4
Management of pain and anxiety
M.T. Hosey, L. Lourenço-Matharu, and G.J. Roberts
Chapter contents
4.2 The use of analgesics to manage pain in children
4.2.1 Paracetamol (Acetaminophen)
4.2.2 Non-steroidal anti-inflammatory drugs (Ibuprofen)
4.3 Pharmacological management of the anxious child
4.3.1 Children are different from adults
4.4.1 The choice of pharmacological management
4.5 Conscious sedation: drugs and routes
4.5.1 A definition of conscious sedation
4.6 Environment, facilities, and pre- and postoperative instructions
4.6.3 Pre- and postoperative instructions
4.7 Monitoring the sedated child
4.7.1 Alert clinical monitoring
4.7.2 Pulse oximeter and other monitors
4.7.3 Protocols and checklists
4.7.4 Requirements for training
4.7.5 Management of unexpected loss of consciousness
4.8 Nitrous oxide inhalation sedation
4.8.1 Pen picture of the child undergoing nitrous oxide inhalation sedation
4.8.2 Indications and contraindications
4.8.4 The inhalation sedation technique
4.8.6 Monitoring during inhalation sedation
4.9.1 Pen picture of the child undergoing intravenous midazolam sedation
4.9.2 Indications and contraindications
4.9.4 Intravenous midazolam technique
4.9.5 Monitoring during IV sedation
4.10.1 Oral midazolam conscious sedation
4.10.2 Pen picture of the child undergoing oral sedation using midazolam
4.10.3 Indications and contraindications for oral midazolam
4.10.4 Oral midazolam technique
4.10.5 Monitoring during oral sedation
4.10.6 Other drugs used for oral sedation
4.11.1 What is general anaesthesia?
4.11.2 Risks associated with general anaesthesia
4.11.3 Indications for general anaesthesia
4.11.5 Consent for dental treatment under GA
4.11.6 The general anaesthesia service, site, and facilities
4.11.10 Types of GA for paediatric dentistry
4.11.14 Treatment planning for GA
4.1 Introduction
Pain and anxiety are natural physiological and psychological responses. Pain is a direct response to an adverse stimulus that has occurred; anxiety is the unpleasant feeling, the worry that something unpleasant might occur. Pain and anxiety are often intertwined, especially in the dental setting. The best way to manage child dental anxiety is to avoid its occurrence in the first place through prevention of dental disease, good behaviour management, pain-free operative care, and treatment planning that is tailored to the needs and developmental stage of each individual child. These issues are detailed in the previous chapters. This chapter specifically focuses on pharmacological pain and anxiety control and explores the roles of conscious sedation and general anaesthesia (GA) as adjuncts to behaviour management.
A child’s perception of pain is purely subjective and varies widely, particularly with age. Infants up to about 2 years of age are unable to distinguish between pressure and pain. Older children begin to have some understanding of ‘hurt’ and begin to distinguish it from pressure or ‘a heavy push’. It is not always possible to identify which children are amenable to explanation and will respond by being cooperative when challenged with local anaesthesia (LA) and dental treatment in the form of drilling or extractions. Children over 10 years of age are much more likely to be able to think abstractly and participate more actively in the decision to use LA, sedation, or GA. Indeed, as children enter their teenage years they are rapidly becoming more and more like adults and are able to determine more directly, sometimes aggressively, whether or not a particular method of pain control will be used. The response is further determined by the child’s coping ability influenced by family values, level of general anxiety (trait), and intelligence.
There is a strong relationship between the perception of pain experienced and the degree of anxiety perceived by the patient. Painful procedures cause fear and anxiety; fear and anxiety intensify pain. This circle of cause and effect is central to the management of all patients. Good behaviour management reduces anxiety, which in turn reduces the perceived intensity of pain, which further reduces the experience of anxiety. (See Key Point 4.1.)
4.2 The use of analgesics to manage pain in children
A number of oral conditions, such as ulcers, teething, and pulpitis, can lead to children complaining of pain. Studies have shown that almost a quarter of 5-year-old preschool children have had a recent episode of dentally related pain. This can lead to the child being sent home from nursery or school, work time lost by parents, and visits to the dentist or doctor.
