficult to justify in other than large preparations in posterior teeth where cusp replacement is required and a direct restoration is indicated.
Resin Composite
Introduction
These materials are a composite of glass filler particles in a resin matrix. There are many classification systems for resin composites but the system based on glass filler particle size is the most widely used. Manufacturers seem to have accepted that the concept of a universal resin composite is flawed and that resin composites for anterior and posterior use require different properties. Consequently, there is a trend away from universal resin composites.
Materials with a higher fillerresin ratio are recommended for the restoration of posterior teeth whilst materials with more resin matrix at the expense of filler particles have been developed for the restoration of anterior teeth. This is because materials with a higher filler:resin ratio tend to be stronger, more wear resistant and shrink less when cured. A high concentration of filler particles, however, makes the materials more opaque, less vital in appearance and more difficult to polish. Conversely, materials with higher filler: resin particle ratios are more easily polished and translucent. Such materials, however, shrink more when cured.
To identify suitable materials for anterior and posterior use, practitioners are advised to look for information that relates to the percentage filler load by volume. Materials that have greater than 60% filler by volume are more suitable for the restoration of posterior teeth, whilst those below 60% filler by volume are recommended for anterior use. Manufacturers will often quote percentage filler by weight for materials, which is misleading because filler particles weigh more than the resin component. For example, a material that is 72–75% filler by weight might only be 60% filler by volume. The extent of polymerisation curing contraction is directly related to the percentage of resin in the material by volume not weight. However, several other factors are important, particularly the monomers incorporated and their specific structures and extent of cure.
Curing strategies for resin composites
Considerable research has gone into developing new resin systems with low shrinkage when cured. To date, none of this research has brought a material to the profession that has a significantly reduced polymerisation contraction when cured. It is important to recognise, therefore, that all resin systems contract on curing and that steps must be taken when placing these materials to reduce the clinical consequences of this contraction.
Currently, the majority of practitioners use a halogen bulb-based light-curing unit for photocuring resin composites. There is evidence that the maintenance of curing lights is poor, with light output in poorly maintained units being below that required: typically 400mw cm-2 to cure a composite adequately. Light output is reduced by debris on the light curing tip, ageing of the halogen bulb and fogging or damage to the light limiting filters. It has been shown that 25% of light-curing units have a light output below that required to cure a resin composite to an adequate depth. It is good practice therefore to check the output of the light from time to time and have the units regularly serviced (Fig 4-2). Some lights are available which can compensate for an ageing bulb. It is necessary to clean and autoclave the light-curing tip after each patient or to use a disposable sleeve.
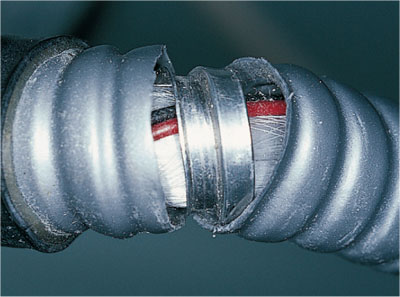
Fig 4-2 Fractured lead of halogen-based curing light still in use. A considerable proportion of the light output is lost from the lead.
A modification to the conventional light curing of resin composites was introduced recently. The concept known as “ramped” or “soft-start” polymerisation has been shown to produce better marginal adaptation, which might lead to reduced interfacial marginal leakage. It has also been suggested that the net overall shrinkage of resin composites cured with this method is less. The system works by providing a variable light output, which increases typically from 100mw cm-2 to 400-800mw cm-2 over a 40-second period (Fig 4-3). The low initial output allows for the material to reach a gel stage whereby the material can reorganise along its molecular planes accommodating initial shrinkage stress within the body of the material.
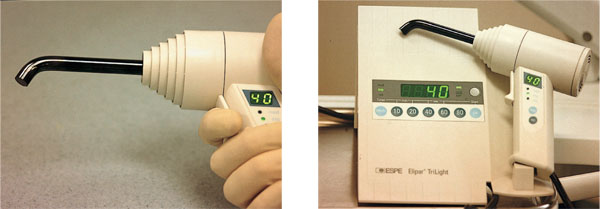
Fig 4-3 Halogen-based curing light with ramped curing mode.
Faster curing strategies (for example, plasma-curing lights) designed to reduce shrinkage and increase depth of cure have not been demonstrated to have a significant benefit over more conventional curing strategies. Concerns have been expressed about heat generation during plasma light curing in addition to the exotherm when any resin composite polymerises, depth of cure and residual monomer post curing. It has been suggested, however, that polymerisation shrinkage is less with these lights. There is not enough evidence currently to suggest that these lights confer any advantage over a conventional halogen-based curing system, let alone a soft-start halogen-based curing light. Consequently, it is currently not possible to recommend their use.
New curing lights based on light-emitting diode (LED) technology are now available to practitioners and these look promising (Fig 4-4). The benefits of these systems are reported to be as follows:
-
More energy efficient with no heat generated.
-
They are quieter because no fan is needed for cooling.
-
The machines are cordless, smaller and lighter.
-
Depth of cure is greater than with halogen lamps.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


