Chapter 34 Premaxilla Surgery: Implant Insertion, Bone Spreading, Nasal Floor Elevation, and Incisive Foramen Implants
INTRODUCTION
Seventeen percent of the U.S. population (30 million adults) has no maxillary natural teeth. A large segment of the population is also missing multiple maxillary anterior teeth, often from trauma or failed fixed partial dentures (FPDs). Therefore the premaxilla is a region often in need of implant abutments for either fixed or overdenture prostheses. In a 20-year review of the literature by Goodacre et al., restorations associated with the edentulous maxillae have the highest early implant failure rate (19% for overdentures and 10% for fixed prostheses). In comparison, mandibular overdentures or fixed restorations have some of the highest implant survival rates (3% failure rate).1
Several factors affect the condition of the edentulous maxilla and may result in a decrease in implant survival or an increase in surgical complications. After tooth loss, the facial cortical plate rapidly resorbs during initial bone remodeling, and the anterior ridge loses 25% of its width within the first year, as well as 40% to 50% within the next 3 to 5 years, mostly at the expense of the labial contour. As a result, the residual available bone migrates to a more palatal position.2–7 The farther forward the maxillary anterior teeth are positioned from the more palatal bone position implants, the greater the moment force leverage on the bone-implant interface, abutment screws, and implants. Coupled with an angled force in both centric and excursions, more stress is transmitted to premaxillary implants than those in anterior mandibles. This often mandates more implants and larger-diameter implants with bone augmentation by bone-spreading or bone graft procedures before or in conjunction with implant placement.
In most patients with available bone, the bone is less dense in the anterior maxilla than in the anterior mandible. The maxilla presents thin porous bone on the labial aspect, very thin porous cortical bone on the floor of the nasal and sinus region, and a more dense cortical bone on the palatal aspect.8,9 The trabecular bone in the premaxilla is usually fine and less dense than the anterior region of the mandible. This usually results in more overload implant failures or crestal bone loss. However, this type of bone lends itself to bone spreading or a compaction technique to insert implants.
In the anterior maxilla, the moderately resorbed bone categories of Division B to C–w often remain narrow almost to the floor of the nose; therefore osteoplasty to gain width is inappropriate. Once the tissues are reflected, the unusual anatomy may confuse the surgeon, and the resultant angulation of implant insertion complicates the restoration of the prosthesis (Figure 34-1). On occasion, osteoplasty to gain bone width results in a Division C–h or D bone volume. The incisive foramen may be used as an implant site in a C–w or C–h bone volume. Nasal elevation and implant insertion may also modify the opposing landmark in C–h bone volume. Therefore unique force factors and implant insertion procedures are more often observed in the anterior maxilla compared with the anterior mandible.
PREMAXILLA EDENTULOUS TREATMENT PLANS
Key Implant Positions
If a patient desires a fixed restoration, implants are required whenever any of the following three combinations of adjacent teeth are missing: (1) the first premolar, canine, and lateral incisor; (2) the canine, lateral incisor, and central incisor; and (3) the canine, first premolar, and second premolar. When any of these conditions exist, a fixed restoration is contraindicated because of the length of the span (three pontics), the amount of force (forces greater in the canine region compared with the anterior region), and the direction of the force (angled forces to the canine region).10
PREMAXILLA ARCH FORM AND IMPLANT NUMBER
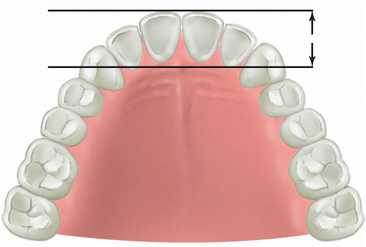
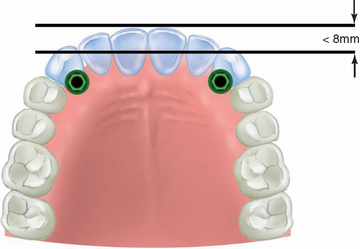
The distance between two horizontal lines, drawn from the two canine tips and the facial of the central incisors, determines the dental arch form in the anterior maxilla. (Figure 34-2). A distance less than 8 mm corresponds to a square dental arch form. Lateral and central incisors are not cantilevered very much facially from the canine position, and therefore mandibular excursions and occlusal forces exert less stress on the canine implants. Implants in the canine positions to replace the six anterior teeth may suffice when the force factors are low and if they are splinted to additional posterior implants (Figure 34-3).
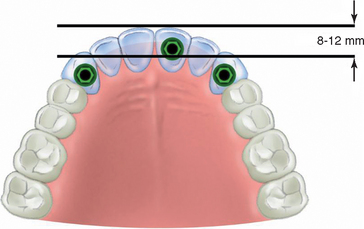
An ovoid dentate arch form corresponds to a distance from the canine to central incisor horizontal lines between 8 and 12 mm. At least three implants should be inserted into the premaxilla, one in each canine and preferably one in a central incisor position (Figure 34-4). The central incisor position increases the anteroposterior (A-P) distance from the canine to central and provides improved biomechanical support to the prosthesis. In long-term edentulous maxillae, this most likely will require bone augmentation before implant insertion (Figure 34-5). When patient force factors are low to moderate, the anterior implant may be positioned in a lateral incisor site.
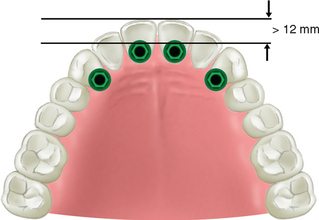
When the distance between the canine and central incisor horizontal lines is greater than 12 mm, the dentate arch form is tapering and the restoration of a tapered dental arch form places the greatest forces on anterior implants, especially during mandibular excursions (Figure 34-6). The anterior teeth create a significant facial cantilever from the canine position. As such, four implants should be considered to replace the six anterior teeth. When more than six anterior teeth are missing, additional posterior implants should also be splinted to the anterior segment (Figure 34-7).
As a consequence of bone resorption, the residual ridge form becomes more squared. The edentulous ridge arch form may be different from the dentate arch form (which is determined by the final teeth position in the premaxilla and not the arch shape of the residual ridge). The number and position of implants are related to the arch form of the final dentition (restoration), not the existing edentulous arch form. The worst-case scenario is a patient requiring restoration of a dental tapered arch form with a square residual ridge form. When force factors are greater than usual in any arch form, four implants in the premaxilla should be splinted together and share any lateral forces during excursions. In this patient condition, four implants in the premaxilla are required to compensate for the cantilevered anterior tooth position. These implants should be connected to additional posterior implants, preferably to include implants as far distal as the second molar sites, to increase the A-P position of the implants (Figure 34-8).
Restorations with posterior pontics that are cantilevered should not be placed on maxillary anterior implants. The forces are two to five times greater in the posterior regions compared with the anterior region of the mouth. A cantilever magnifies these higher bite forces. As a result, the anterior implant abutments with a cantilever may receive a tenfold greater load compared with implants without a cantilever. If posterior teeth also are being replaced in the prosthesis, then additional implants are required. Seven to 10 implants often are inserted to restore a completely edentulous maxilla with a fixed prosthesis, especially when opposing natural dentition or a fixed restoration.
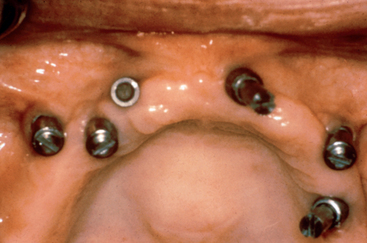
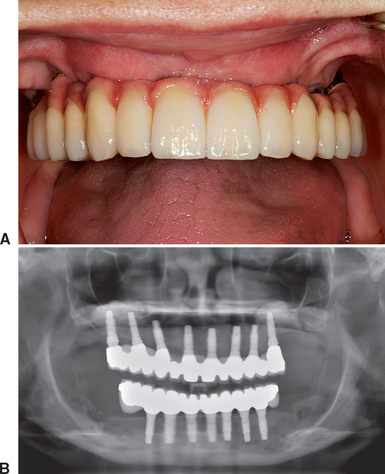
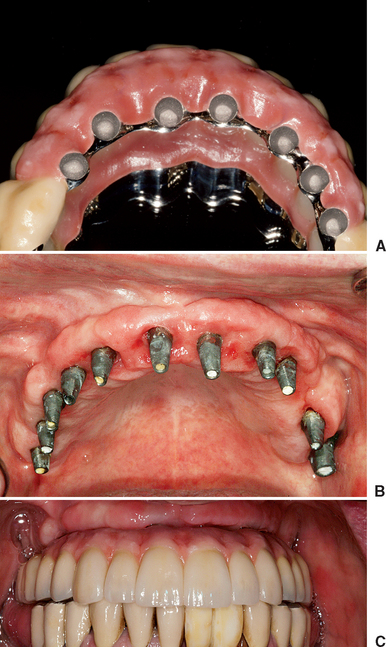
It should be noted that most full-arch maxillary prostheses are FP-3 fixed restorations or RP-4 overdentures. In either scenario, mesiodistal implant position does not have to strictly correlate with tooth position. The faciopalatal position may also be more flexible, because the emergence profile of the prosthesis is usually outside of the esthetic zone and because the gingival aspect of the restoration separates the clinical crown from the implant site. As such, the implant sites are determined more for biomechanics, interimplant spacing, or available bone, rather than a strict tooth position (as in an FP-1 prosthesis) (Figures 34-9 and 34-10).
MULTIPLE ANTERIOR IMPLANT DIAMETER
Several conditions should be considered for the proper implant diameter: tooth size, distance from an adjacent tooth, interimplant distance, facial bone dimension, and loading forces. A primary factor for the implant size when multiple anterior teeth are missing is the distance between the adjacent teeth or implants. The horizontal dimension of a wedge-shaped bone defect around an implant at the crest of the ridge from the biological width, implant design, or occlusal overload ranges from 0.5 to 1.4 mm.11,12 Therefore when implants are placed adjacent to each other, a minimum interimplant distance of 3 mm is suggested to accommodate for eventual crestal bone loss and maintain interseptal bone levels.11 This is of importance for an FP-1 restoration because the interseptal bone height in part determines the incidence of presence or absence of a lack of interdental papillae between the teeth or implants, with the most ideal results having a distance of 5 mm or less from the interproximal bone to the interproximal crown contact.13,14
Implants with 3 mm or greater interimplant space permit the development of papilla between the implants. When two adjacent teeth are missing in the premaxilla, the natural teeth adjacent to the edentulous span provide the interdental papilla support for proper esthetics, and an FP-1 restoration is often fabricated (Figure 34-11). However, the interdental papilla between the two implants is more difficult to restore.
The usual range of interimplant papillary height is 2 to 4 mm, even when the implants are 3 mm or more apart.15 Therefore when an FP-1 restoration is desired, the prosthesis design (square-tooth forms) and implant positions may need to be altered accordingly to improve the esthetic result (Figure 34-12). Implants less than 3 mm apart often have a depressed interimplant papilla. As a result the crown contour is modified to a square form to lower the interproximal contact to the soft tissue. Although this technique reduces the black triangular space over the papilla, it is not an ideal result (Figure 34-13).
When four anterior adjacent teeth are missing, the soft tissue drape is usually inadequate to restore the height of the interimplant papillae; therefore the anatomy rarely permits an FP-1 prosthesis design. FP-2 or FP-3 prostheses are most always fabricated, dependent on the high lip dynamics of smiling within the esthetic zones (Figure 34-14).
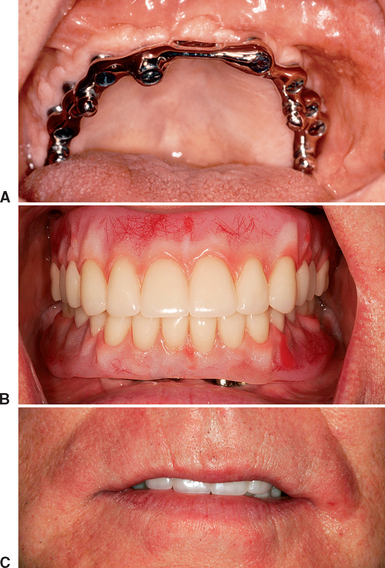
MAXILLARY OVERDENTURE TREATMENT PLANS
The edentulous maxilla has the lowest implant survival for removable implant restorations.1,16,17 All reports concur that maxillary bone tends to be of poorer quality and volume and presents several biomechanical disadvantages. To compensate for the poor local conditions, a greater number of implants should be treatment planned, along with a greater A-P distance. With these concerns in mind, the minimum implant number for a completely edentulous maxillary overdenture prosthesis is four implants splinted in the premaxilla. The most usual sites are one central (or lateral) incisor position, bilateral canine positions, and at least one in the contralateral central or premolar site. Additional implants are often indicated when force factors are greater or for a RP-4 prosthesis overdenture.