The management of the dental pain depends on the cause but usually involves some form of clinical intervention (e.g. a dressing). This operative management of toothache and the management of other dental emergencies are covered elsewhere in this text. However, sometimes the use of oral analgesics to achieve pain relief is required whilst the operative measures are taking effect. Children may need pain control for ‘toothache’ for a day or two before the removal of carious teeth. Additionally, analgesia is required postoperatively, usually after dento-alveolar surgery, and perioperatively during extractions under GA.
The use of analgesics should be viewed as a temporary solution whilst the causative factors are being brought under control (see Box 4.1). The most commonly used analgesics for oral pain in children are also the familiar ‘over-the-counter’ medicines, namely paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs). Therefore a prescription is not required. Most parents are already familiar with these preparations and their brand names.
Table 4.1 Over-the-counter analgesics
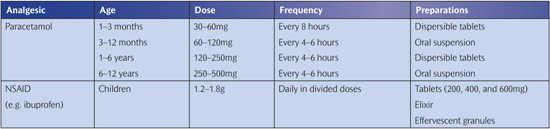
The most common method of administration is by mouth. Small children and some recalcitrant adolescents refuse to take tablets, so liquid preparations are needed. Sugar-free preparations are readily available.
It should be remembered that the dose for children of different ages needs to be carefully estimated to avoid the risk of an overdose (dangerous) or an underdose (ineffective) (Table 4.1). The parents must be advised that all drugs must be stored in a safe place in a child-proof container. Bathroom cabinets or kitchen cabinets are the safest places as they are out of reach and out of sight of small children. Specific advice on prescribing for children can be obtained from a local pharmacist or the British National Formulary (BNF).
4.2.1 Paracetamol (Acetaminophen)
Paracetamol is a non-opiod analgesic. For children, it is available as an oral suspension (120/5mL or 250/5mL). It is also available as tablets, soluble tablets, and suppositories. Overdosage can cause symptoms of nausea and vomiting. Single or repeated dosages totalling as little as 150mg/kg within 24 hours may cause liver damage, so parents should be advised to read instructions on the packet.
4.2.2 Non-steroidal anti-inflammatory drugs (Ibuprofen)
The most commonly prescribed drug in this category is ibuprofen. NSAIDs have the added advantage of being anti-inflammatory and therefore may be of benefit in pulpitis or when a child is pyrexic. Over dosage may cause nausea, vomiting, epigastric pain, and tinnitus. Ibuprofen should be avoided in asthmatics since it has been known to precipitate bronchoconstriction. NSAIDs are known to cause stomach ulceration, and so parents should be advised to avoid prolonged usage.
4.3 Pharmacological management of the anxious child
The different methods of anxiety control vary from simple behaviour management to full intubational GA in a hospital operating theatre. The majority of dental procedures on children can be carried out using a combination of behavioural management and local anaesthesia.
Children’s behaviour can be characterized in four ways: (1) cooperative; (2) potentially cooperative; (3) lacking cooperative ability (pre-cooperative); (4) uncooperative. Potentially cooperative children may manage a simple examination, but operative procedures, especially if these are carried out too early in the treatment plan, may be beyond their coping ability. An example of this is a child who readily accepts fissure sealants but who is upset at tooth extraction. Thoughtful treatment planning and good behaviour management will usually suffice for this group, especially if the child is asymptomatic and treatment can progress at an easy pace. However, when invasive treatment is unavoidable (maybe it is all that is required, e.g. orthodontic premolar extractions) or when an emergency situation arises, conscious sedation may be needed.
The pre-cooperative child is the very young child with whom communication cannot yet be established even though they may potentially cooperate later, when they are more mature. The uncooperative child is too anxious to cope with any procedure. Children with specific disabilities with whom cooperation in the usual manner may not ever be achieved also fall into this category. Both of these groups need a different approach, which may include conscious sedation or GA.
Children learn to be anxious by experience, through either a real traumatic event or what they perceive to be a traumatic event. This is why irregular dental attendees who first present with toothache and require an emergency operative intervention can be so traumatized by the event that they become dentally anxious. Although pharmacological management is an adjunct to, rather than a replacement for, the specific behavioural techniques that are employed, its use should be considered in an emergency and in potentially traumatic situations. This is known as ‘prophylactic’ sedation.
