CHAPTER 4
Managing the Developing Occlusion
Thumb/Finger Sucking
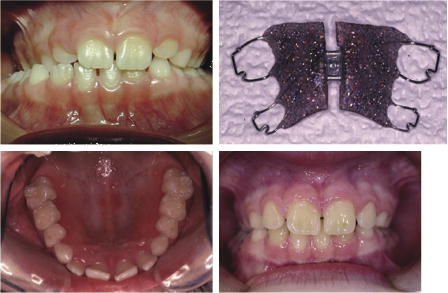
Thumb/finger sucking can cause significant distortion of the dental arches. The severity of this is related to the amount of time spent digit sucking each day and the method and intensity with which the individual sucks (Warren et al., 2005). It has been reported that up to 70% of 10-year olds have a digit sucking habit and that two-thirds of these can end up with a serious malocclusion as a result. Studies have shown that the main effects of a persistent habit can include a reduced overbite or mild anterior open bite, and a mild tendency to proclination of the upper incisors with tendency to mild posterior crossbites as a result of the negative pressure produced by the sucking. More serious effects, such as an asymmetric open bite or severe posterior crossbites are much rarer (Figures 4.1 and 4.2) (Popovich, 1966; Mitchell, 2000; Patel, 2008; Mistry et al., 2010). These effects can be socially unacceptable and difficult to treat if left to establish in the permanent dentition.


There are a number of options to intercept the distortion effects of a digit habit, but children younger than 6 years of age are rarely able to cope with appliance treatment. Cognitive behavioural management with reward charts designed to reward ‘good’ rather than ‘punish’ bad behaviour are the interceptive measures of choice in the younger patient. If this has not been effective by 7 years of age, more definitive treatment is required and appliance therapy should be considered to ensure that arch distortion or displacement of the developing incisors does not occur. Simple measures such as nail paint, putting gloves on or finger/thumb splints can be used to deter the habit in patients who actively wish to give up. Appliance wear however can not only deter the habit, but can also be used to address other occlusal problems such as crossbites or overjet and overbite issues. For those who have a significant sagittal discrepancy, a functional appliance can be used to combine a deterrent with Class II correction. Unfortunately, any removable appliance can easily be removed at times when the urge to suck a digit is at its greatest (such as sitting in front of the TV or on long car journeys) and therefore is much less effective than an appliance that cannot be removed. The only true preventative appliance is the fixed thumb guard (Figure 4.3).
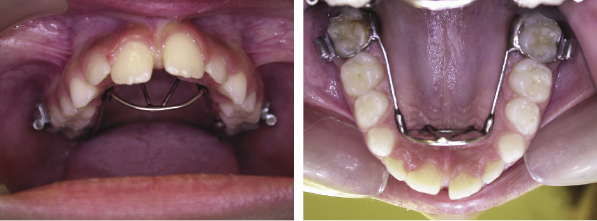
The fixed thumb guard ensures full compliance and is well tolerated. The wirework must be large enough to ensure the digit cannot be put into the mouth, thus forcing an immediate cessation of the habit, and it must be very well polished so that there is no trauma to the tongue. All habits are individual and there cannot be any general rule as to the period of wear; however, it is reasonable for these appliances to be left in situ for at least 6 months to ensure the habit is broken (Figure 4.4).
Fixed orthodontic expansion appliances, such as the Quadhelix, can also be used to incorporate arch expansion, but they are not as effective as a thumb guard as they do not physically stop the thumb from being put in the mouth (Figure 4.5). The design of these appliances should be modified so that the anterior wires act as a thumb guard.

Crowding of the Permanent Lateral Incisors
A common early presentation of crowding is a lack of space for the development of the permanent lateral incisors. Delaying orthodontic treatment until all the permanent teeth have erupted may mean that these permanent teeth become rotated or displaced palatally, or even impacted, due to the lack of space (Figure 4.6).