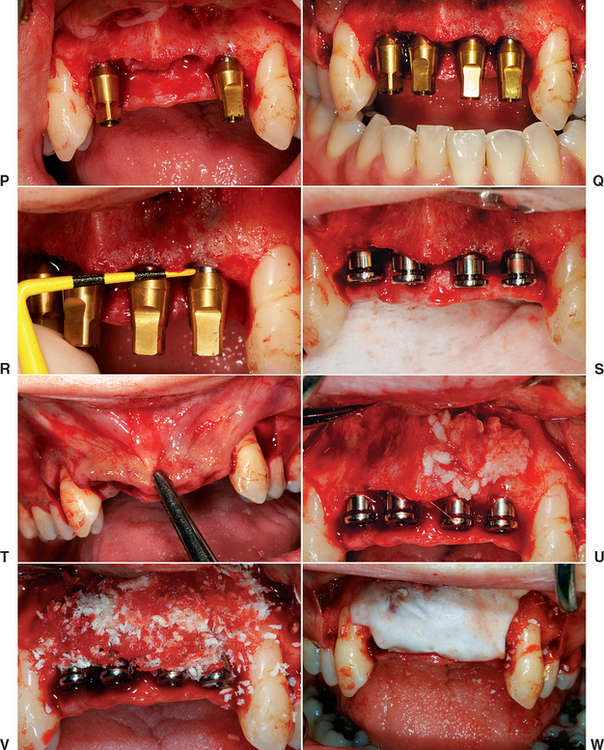
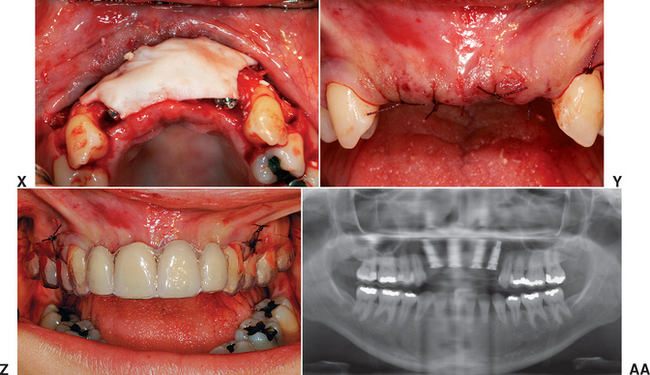
PREMAXILLA SURGERY
Maxillary Lip Support
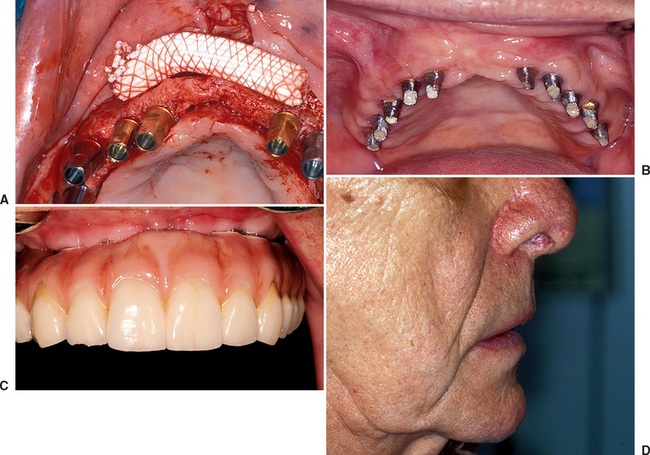
The maxillary lip support above a fixed prosthesis should be evaluated before surgery. The maxillary lip should be more facial than the mandibular lip at repose, yet a depressed philtrum should be maintained, especially in a younger patient. As a general rule, when a vertical line is drawn along the patient profile, the maxillary lip should be 1 to 2 mm in front of the lower lip, and the chin should be 2 mm behind the lower lip position when the patient has the jaw in a vertical rest position. If the patient wears a labial flange on the removable prosthesis that provides acceptable maxillary lip support, or one exists at the prosthetic try-in, and a fixed prosthesis is desired, then a soft tissue template may be fabricated from the removable prosthetic try-in to indicate the soft tissue support required (Figures 34-15 and 34-16).
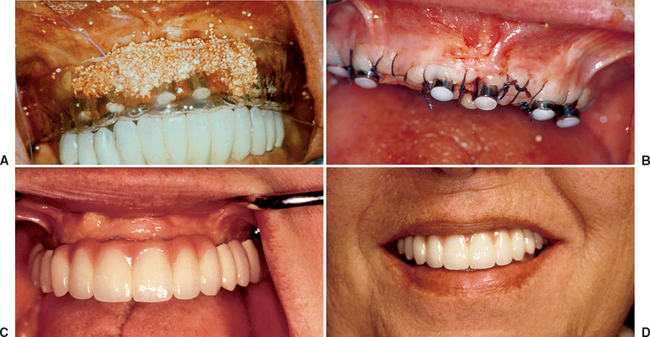
When the maxillary lip requires greater horizontal support, yet adequate bone is present to place implants, an acellular tissue graft (AlloDerm) and/or or dense hydroxyapatite (HA) graft may be used on the facial aspect of the bone before closure of the soft tissue over the implant (Figure 34-17). A bone graft may be used to support the maxillary lip above the prosthesis. This is often indicated when insufficient bone is present for the proper implant size, position, and/or number (Figure 34-18). The added labial tissue thickness will support the maxillary lip above the cervical regions of the teeth, increase the crestal tissue thickness, and improve ridge contour. In addition, the soft tissue augmentation to support the maxillary lip may also create sufficient volume of tissue to allow the sculpture of an interdental papilla around the implant crowns at stage II uncovery.