4.3.1 Children are different from adults
Children are different from adults and sedating them can be unpredictable. They are more likely to become hypoxic, i.e. low blood oxygen leading to low brain oxygen. The reason for caution when sedating children is related to child anatomy, physiology, drug response, and emotional development. Anatomically, children have large heads, tongues, tonsils, and adenoids. They also have a U-shaped larynx and narrow pharyx. They have a greater ratio of body surface area to body weight, a higher metabolic rate, and higher oxygen consumption. It is common for children to present with upper respiratory tract infections. Cardiac output in children is 30–50% higher than in adults, and the arterial blood pressure is lower. Children have smaller veins, which are often hidden under subcutaneous fat. They are emotionally and psychologically underdeveloped, which may result in the occurrence of dysphoria during and after sedation. (See Key Point 4.2.)
4.3.2 Guidelines
According to the National Institute for Health and Clinical Excellence (NICE) guidelines (NICE 2010), sedation may be considered in children and young patients when a procedure is too frightening or too painful, or needs to be carried out in a child or young person who is ill or in pain or who has behavioural problems. Nitrous oxide inhalation sedation is the most common and also the safest sedative agent for use in children’s dentistry and is considered to be the ‘standard technique’.
In the UK, attitudes related to GA have changed since the Poswillo Report in 1990 (Department of Health 1990). This report included recommendations to discourage GA in favour of sedation. This resulted in a renewed interest in conscious sedation techniques and drugs for behavioural and anxiety control in children. In common with many European countries, ‘deep sedation’ is not recommended for paediatric dental practice. These techniques are considered to be a form of GA, and as such further regulations and safeguards apply.
Dental treatment should only be carried out under GA when this is judged to be the most clinically appropriate method of pain and anxiety management. Children undergoing outpatient dental GA receive the same standard of preparation and assessment, including preadmission, as children admitted for medical procedures. The Association of Paediatric Anaesthetists of Great Britain and Ireland (APAGBI), in collaboration with a wide range of stakeholders, has published guidelines to develop an evidence-based consensus on the care pathway from referral to discharge for children and young people who are considered for outpatient dental extractions under GA (APAGBI 2011).
4.3.3 Evidence
Numerous studies have been carried out worldwide to explore the use of pharmacological agents in paediatric dental management. Despite this, a Cochrane systematic review was unable to conclude which sedative drug is the most effective (Matharu and Ashley 2006). This was because the majority of studies, especially those carried out in the USA, used polypharmacy in conjunction with either 30% or 50% nitrous oxide, and many also used some form of physical restraint. Indeed, 19 different drugs or combinations of drugs and various modes of administration were reported. Therefore the choice of drug and method of sedation is largely determined by the culture, legal framework, professional ethics, and accepted definition of conscious sedation in any given country.
4.3.4 Medical status
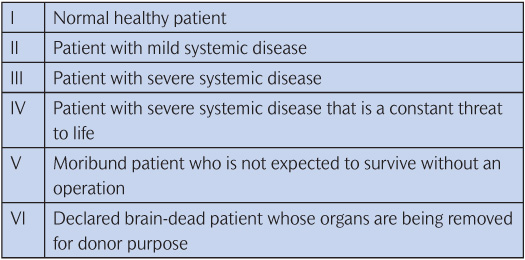
The American Society of Anesthesiologists (ASA) classification (Table 4.2) provides an excellent guide to the appropriateness of the pharmacological management and the setting in which the patient should be treated (ASA 2006). In general, ASA I and ASA II patients are suitable for treatment in primary care settings and simple sedatives can be used. There are a wide variety of medical problems and medically compromised children are usually treated in hospital under the care of a team led by a paediatric dentistry consultant so that there is liaison with medical services and access to inpatient facilities if required.
4.4 Clinical decision-making
The decision as to whether a patient should be treated under GA, LA, or LA with sedation depends on a combination of factors, the most important of which are the age of the child, the degree of surgical trauma involved, the perceived anxiety and how the patient may respond (or has responded) to similar levels of surgical trauma, the complexity of the operative procedure, the number of quadrants involved, and the medical status of the child.
There are no hard and fast rules. Every procedure in every child must be assessed individually and the different elements considered in collaboration with the parent and, where appropriate, the child (Box 4.2). For example, the younger the child, the greater is the likelihood of the need for GA. At the other end of the age range it is unlikely that a 15-year-old will need GA for simple orthodontic extractions, although this might be required for moderately complex surgery such as exposing and bonding an impacted canine. The degree of trauma involved is also another factor; a single extraction is most likely to be carried out under LA, whereas removal of the four first permanent molars is most likely to be carried out under GA. Anxiety perceived as excessive, especially after an attempt at treatment under LA and sedation, might lead to simple treatment such as conservative dentistry being carried out under GA, usually involving endotracheal intubation. Serious medical problems (e.g. cystic fibrosis with its associated respiratory problems) would justify using sedation instead of GA even for more traumatic surgery, such as removal of impacted canines, but it would be appropriate to carry out this sedation in a hospital environment. The degree of intellectual and/or physical impairment in special needs or medically compromised children is also a factor to be considered.
Table 4.2 ASA physical status classification
The need for the use of LA is also a factor in determining the best management option. Sedated patients still need to have LA administered. It is important that usage, and especially the dosage, of LA is considered in the decision-making process. Readers are reminded that care must be taken to avoid overdosage in children. Therefore several visits may be needed to complete treatment if sedation is planned.
4.4.1 The choice of pharmacological management
The choice of the most suitable pharmacological technique should be based on all the following factors:
• invasiveness of the proposed procedure
• level of sedation anticipated
• contraindications
• side-effects
• patient (or parent/carer) preference
• operator preference.
4.5 Conscious sedation: drugs and routes
The routes of administration of sedative drugs used in clinical paediatric dentistry are oral, inhalational, intravenous (IV), and transmucosal (e.g. nasal, rectal, and sublingual). Nitrous oxide inhalation sedation is considered to be the standard conscious sedation technique. Other drugs and routes are seldom used in the UK. Whilst there is considerable recent interest in the use of midazolam, a benzodiazepine, this is generally confined to paediatric dentistry specialist units rather than primary care settings. ‘Advanced techniques’ such as propofol target-controlled infusion pumps and patient-controlled sedation (PCS) require further research. (See Key Points 4.3.)
4.5.1 A definition of conscious sedation
Conscious sedation is a technique in which the use of a drug or drugs produces a state of depression of the central nervous system (CNS) enabling treatment to be carried out, but during which verbal contact with the patient is maintained throughout the period of sedation. The drugs and techniques used to provide conscious sedation for dental treatment should carry a margin of safety wide enough to render loss of consciousness unlikely. The level of sedation must be such that the patient remains conscious, retains protective reflexes, and is able to understand and respond to commands.
The ideal qualities of a sedative agent are:
• both sedative and analgesic effects
• easy and acceptable method of administration
• easy titration
• minimal cardiovascular side-effects
• minimal respiratory side-effects
• rapid onset of action
• rapid recovery
• no accumulation in renal/hepatic dysfunction
• inactive metabolites
• inexpensive
• no interactions with other drugs.
4.6 Environment, facilities, and pre- and postoperative instructions
4.6.1 Environment
There should be a suitable child-friendly area where the child can be treated in a calm, peaceful setting without noise or interruption. When oral sedation is planned, a ‘quiet room’ is needed so that the child can sit quietly before the dental procedure. This is the place where the sedative is administered and the child monitored while sedation is taking effect.
Irrespective of the choice of sedative drug, all equipment must be checked to ensure that it is working correctly before the child enters the surgery. This includes the operating light, dental chair, three-in-one, dental headpieces, dental materials, instruments, and suction.
Sedated patients may hallucinate or misinterpret words and actions, so a chaperone must be present at all times to safeguard the operator–sedationist. Once treatment is complete the child must sit quietly until sufficiently recovered to be accompanied home. (See Key Points 4.4.)
4.6.2 Facilities
The use of sedative drugs carries the risk of inadvertent loss of consciousness. Although the techniques are designed to reduce this risk to a minimum, it should always be borne in mind that every time a sedative is given to a patient there is a risk of an idiosyncratic reaction to the drug which may result in hypoxia or unexpected loss of consciousness.
4.6.3 Pre- and postoperative instructions
All instructions should be provided verbally and in writing in advance of the sedation visit and then confirmed at the time of sedation.
Fasting is not required prior to either nitrous oxide inhalation sedation or IV midazolam sedation. The ‘2–4–6’ rule applies for oral sedation and GA. This is 2 hours fast for clear fluids, 4 hours fast for milk, and 6 hours fast for solids.
Preoperative information should also include any possible side-effects and requirements for postoperative care, since families need to plan the return home in advance. Suitable arrangements need to be in place for travel, to ensure that the child plays quietly at home, and t/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Key Point 4.1
Key Point 4.1 Key Point 4.2
Key Point 4.2 Key Points 4.3
Key Points 4.3 Key Points 4.4
Key Points 4.4