Early extraction of the primary canines to create space to guide the eruption of these teeth has little evidence base; however, this approach can be justified if the consequences of the crowding for the patient are appreciated. If there is a shortage of space for the eruption of the permanent lateral incisors, it is certain that they will be displaced from their ideal position and orthodontic treatment will be necessary later. If they erupt rotated or displaced, the periodontal fibres form in these poor positions. Once the tooth position is corrected with orthodontic treatment, the fibres have to reorientate to stabilise the tooth. This takes a long time and often is incomplete, leading to the high probability of relapse of the tooth position or protracted retainer wear. More importantly, in today’s society poor aesthetics is not tolerated and may cause psychological issues for the child with regard to self-esteem or lead to teasing at school.
Early extraction of primary canines to prevent centre-line shift is also indicated if one primary canine is lost early. For the best outcome the teeth should be removed before the permanent lateral incisors have erupted.
It must be understood that interceptive extractions will not eliminate crowding of the permanent dentition. In fact, they may make it worse as the lateral incisors will drift distally in the arch as they erupt. Early deciduous extraction is based on the premise that crowding of these teeth implies that there is a dento-alveolar disproportion and that extraction of a permanent unit in each quadrant is almost inevitable at a later date. This will normally be a premolar (usually the first premolar); however, exceptionally, it can be the permanent canine if this is ectopic, or indeed any other compromised tooth.
The great advantage of this interceptive approach is that anterior aesthetics is maintained throughout the establishment of the permanent dentition and the permanent teeth are guided into the dental arch form. This reduces the length of time of the later comprehensive orthodontic treatment in the established permanent dentition.
Other methods of inclusion of the lateral incisors will depend on the amount of crowding and the upper arch width. If there is minor crowding and an element of maxillary narrowness tending toward crossbite, upper arch expansion can be considered. The buccal segments should never be expanded into a buccal crossbite, but correcting posterior crossbites (with or without a displacement) to correct the arch shape and create space for the inclusion of all the adult dentition is valid (Figure 4.7).
Great care must be taken to ensure that the correct interdigitation of the buccal segments is maintained, and even if it is, long-term retention of this expansion will be required. However, in reality the whole argument about the importance of buccal segment interdigitation in retaining arch expansion has to be challenged, as teeth are rarely together when at rest as there is a freeway space between the upper and lower dentition. The only time the teeth are in contact is during biting or tooth clenching and this amount of time cannot maintain the tooth position. It is much more likely that mild maxillary asymmetries are due to developmental moulding or tongue position.
If there is no buccal crossbite, expansion is not warranted and extraction of the primary canines or disking of them to create space for the lateral incisors to erupt is the treatment of choice. Choosing whether to undertake expansion of the arch or extraction of the teeth depends on a careful assessment of the patient. This will include radiographic examination with an orthopantogram (OPG), an assessment of the amount of crowding of the anterior teeth, the shape of the dental arch and the posterior occlusion, as well as consideration of the wishes of the child and their parents. The ability of the child to accept a tooth extraction without being traumatised is also an important part of the treatment planning process. Good oral hygiene is an advantage and both the child and their parents must understand the long-term commitment to treatment and the possibility of further extractions and comprehensive orthodontic treatment at a later stage. This non-appliance approach is also particularly useful if no orthodontic treatment is contemplated or possible due to medical or physical factors, or even when compliance with oral hygiene is poor. The non-appliance guiding of the adult teeth into the line of the dental arch will usually give reasonable aesthetics without the need for complex orthodontic treatment.
Where there is little crowding but anterior spacing is leading to a lack of appropriate space for the developing secondary teeth, a short course of fixed appliance treatment to gather space in the upper labial segment can also have beneficial effects on the eruption of the secondary dentition (Figure 4.8).
Anterior Crossbites
Anterior crossbites should be treated early to avoid periodontal damage, fenestration of the lower labial plate due to incisor displacement, tooth wear due to abnormal contact or mandibular displacement and the potential for temporomandibular joint (TMJ) dysfunction (Figures 4.9, 4.10 and 4.11). It is important to remember that the correction of anterior crossbites needs bite opening to avoid compensatory movement of the opposing teeth and therefore, bite planes may need to be used. As a removable appliance causes tipping movements of the teeth, it is preferable to begin correction of the crossbite early whilst the offending tooth is erupting as this takes advantage of the vertical movement of the tooth during treatment, which allows a better vector of movement of the tooth with the appliance during tooth eruption. If the tooth has fully erupted, further tipping will be required to correct its position. Once the tooth is in the correct position with a positive overbite, the bite blocks can be removed from the appliance as the crossbite will be self-retaining (Figures 4.12 and 4.13). It is important to ensure that adequate space is available for the labial movement of the tooth in crossbite. If there is no distal space for the teeth either side of the tooth in crossbite to be moved into, deciduous extractions will be necessary.





Occasionally, a crossbite can be corrected by extraction alone (Figure 4.14).

Posterior Crossbites and Guidance of the Secondary Dentition
Expansion of the posterior teeth is a contentious subject. There is little evidence to confirm that early expansion in the absence of a crossbite will create enough space for the permanent teeth to develop into and improve the arch form, or that a crossbite is damaging to dental or TMJ health. However, if a number of features are present, such as a crossbite, displacement and asymmetrical dental arch form, expansion has the potential to guide the developing secondary dentition and, in cases with mild crowding, of eliminating the need for extractions by producing a symmetrical dental arch.
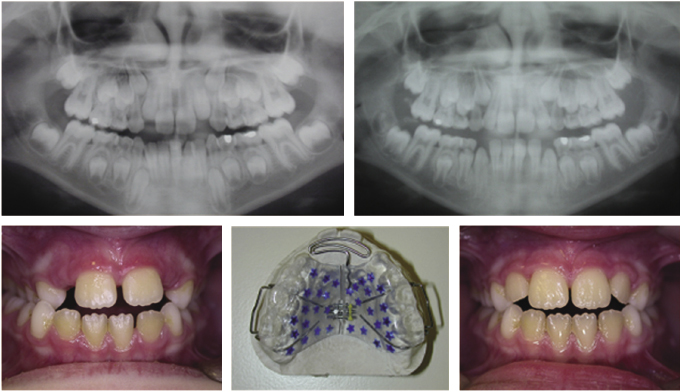
Before embarking on expansion, careful assessment of an OPG is required. Although an accurate space analysis cannot be done from a tomograph, a rough space assessment can be done by measuring the space between the distal edge of the lateral incisor and first permanent molar (including an assessment of any anterior spacing that can be used to accommodate the teeth) and comparing this with the combined crown widths of the canine and both premolars. The difference will give a good idea of whether the crowding is mild, moderate or severe. Careful assessment of the OPG will also rule out the presence of hypodontia or supernumerary teeth, which may significantly influence early deciduous arch guidance.
Posterior expansion can be done with a removable or fixed appliance (Figures 4.15 and 4.16), but care must be taken to ensure the bite is opened with posterior bite blocks on removable appliances, or Glass Ionomer cement placed on the teeth when using a Quadhelix appliance to avoid compensatory expansion of the lower arch due to the cuspal interlock. Appliances should be worn full-time during the active phase and for at least 6 months afterwards to allow the arch dimension to stabilise. It is usually preferable to use a fixed appliance rather than a removable one as compliance is guaranteed if the appliance cannot be removed by the patient. This treatment works well for arches where the crossbite is due to dental or dento-alveolar malposition. When the crossbite is skeletal in origin, expansion of a narrow maxilla will not be stable.

A number of practitioners take the view that arch expansion should be undertaken in most circumstances to accommodate all the permanent teeth. They claim that this approach will give a broad arch that is both aesthetic and functional. However, there is no respected evidence to confirm this and no long-term studies that demonstrate that arch expansion will be stable if there is intrinsic dento-alveolar disproportion. When expansion is done in these circumstances, long-term or even life-long retention is required. For an adult who is looking for a specific aesthetic solution, this may not be unreasonable, but for a child, expansion of the maxillary arch (when there is no crossbite) often requires concomitant expansion of the mandibular arch. Without clear soft tissue factors indicating that this is advisable, long periods of retainer wear will be required, which is an unrealistic expectation for a child.
There is a need for a period of retainer wear after most orthodontic tooth movements. The important question is how long is it reasonable to expect a child to wear a retainer. Commitment to retainer wear must be part of informed consent, but expanding the dental arches in the knowledge that they will be unstable or expecting that the soft tissues or skeletal bases will expand with the dental movements is bad practice. It is of course impossible on an individual basis to assess this, but the greater the expansion the more likely it is that it will relapse. As in all orthodontic treatment planning, there are guidelines but very little absolute evidence on which to base specific practice. A full discussion with the patient, a cautious approach and excellent mechanics is the most likely recipe for success.
Serial Extraction: a Modern Approach
Serial extraction was introduced in the 1940s to guide the developing dentition at a time when orthodontic appliances did not easily allow precise tooth movement. Its practice fell out of favour with the introduction of sophisticated fixed appliance systems in the 1970s as it was thought that these simplified the approach to orthodontic treatment. More recently, due to the demand for higher aesthetic standards during the developing dentition phase, an appreciation has developed for the advantages of interceptive tooth guidance and as a result there has been a decline in fixed appliance treatment.
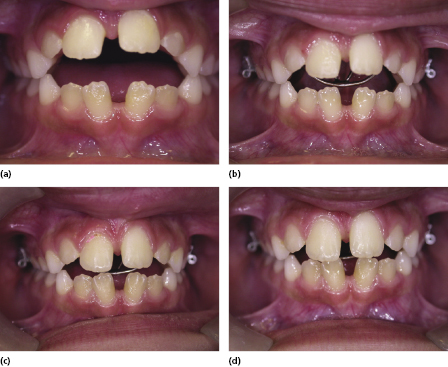
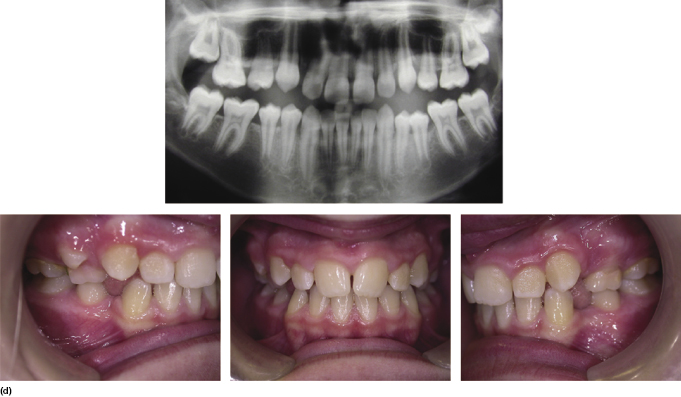
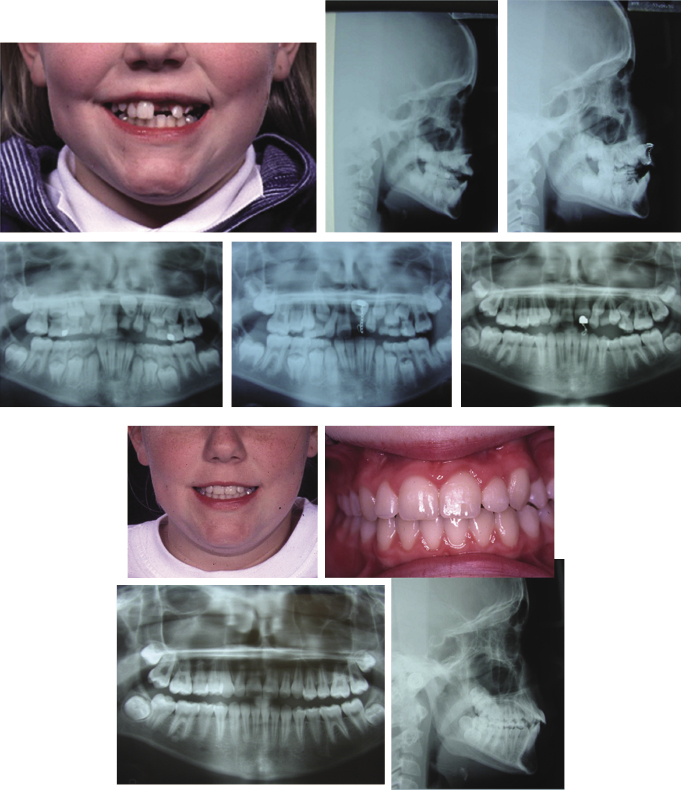
The modern approach starts with the removal of the primary canines in cases where there is anterior crowding to allow the permanent incisors to align as the lateral incisors are erupting (Figure 4.17a). This is usually undertaken at 7–8 years of age. This is followed by a period of occlusal monitoring (Figure 4.17b). As the first premolars erupt at around 10 years of age, the position of the permanent canines is assessed and if crowding is present, the first premolars are removed to allow the eruption of the canines and second premolars into the line of the dental arch (Figure 4.17c). When serial extraction was first described, the first deciduous molars were also extracted, but there is no evidence that they delay the eruption of the first premolars. It is felt that this is an unnecessary stage in the process. During occlusal management with interceptive extractions, the occlusion should be reassessed every 9–12 months until the permanent dentition has erupted (Figure 4.17d). If the permanent tooth position is not ideal, fixed appliances can be placed to improve the tooth position. If the tooth position is acceptable or the oral hygiene is poor, this interceptive approach will hopefully lead to the reasonable alignment of the teeth without the need for fixed appliance therapy.

The premise behind this approach is to use the natural eruptive potential of the teeth to improve tooth position rather than allowing teeth to move ectopically before orthodontic treatment. This approach can significantly shorten the active treatment time. In cases where there is a skeletal element to the malocclusion, serial extraction can be combined with sagittal correction with headgear or functional appliances. When the skeletal discrepancy cannot be managed with functional appliances, masking of the overjet can be done by extraction of the first premolars in the maxilla and allowing proclination of the lower labial segment to manage any crowding in the lower arch. This approach will have implications for retention and must be discussed with the patient.
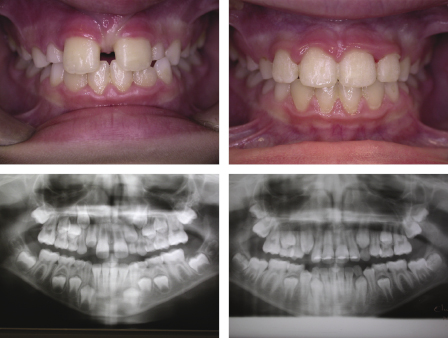
Modern occlusal guidance is geared towards encouraging the permanent dentition to erupt into the line of the dental arch with selective extractions (Figure 4.18). If a tooth is very ectopic (particularly a canine), it may be more expedient to remove this tooth, and thereby avoid the need to commit the patient to many months of complex orthodontics to pull the tooth into the line of the arch. With modern restorative materials and adhesive dentistry, very good camouflage and crown modification can be achieved.

The Unerupted Central Incisor
If the eruption of one central incisor is more than 6 months delayed with respect to the other or the lateral incisor has erupted, it is important to take radiographs to assess its position (Mason et al., 2000). The most common cause of delayed eruption is the presence of a supernumerary tooth (Figure 4.19) (DiBiase, 1968–1969). After removal of the obstruction, 68% of incisors have been shown to erupt spontaneously (if there is sufficient space in the arch) within 12 months (Witsenberg and Boering, 1981). It is prudent however, to bond a gold chain to the unerupted tooth at the time of the surgical removal of the supernumerary(s) to ensure a second procedure is avoided if there is no spontaneous eruption; if there is, the gold chain simply needs to be removed. Careful clinical assessment is required with palpation buccally and palatally. Radiographic examination should include either vertical or horizontal parallax depending on the radiographs taken, and an OPG should always be taken to assess all the developing dentition (Figure 4.20). Cone-beam computed tomography (CBCT) is also an invaluable tool in assessing tooth position (see Figure 3.4).