An RP-5 or RP-4 prosthesis does not require bone, HA, and/or AlloDerm to support the maxillary lip. Instead the flange of the overdenture may be designed similarly to a traditional denture to support the lip (Figure 34-19).
Division A Premaxilla
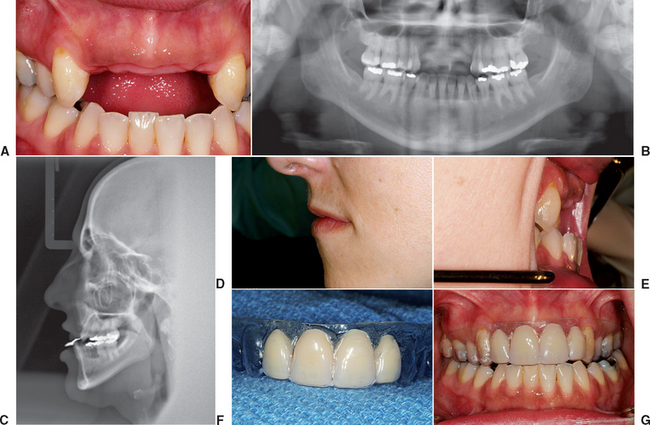
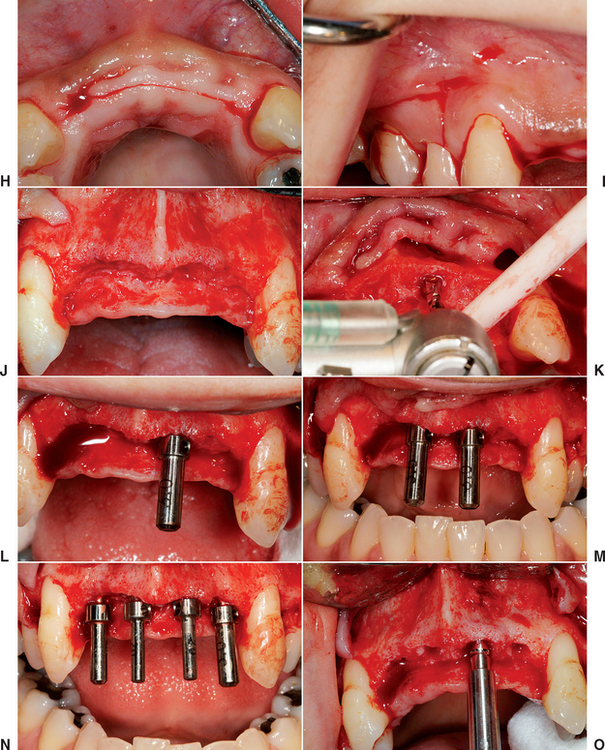
The maxillary anterior root form surgery with Division A bone is similar to that described in the maxillary anterior single-tooth implant (see Chapter 33). For a successful placement of standard-diameter endosteal implants in the Division A anterior maxillary region, the recipient bone bed should be greater than 6 mm wide, greater than 12 mm high, and have a crown/residual bone height ratio less than 1.
When ideal anterior bone is present and the treatment plan is for an FP-1 prosthesis, a surgical template should identify the incisal edges and the mesiodistal tooth position of the final prosthesis. This template should be designed to rest on adjacent teeth (when present) or on the reflected ridge with a computed tomography (CT) bone model or index of the lower teeth to aid in correct positioning for the edentulous maxilla (Figure 34-20, A to G). The soft tissue crestal incision may be made on the lingual aspect of the edentulous ridge, providing additional keratinized tissue to the facial aspect (Figure 34-20, H). A vertical-release incision most often is made distal to the last tooth in each quadrant and includes the interdental papilla (Figure 34-20, I). When the mesial papilla is ideal, a “papilla-saving” incision may be medial to the papilla, similar to a single-tooth site.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses