CHAPTER 1
Introduction
An attractive smile with a good display of teeth is important for psychological well-being. There are a number of goals that should be aimed for when considering dental attractiveness, such as the symmetry, alignment, smile line, dental arch shape and gingival contour, as well as the quality and morphology of the dental tissue itself. Orthodontic management of the developing dentition is important to ensure that the established dentition will be in the most aesthetic position. Orthodontics requires a good understanding of facial and dental growth and the effects of occlusal guidance.
In the past it was common practice for patients to be referred to an orthodontist once their secondary dentition was established. This practice allowed many developing problems to significantly worsen and ultimately be more difficult to correct. In many cases, developmental problems can be managed as the dentition develops and early intervention can eliminate some of the complex occlusal problems that can take 24 months or longer to manage with orthodontic appliances.
The premise of early interceptive treatment is to allow the secondary dentition to establish itself in an aesthetic position with the dental units lying within the dental arches. Issues such as skeletal discrepancy are managed within the scope of the genetic potential of each patient and early intervention should be decided on not only with reference to the severity of the discrepancy, but also the aesthetic and emotional needs of the patient and the implications of not undertaking treatment. For these reasons, general dental practitioners (GDPs) must consider early referral to a specialist orthodontist for all patients to ensure that all opportunities for occlusal guidance are taken. Referral at the age of 7 years allows any developing issues to be addressed in a strategic and planned manner.
What Do We Know about Growth?
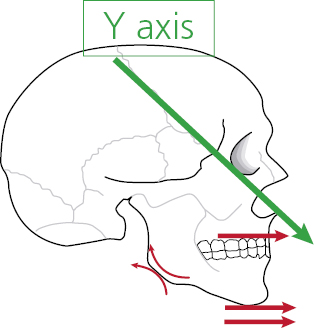
While a patient is still growing, there exists the possibility of addressing orthodontic problems with orthodontic appliances to alter facial growth. However, the problem in clinical orthodontics is that facial growth continues from birth to early adulthood and the growth pattern cannot be accurately predicted. We do know the average rate and direction of growth, but are aware of different skeletal relationships in three planes of space and of growth rotations that lead to differences in facial form from Class II to Class III, high and low angle and transverse discrepancies. We also have some understanding of the role of the facial muscles and the influence environmental factors have on the dentition (Figure 1.1). However, we cannot reliably predict the timing of growth or the ultimate amount of growth for any individual until it is almost at an end, even if analytical techniques such as cervical spine and hand/wrist radiograph assessments are employed. In addition, while the soft tissue balance between the tongue, lips and cheeks and how this affects tooth position and dental arch shape can be predicted, we cannot quantify the latter over time or predict accurately the influences that these may have on the dental arch.
Growth and Development of the Jaws
Growth generally refers to an increase in size, number or complexity by natural development. Development is an increase in the degree of organisation (Proffit, 1993). Craniofacial growth may be divided into four components (Thilander, 1995):
- growth mechanisms (how new bone is formed);
- growth pattern (change in size and shape of the bone);
- growth rate (speed at which the bone is formed);
- regulating mechanism that initiates and directs the above three factors.
Growth Mechanisms
Growth and development of the craniofacial skeleton occurs in two ways:
- endochondral ossification: growth and ossification of a cartilage model;
- intramembranous ossification: transformation of mesenchymal connective tissue and deposition of bone on existing bone surfaces.
The bones of the skull base mainly grow and develop by endochondral ossification, and the vault of the cranium and facial skeleton mainly by intramembranous ossification (Enlow, 1990).
Although several ossified areas fuse into large morphological units, remnants of the chondrocranium persist as synchondroses (cartilaginous joints) between the bones in the cranial base. When intramembranously formed bones meet, sutures develop. Bone growth and adaptation can thus proceed due to the separation of bones in the synchondroses and suture areas.
Growth of the Cranial Base
Displacement growth of the cranial base is made possible mainly by synchondroses. The spheno-occipital synchondrosis is regarded as the most important growth centre for the cranial base (Sicher, 1952; Björk, 1955). The upper facial skeleton is attached to the anterior cranial base, whereas the mandible is connected to the middle cranial base; thus, the length and growth of the cranial base has an important effect on the jaw relationships (Björk, 1955).
Growth of the Mid-Face
Scott (1953) suggested that the essential primary elements directing craniofacial skeletal growth are the cartilages, in particular the anterior extension of the chondrocranium, the nasal septal cartilage. The anteroposterior expansive growth of the nasal septal cartilage, which is buttressed against the cranial base posteriorly, is thought to ‘push’ the mid-face downward and forward and as such, the nasal septum is thought to play an important part in the prenatal and very early postnatal growth of the mid-face. However, opinions differ as to its role in postnatal growth; one view is that growth is secondary to, and compensatory for, passive displacement of the mid-facial bones and the nasal septum plays a significant biomechanical role in maintaining normal mid-facial form (Melsen, 1977; Moss, 1977).
Growth of the Mandible
The cartilage of the mandibular condyle is a secondary cartilage and is different in origin and structure from the epiphyseal plate and synchondrosal cartilage (Thilander et al., 1976).
The traditional view of the condylar cartilage was that it controlled overall mandibular growth and represented a major growth centre for the entire mandible (Scott, 1962). Koski and Makinen (1963) and Koski and Mason (1964) attempted to grow the condylar cartilages of rats and showed that cartilage only grew when it was explanted with the adjacent bone. Koski and his team interpreted this as confirmation of the views of Moss (1968) that growth of the condylar cartilage is always secondary to forward displacement of the mandible as a result of some outside influence, ‘the functional matrix’, and only participates in regional adaptive growth. They suggested therefore, that condylar cartilage is not a major growth centre for the mandible, but it does have a great capacity to adapt to mandibular displacement during growth (Koski and Ronning, 1966; Enlow, 1990).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


