Control of pain and anxiety
4.1 Systemic analgesia
Nociception and pain
Nociception: Nociception has been defined as the process of detection and signalling the presence of a noxious stimulus. Detection involves the activation of specialised sensory transducers, nociceptors, attached to Aδ and C fibres.
Pain: The International Association for the Study of Pain (IASP) has endorsed a definition of pain as an ‘unpleasant sensory and emotional experience associated with actual or potential damage, or described in terms of such damage’. Pain involves a motivational-affective component as well as a sensory-discriminative dimension and can occur without nociception.
Inflammatory and neuropathic pain
Clinical pain may be inflammatory or neuropathic in origin; the former refers to pain associated with peripheral tissue damage, such as that produced during surgery, and the latter refers to pain resulting from nervous system dysfunction, such as is seen in postherpetic neuralgia or trigeminal neuralgia (Chapter 14).
Dental pain and pain after surgery
Analgesics should be prescribed according to their effectiveness and appropriate to the pain intensity reported by the patient or the anticipated postoperative pain intensity and taking into account potential adverse effects and the general health of the patient (Table 4.1). There are many clinical trials comparing analgesic effectiveness and the most effective drugs have a low NNT, where the NNT is the number of patients who need to receive the active drug to achieve at least 50% relief of pain compared to placebo over a 4–6 hour treatment period.
Table 4.1
Systemic pain relief after dental and surgical procedures
| Typical pain level | Type of procedure | Protocol |
| Mild pain | Forceps extraction | Paracetamol 1 g every 6 hours regularly (maximum 4 g/24 h) |
| Moderate pain | Surgical removal of tooth | Ibuprofen 400 mg every 6 hours regularly (maximum of 2.4 g/24 h) and paracetamol 1 g every 6 hours as necessary (maximum of 4 g/24 h) |
| Severe pain | Surgical removal of tooth involving bone removal | Ibuprofen 400 mg every 6 hours regularly (maximum of 2.4 g/24 h) and paracetamol 1 g/codeine 60 mg combination every 6 hours regularly (maximum of 4 g paracetamol/24 h) When NSAIDs contraindicated: paracetamol 1 g/codeine 60 mg combination every 6 hours regularly (maximum of 4 g paracetamol/24 h) |
| Severe pain for inpatients | More difficult surgical removal of teeth or major surgery | Morphine by intravenous titration or intermittent intramuscular injection |
Acetaminophen (paracetamol) possesses antipyretic activity and is an effective analgesic. It is considered safe because it does not have the side-effects such as gastrointestinal ulceration and haemorrhage, cardiorenal adverse effects or impair platelet aggregation. However, paracetamol is associated with liver toxicity, especially in patients who already have compromised liver function, cirrhosis or hepatitis. Patients should always be warned that many combination analgesics may contain paracetamol and they should only take the analgesics recommended or prescribed. Paracetamol may be administered intravenously, intraoperatively followed by oral administration after discharge home.
• hypersensitivity to aspirin or any other NSAID
• history of gastrointestinal bleed, peptic ulcer disease
• those with coagulation defects, inherited bleeding disorder and patients who are taking oral anticoagulants
Dosing schedules
Analgesic drugs should be given at regular times according to their half-life and at high enough doses to ensure therapeutic plasma levels. Adequate doses of analgesics should not be withheld because of misconceptions and fears on the part of the prescriber. It is wrong to believe that pain is the inevitable consequence of surgery or that the use of opioids for acute pain in hospital will lead to addiction.
4.2 Local anaesthesia
By common usage, the localised loss of pain sensation is referred to as ‘local anaesthesia’, rather than local analgesia, which would be more accurate. The word ‘anaesthesia’ implies loss of all sensation including touch, pressure, temperature and pain.
Mechanism of action
Failure of anaesthesia
Failure of anaesthesia can occur for a number of reasons:
• Inadequate dose administered: the full contents of a dental cartridge (1.8–2.2 ml) are required to obtain a reliable mandibular block according to minimum-dose calculations (Fig. 4.1).
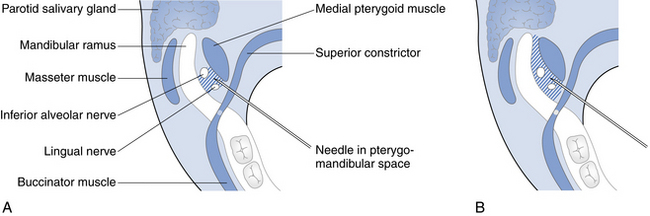
Fig. 4.1 Diagram of pterygomandibular space illustrating the need to inject an adequate dose of local anaesthetic for a reliable block of inferior alveolar and lingual nerve conduction.
(A) The area covered by 1 ml of local anaesthetic, which is not sufficient to block conduction. (B) A full cartridge of local anaesthetic is necessary to block the inferior alveolar and lingual nerve conduction.
• Inaccurate injection technique: inadvertent injection of solution into a vein or muscle will result in inadequate anaesthesia.
• Biological variation: duration of anaesthesia may vary widely between individuals.
• Anatomical variation: can lead to ineffective anaesthesia (e.g. of an inferior dental block when an aberrant mandibular foramen occurs).
Complications
There are three typical types of complication:
Toxic: Overdose with LA may lead to light-headedness, sedation, circumoral paraesthesia and twitching. More serious overdose can result in convulsions, loss of consciousness, respiratory depression and cardiovascular collapse. Accidental i.v. injection may lead to excessively high plasma concentration. Prilocaine has low toxicity, similar to lidocaine, but if used in high doses may cause methaemoglobinaemia.
Allergic: Approximately two million dental local anaesthetic injections are administered daily around the world. Reports of allergic reactions are extremely rare. In the past, they may have been associated with the preservative (methylparaben) that was included in the cartridge or antioxidant (metabisulphite) used to stabilise the adrenaline in amide-type anaesthetics. If a patient gives a history compatible with an allergic reaction (rash, swelling or bronchospasm), rather than psychogenic reaction or the consequences of i.v. injection (tachycardia), then they should be referred for allergy testing. Hypersensitivity reactions occur mainly with the ester-type local anaesthetics such as benzocaine, cocaine and procaine. Latex-free plungers and seals are used by most manufacturers.
Local complications
Complications of inferior alveolar nerve block
• Injection into the medial pterygoid muscle may result in trismus as well as ineffective anaesthesia.
• Deep injection into the parotid salivary gland may result in blockade of the facial nerve and temporary facial muscle paralysis.
• The patient may experience an ‘electric shock’ type of sensation if the needle touches the inferior alveolar nerve and the injection should only start after withdrawing the needle 1 mm; otherwise direct damage resulting in long-term paraesthesia may result.
Types of local anaesthetic drugs
Intraoral: Lidocaine (4%) is available as an ointment or gel. There are also spray formulations (10% lidocaine) available for intraoral use.
Skin: Lidocaine 2.5% and prilocaine 2.5% (EMLA) or 4% tetracaine (amethocaine) (AMETOP gel). EMLA (eutectic mixture of LA) is contraindicated in infants under 1 year and AMETOP is not recommended in infants under 1 month.
Application method: The LA is applied to the skin and covered with a dressing. The dressing and gel is removed before venepuncture 60 minutes (EMLA) or 30 minutes (AMETOP) later. Systemic absorption is low from skin but topical LAs should never be applied to wounds or mucous membranes, where absorption is rapid.
Vasoconstrictors
• Synthetic analogue of naturally occurring vasopressin.
• Constricts venous outflow and, therefore, is less effective in haemorrhage control than adrenaline (epinephrine).
• Contraindicated in pregnancy as it is similar to oxytocin and there is a possibility of uterus contraction, although the dose is actually very small compared with the dose of oxytocin used by obstetricians to induce labour.
Drug dose for safety
Estimation of a safe dose must take into account:
The maximum recommended doses are given in Table 4.2. Articaine has not been recommended by the manufacturer for use in children under 4 years of age, although dentists have been known to use it and find it effective in children between 2–3 years.
Table 4.2
Maximum recommended doses of local anaesthetics
| Preparation | Maximum dose in healthy adult | Child (20 kg) |
| 2% Lidocaine | 4.4 mg/kg up to 300 mg (7 cartridges) | 2 cartridges |
| 3% Prilocaine | 6.0 mg/kg up to 400 mg (6 cartridges) | 1.8 cartridges |
| 4% Prilocaine | 6.0 mg/kg up to 400 mg (4.5 cartridges) | 1.4 cartridges |
| 4% Articaine | 7.0 mg/kg up to 440 mg (5 cartridges) | 1.5 cartridges |
4.3 Conscious sedation
Routes of administration: Sedative drugs may be administered by a variety of routes, for example, via the lungs, via the gastrointestinal tract (orally or rectally), intranasally, by intramuscular injection or directly into the circulation by intravenous injection. The most popular are the inhalational, oral and i.v. routes.
Risk avoidance: When using sedation techniques, it is important to avoid risks and the dentist should only proceed with methods with which he or she feels competent, in an environment that is adequately equipped and with staff that are appropriately trained. There should always be a second person present who is trained in the care of sedated patients. While UK dental schools provide undergraduate students with the necessary knowledge and skills to enable them to provide conscious sedation to patients, the British General Dental Council currently recommends additional postgraduate training. It is essential that dentists and their staff working in these fields are familiar with the appropriate regulations according to their country of practice.
All dental treatment facilities must have appropriate equipment and drugs for resuscitation at hand, the dentist and his or her team must have the skills to use them in an emergency whether providing conscious sedation techniques or treatment under local anaesthesia alone.
Assessment for conscious sedation
Psychological indications: Anxiety may be the most obvious and common reason for prescribing conscious sedation rather than LA alone but it is important to confirm this by discussion, rather than accept a request for sedation from a patient who may not be aware of its implications or of treatment alternatives. It may be necessary to justify the selection and patient preference alone is not sufficient reason. Extremely anxious and phobic patients may require GA for their dental management or consideration of other strategies such as cognitive behavioral therapy (CBT).
Dental indications: Moderately difficult or prolonged procedures such as dental implant surgery may be an indication for sedation. Some patients who are happy to undergo routine dental treatment with a LA alone, may require sedation to accept more invasive surgical procedures. Extensive dental treatment or surgery may require GA.
Medical and behavioural indications: Systemic disorders such as mild angina, controlled hypertension or controlled anxiety-induced asthma, may be an indication for the use of sedation as this minimises the psychological response to stress and so will reduce the activity of the sympathetic nervous system. This may avoid, or at least reduce, the likelihood of an angina or asthma attack or of raising the systemic blood pressure. Those with cardiorespiratory compromise should receive supplemental oxygen.
Contraindications
Psychological and social contraindications: It is better to admit defeat and arrange for treatment under a GA than to attempt sedation of a totally uncooperative patient. Successful sedation requires a patient to have sufficient intellect, insight and cooperation. Psychologically immature individuals unmanageable with LA alone may exhibit disinhibited or childish behaviour when sedated and so a GA may be needed.
Dental contraindications: Prolonged or difficult oral surgery is a contraindication to treatment under any form of sedation as this may stretch both the patient and operator beyond their limits of endurance. It must also be remembered that sedation techniques do not reduce surgical morbidity. Planned GA may be preferable.
Allergy: Allergy to sedatives or anaesthetics is obviously an absolute contraindication to the use of these drugs, but such allergies are very rare.
Systemic disease: Severe forms of systemic disease such as a recent myocardial infarct or poorly controlled or severe hypertension or angina, may be obvious contraindications for sedation for GA, but even hay fever or the common cold may contraindicate inhalational sedation if there is nasal obstruction.
Respiratory disease: Chronic obstructive pulmonary diseases (COPD) such as bronchitis, emphysema or bronchiectasis are contraindications. Such patients are particularly sensitive to the respiratory depression associated with benzodiazepines and anaesthetic drugs. Also, patients whose respiration is driven by a low partial pressure of oxygen rather than their partial pressure of carbon dioxide are likely to have their hypoxic drive removed by the relatively high concentration of oxygen administered during inhalational sedation. Patients with impaired cardiac function, as well as those with chronic obstructive pulmonary disease may be subject to hypoxic drive.
Pregnancy: Women who are, or may be pregnant, should preferably not be sedated or given a GA. Nitrous oxide inactivates vitamin B12, inhibits DNA formation and may be teratogenic. Its use in elective situations is therefore, contraindicated, particularly during the first trimester when cell differentiation is occurring. Nitrous oxide may be used safely, however, during late pregnancy and indeed is frequently used for pain relief during childbirth. Animal experiments have not indicated any teratogenic risk with midazolam, but evaluation in human pregnancy has not been undertaken and it would, therefore, be unwise to use it unless considered essential. High doses of benzodiazepines in the last trimester of pregnancy have been reported to produce irregularities of the fetal heart rate, hypotonia, poor sucking and hypothermia in the neonate. Midazolam should not, therefore, be used during the last trimester. Caution must be exercised when using intravenous sedation for breastfeeding mothers. If using midazolam, it is reasonable to ask the mother not to breastfeed for 8 hours after the sedation and use synthetic or pre-expressed milk during this time.
Liver and kidney disease: Since benzodiazepines are metabolised by the liver and excreted by the kidneys, diseases affecting these organs may interfere with recovery. Alcoholics may have some degree of liver damage and should therefore, be sedated with caution.
Muscle disease: Myasthenia gravis and other muscle-weakening or muscle-wasting diseases are contraindications to the use of benzodiazepines because of the risk of serious respiratory depression.
Obesity: Obese patients often have poor airway control and may also have difficult veins to cannulate.
Psychiatric disorders: Patients with severe psychiatric or personality disorders may also be unsuitable for sedation as disinhibiting effects may be observed. Patients taking CNS depressants, such as potent analgesics, tranquillisers or sleeping tablets, may be unpredictably sensitive to or tolerant of sedation. The possibility of severe respiratory or cardiovascular depression should be considered when using benzodiazepines.
Patients who are using non-prescribed drugs may have increased tolerance an/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


