CHAPTER 34
Eminectomy
Joseph P. McCain1 and Reem Hamdy Hossameldin2
1Private Practice; Baptist Health Systems; and Oral and Maxillofacial Surgery, Herbert Wertheim College of Medicine, Florida International University Miami, Florida, USA; and Nova Southeastern School of Dental Medicine, Fort Lauderdale, Florida USA
2Department of Oral and Maxillofacial Surgery, Faculty of Dental Medicine, Cairo University, Cairo, Egypt; and General Surgery Department, Herbert Wertheim College of Medicine, Florida International University, Miami, Florida, USA
A procedure performed to correct chronic dislocation or closed lock of the mandible with surgical reduction of the articular eminence.
Indications
- Habitual chronic dislocation of the mandible, where all conservative and minimally invasive methods are either unsuccessful or contraindicated
- Treatment of closed lock of the temporomandibular joint (TMJ) (modified eminectomy)
Contraindications
- Chronic mandibular dislocation cases involving a shallow articular eminence
- Radiological evidence of a pneumatized eminence (increased risk of infection as a result of communication between the joint space and the mastoid air cells)
- Radiographic evidence of a vascularized eminence (intracranial hemorrhage)
Anatomy
-
Superficial temporal vessels: Emerge from the superior aspect of the parotid gland and accompany the auriculotemporal nerve (Figure 34.1). The superficial temporal artery (STA) arises from the parotid gland as a bifurcation of the external carotid artery (ECA). The STA is a common source of bleeding during approaches to the TMJ. The superficial temporal vein lies superficial and usually posterior to the artery.
- Transverse facial vessels: Branch off of the superficial temporal vessels and course inferior and relatively parallel to the zygomatic arch (Figure 34.1).
- Auriculotemporal nerve: Courses from the medial aspect of the posterior neck of the condyle and turns superiorly, coursing superficial to the zygomatic root of the temporal bone (Figure 34.1). Just anterior to the auricle, the nerve divides into its terminal branches within the skin of the temporal area. The auriculotemporal nerve accompanies, and is posterior to, the STA. Pre-auricular exposure of the TMJ area almost always invariably injures this nerve. Damage is minimized by incision and dissection in close apposition to the cartilaginous portion of the external auditory meatus. Temporal extension of the skin incision should be located posteriorly so that the main distribution of the nerve is dissected and retracted forward within the flap. Patients rarely complain about sensory disturbances that result from damage to the auriculotemporal nerve.
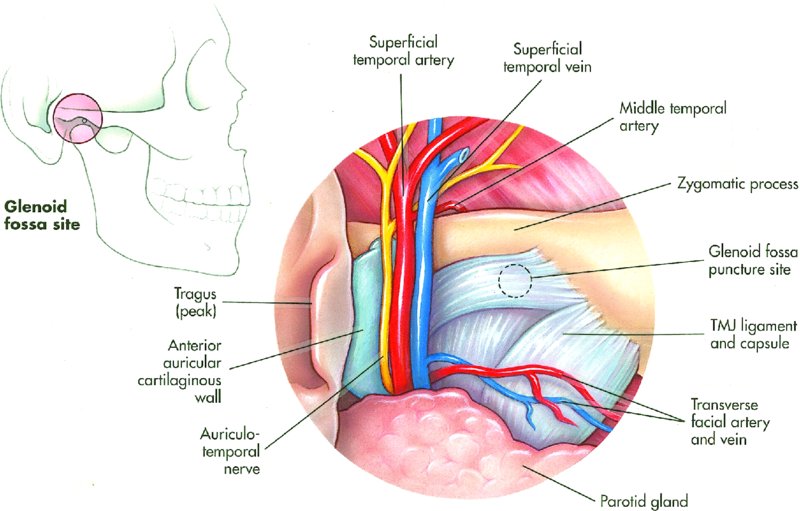
Figure 34.1. Image depicting the orientation of the superficial temporal artery and vein, auriculotemporal nerve, and transverse facial artery and vein at the root of the zygoma.
Pre-auricular Dissection Layers
- Temporoparietal fascia (superficial temporal fascia): The temporoparietal fascia, which is the most superficial fascia layer beneath the subcutaneous fat, is the lateral extension of the galea and is continuous with the superficial musculoaponeurotic layer (SMAS). The blood vessels of the scalp, such as the superficial temporal vessels, run along its superficial aspect closely related to the subcutaneous fat. Motor nerves, such as the temporal branch of the facial nerve, run on the deep surface of the temporoparietal fascia.
- Subgaleal fascia: The subgaleal fascia within the temporoparietal region is well developed and can be dissected as a discrete fascial layer if desired, but it is usually used only as a cleavage plane in the standard pre-auricular approach.
- Temporalis fascia (deep temporal fascia): The dense, white fascia overlying the temporalis muscle. This thick fascia arises from the superior temporal line and fuses with the pericranium. The temporalis muscle arises from the deep surface of the temporal fascia and the whole of the temporal fossa. Inferiorly, the temporal fascia splints into a superficial and a deep layer above the zygomatic arch. A small quantity of fat between the two layers is referred to as the superficial temporal fat pad. A large vein frequently runs just deep to the superficial layer of temporalis fascia.
Technique
- The patient is placed supine on the operating room table and nasally intubated.
- The patient is prepped and draped, allowing for visualization of the entire ear and lateral canthus of the eye. The pre-auricular hair is shaved, and the remainder of the patient’s hair is positioned under a surgical head cap. An ear wick soaked in antibiotic solution is placed within the external auditory canal.
- No local anesthetic or vasoconstrictors are injected.
-
The pre-auricular incision is marked along an actual skin crease, contouring the incision around the tragal cartilage (Figure 34.5 [all figures cited in this list appear in Case Report 34.1]). The incision originates at the top of the ear and extends just inferior to the tragal cartilage. The incision does not extend to the pinna. The incision initially transverses skin and subcutaneous tissue only (Figure 34.6). Small bleeding points are cauterized with needlepoint cautery at the coagulation mode of 20.
- The dissection can be divided into thirds. The upper third is performed first. A curved hemostat is used to dissect bluntly through the horizontal auricular muscles down to the glistening white temporalis fascia (Figure 34.7). The neurovascular bundle is kept forward. Occasionally, a horizontal vessel is encountered arising from the superficial temporal artery or vein that crosses the dissection site (transverse facial vessels) and requires cauterized or suture ligation. Once the glistening white temporalis fascia is identified, a Messer retractor is placed to confirm that position and to reflect the flap anteriorly.
- The second part of the dissection is within the lower third of the incision. The tragal cartilage is skeletonized (Figure 34.8) to its apex with a curved hemostat. A small tag of tissue may be retained (4 to 6 mm) along the tragal cartilage to provide a point to place subcutaneous sutures during closure. With the upper and the lower aspects of the dissection completed, two points of depth are established: one within the superior third of the dissection at the level of the temporalis fascia, and a second at the inferior third of the dissection at the level of the tragal cartilage apex that goes to the capsule.
- The third part of the dissection connects the middle third of the incision to the superior and inferior thirds of the dissection (Figure 34.9). Sharp dissection proceeds through the horizontal auricular muscles to expose and connect the temporalis fascia with the superior dissection and the tragal tip with the inferior dissection.
-
A periosteal elevator is utilized in a sweeping motion to flap forward the tissue within the layer superficial to the temporalis fascia (Figure 34.10). A sharp incision from the apex of the tragal cartilage to the superior aspect of the incision is made. Methylene blue mark can be used to mark the incision site (Figure 34.12). The Messer retractor is used to pull the flap superior to allow for a release of the temporalis fascia so that the skin incision does not need to be extended for additional exposure. The incision extends from the tip of the tragal cartilage, superiorly through the temporalis fascia and temporalis muscle, and down to bone (Figure 34.13). The temporalis muscle is transected with the cautery/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


