Biologic Aspects
Protection of the Pulp and Dentin Adhesion
D. Pansecchi, F. Brenna, P. Ferrari, L. Breschi, G. Dondi dall’Orologio, M. Gagliani, L. Fadini and A. Cerutti
Pulp-Dentin Protection with Adhesive Techniques
Esthetics and Function in Relation to the Internal Biologic Structures
Direct Restoration with Pulp-Dentin Protection of Two Class I Cavities with Esthetic Adhesive Materials
Direct Pulp Capping with Adhesive Techniques
Innovations in the Field of Dentin Adhesion
Protection of the Pulp
The following characteristics make the dental pulp unique compared with any other body tissue:
• Pulp is surrounded by unyielding walls of dentin and therefore cannot expand in response to inflammatory lesions.
• Vascularization is terminal arteriolar, which reduces the pulp’s ability to regenerate itself after an injury; one or more arterioles enter the tooth through the apical foramen, and smaller vessels can enter the pulp through lateral channels.
• Innervation lacks proprioceptive sensory mechanisms.
• It is composed almost entirely of specialized loose connective tissue and a highly sophisticated cell population: odontoblasts in the outer area near the dentin, and fibroblasts, lymphocytes, macrophages, and undifferentiated mesenchymal cells in the inner portion of the tissue.
Functions of the Dental Pulp
The dental pulp has four major functions: dentinogenic, defensive, sensory, and nutritive.
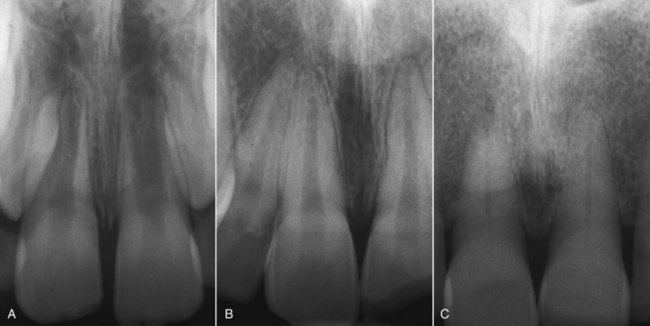
Figure 4-2 shows the radiographs of 8-, 25- and 79-year-old patients. These are sound teeth with healthy pulp that exhibit physiologic responses to pulp vitality and percussion tests and that radiographically do not show any sign of calcification or root resorption but a normal lamina dura and a periodontal space of normal width.
Trauma
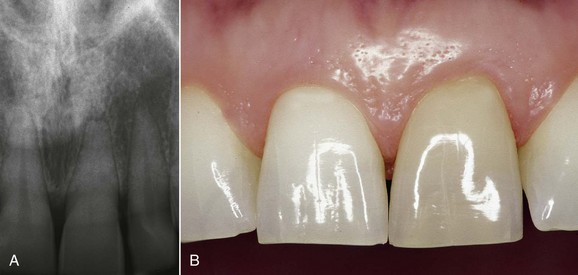
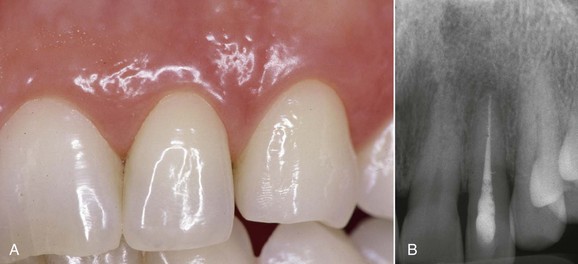
Figure 4-3 shows pulp that has aged prematurely, as it belongs to a young patient (tooth 9). The pulp chamber and root canal have clearly disappeared. This is a sign of pulp damage and can be observed as the result of trauma with injury of the neurovascular bundle. The crown is discolored as a result of degradation of hemoglobin released from the red blood cells that infiltrated the dentinal tubules.
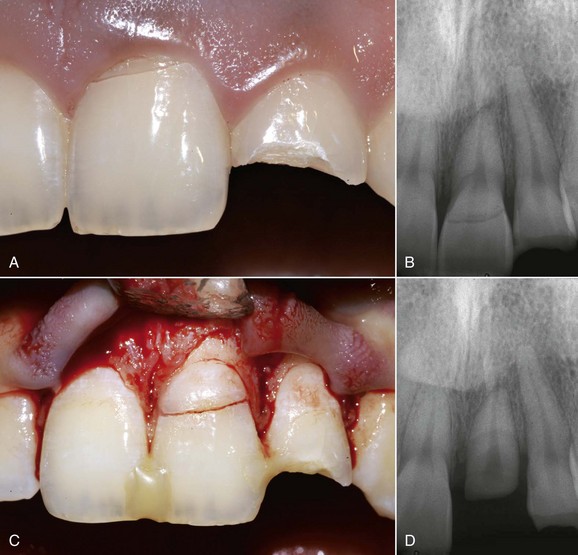
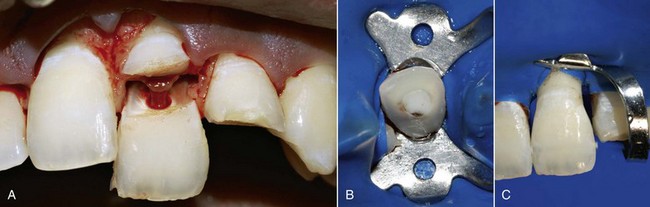
This kind of aging is frequently asymptomatic, and often the patient comes to observation because of unsightly dental crown discoloration or the onset of periodontal symptoms caused by pulp necrosis; in some cases it is noted on x-ray images. The following clinical case (Figure 4-4) is the result of trauma. This young patient (21 years old) presents a buccal supracrestal and palatal subcrestal complete crown-tooth fracture complicated by pulp exposure (Ellis Class V fracture). Figures 4-5 and 4-6 also show the outcome of the trauma.