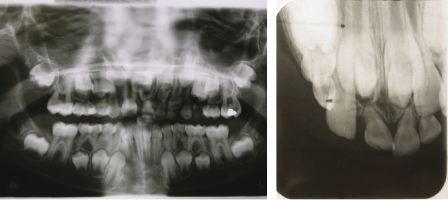
If a tooth is impeded in its eruption, this may be due to an obstruction or dilaceration of the root. If either is the case, the tooth is unlikely to erupt on its own, but could be brought into place with orthodontic traction even if severely ectopic (Figures 4.21 and 4.22).

This treatment however can be very protracted and careful discussion with the patient is needed to ensure their compliance. The advantages of bringing the tooth into the line of the arch is that alveolar bone is preserved and will be brought into the area as the tooth moves. With this approach, the resulting contour of the gingival margin is likely to be better with respect to the other incisors than that achieved with a bridge or implant. Bringing an unerupted tooth down at a young age when there is mixed dentition can be difficult and protracted, and the root of the dilacerated tooth can become compromised. Each case must be assessed on its own merits and skeletal pattern and smile line must be taken into account. Other methods of managing an ectopically positioned tooth, such as autotransplantation of crowded premolars or the unerupted tooth itself, have been tried with varying results. With transplantation, the problems of devitalisation, gingival margin contour and ankylosis must be considered.
Attempting to move the lateral incisor into the central incisor space is also possible and useful if there has been early space loss or there is an increased overjet that requires incisor retraction. The disadvantage of this approach, however, is that the emerging profile of the lateral incisor is usually narrow at the gingival margin, which often leads to poor aesthetics and difficulty with cleaning (Czochrowska et al., 2003) (Figure 4.23). The level of the smile line, alveolar bone level and patient preference will significantly influence the space closure method of choice.

Nowadays the success of single tooth implants often makes this the option of choice; however, an implant cannot be placed until growth has stopped, and the child will have either to wear a retainer to hold the space open or have an acid-etched retained bridge (AERB) placed. The AERB is of course a more stable option as it is not removable from the mouth, but it must be well looked after and demands high oral hygiene standards from the child.
Submerging Deciduous Second Molars
The evidence for the management of these teeth is limited; however, guidance is that if there is a successor, it will usually exfoliate (Ericson and Kurol, 1988a; Power and Short, 1993; Baccetti et al., 2008).
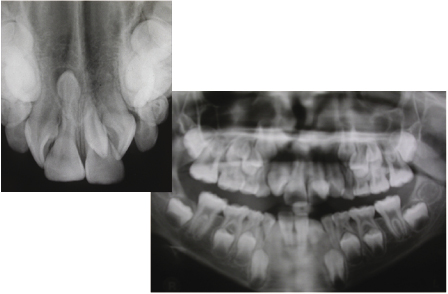
In treatment planning, consideration needs to be given to the presence or absence of crowding, the severity of the submergence and the periodontal condition. An OPG radiograph should always be taken to assess for the presence of a successional tooth under the submerging tooth and whether it is in an ectopic position (Figure 4.24). Extraction of the second deciduous molar can lead to space loss (particularly in a crowded arch) and possible impaction of the developing second premolar if present. This could lead to a food trap and eventual periodontal damage; therefore, early detection and treatment planning are important (Figure 4.25). Where space loss is expected, a space maintainer can be considered. Previously, band and loop styles have been advocated, but these are difficult to make and often do not c/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