What the Pulp Should Be Protected From
In the early 1970s the pivotal studies of Brännström clarified that the greatest threat to pulp and dentin integrity is represented by bacteria and their metabolic products (Figures 4-7 and 4-8).
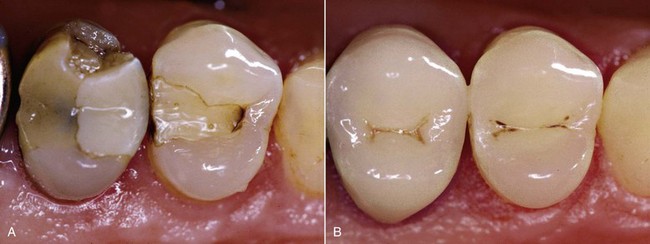
Microleakage
Microleakage is the clinically undetectable passage of bacteria, fluids, and molecules between the cavity wall and the restoration (Figures 4-9 to 4-11).
It is important to maintain the integrity of the marginal seal over time. According to Brännström (1984), when the bacteria nested in the dentin are deprived of nutrients, they probably die.
According to Langeland (1987), pulp reactions caused by initial caries can be reversed by removing the carious dentin.
The key factors for a successful caries treatment are as follows:
• Complete removal of softened infected dentin
• Best possible fit between restorative material and the enamel-dentin substrate to prevent bacterial growth and reinfection of the dentin tubular system (Figure 4-12)
Protection of the dentinal tubules exposed by cavities or prosthetic abutment preparation is crucial for the preservation of pulp vitality, in order to avoid the passage of bacteria and toxins into the pulp. This can be achieved with hermetically sealed restorations able to prevent marginal microleakage and bacterial invasion (Figure 4-13).
Defense Mechanisms
The pulp-dentin complex defends itself against bacterial invasion: 6 hours after cavity preparation, dentin permeability is reduced by approximately 75% (Pashley, 1983).
Protection of the Pulp
Another way to protect the pulp-dentin complex is by using a rubber dam.
The factors that affect the response of the pulp in restorative dentistry are:
• Preoperative conditions of the pulp
• Method of cavity preparation and cleaning
• Tissue changes in dentin and permeability
• Amount and pathogenicity of bacteria at the tooth-restoration interface
The following three key considerations must be made:
• The real status (histology) of the pulp at the time of restoration cannot be ascertained.
• The effect of the iatrogenic trauma of preparation cannot be assessed. Excavation and drying can deal the final blow to the pulp, which is already damaged (even if asymptomatic).
• The countless variables related to materials, dentin substrate, and clinical procedures should be considered.
Pulp Damage
Preparation of the Abutment for a Full Crown
Abutment preparation for a full crown affects all the dentinal tubules. This is an extreme case.
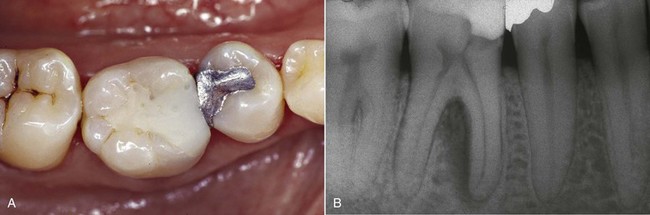
In the case of the first upper molar, which has a mesialized pulp chamber, removal of the mesial dentin wall should be performed very carefully (Figure 4-14).
Temporary Restoration
It is essential to protect the pulp-dentin complex from bacterial, chemical, physical, and thermal insults in the period between tooth preparation and definitive cementation of the direct or indirect prosthetic restoration (Figure 4-15).

Figure 4-15 The tooth is protected during the period between preparation and final cementation of the crown.
Pulp Necrosis Caused by Periodontal-Prosthetic Treatments in Vital Teeth
A study conducted by Ferrara (1991) examined the frequency of periradicular lesions after pulp necrosis of vital teeth used as abutments in periodontal-prosthetic treatments. The teeth had been reduced at least 2 years before the beginning of the study, and at the time they were sound and had no history of trauma. Periradicular lesions were found in 22.6% of cases, and the percentage increased when periodontal involvement was more severe. A previous study by Bergenholtz and Nyman (1984) yielded similar results.
Therefore precision of the margins as well as optimal internal adaptation of the provisional (relining) is very important. This prevents dissolution of the temporary cement owing to infiltration of saliva, imprecise margins, and/or excessive thickness of the cement (Fichera, 2004).
Natural Communication Routes between the Endodontium and the Periodontium
The communication routes are represented by dentinal tubules, the apical foramen, and lateral channels (Figures 4-16 and 4-17).
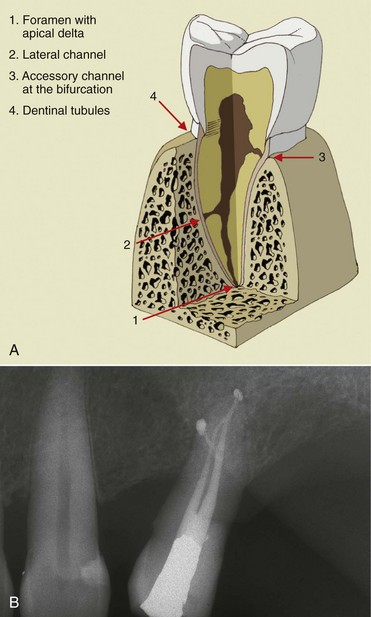
Figure 4-16 First lower molar.

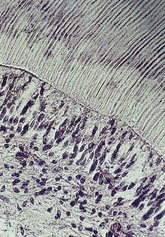
Figure 4-17 Dentinal tubules.
Dentinal Tubules and the Apical Foramen
The dentinal tubules run from the pulp to the amelo-dentinal junction and the cemento-dentinal junction, with a diameter of about 2.5 microns on the pulp side and about 1 micron at the opposite end (see Figure 4-17).
The apical foramen is the main route of communication between the endodontium and the periodontium and represents the main exchange channel for diseases in both directions (Figures 4-18 to 4-21).

Figure 4-19 Lower diaphanized premolar.
Lateral Canals
According to a study on the morphology of root canals conducted by Walter Hess (1925), the occurrence of lateral canals is estimated to be about 43.5%.
Lateral canals unquestionably act as a point of exit of the disease toward the endodontium-periodontium; the hypothesis of the point of entry in the opposite direction is still being investigated. The larger lateral canals contain pulp and fibers that are closely connected with the main canal (Figure 4-22, A and B).
Influence of Periodontal Disease and Periodontal Treatment on the Endodontium
Some authors agree that the periodontal disease can cause pulp alterations (Craney, 1925; Cahn, 1927; Bauchwitz, 1932; Seltzer and colleagues, 1963; Rubach and colleagues, 1965; Staml, 1966; Bender and Seltzer, 1972; Seltzer, 1975), whereas others believe that periodontal disease cannot affect the pulp (Mazur and Massler, 1964; Smukler and Tagger, 1976; Bergenholtz and Lindhe, 1978; Czarnecki and Schilder, 1979; Torabinejad and colleagues, 1985).
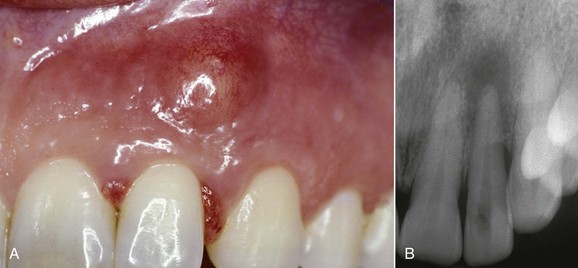
Langeland and co-workers (1974) identified retrograde pulpitis caused by periodontal disease. Retrograde inflammation of the pulp can lead to pulp necrosis. Regarding the influence of the periodontal treatment on the endodontium, Schilder (1978) argued that retrograde pulpitis can be caused by periodontal treatment. For instance, sectioning a vascular pedicle of a large lateral channel with a curette can lead to pulp necrosis. The periodontal treatment can cause pulp necrosis when the blood supply to the pulp through an accessory canal is interrupted by a curette (periodontal curettage—sectioning of a lateral vessel—loss of blood supply resulting in ischemia and pulp necrosis) (Figures 4-24 to 4-26).
Protective Bases
Several materials can be used as protective bases for cavities, such as calcium hydroxide [Ca(OH)2], simple varnishes, cavity liners, Intermediate Restorative Material (IRM), and glass-ionomer cements (GICs) (Figures 4-27 and 4-28).
Why Use a Protective Base?
Why use a protective base? What do we expect from it?
Protective bases aim to do the following:
• Reduce postoperative sensitivity
• Protect the pulp from thermal, chemical, and bacterial stimuli
• Induce the formation of tertiary and pathologic sclerotic dentin
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses