CHAPTER 31. Endocrine disorders and pregnancy
ANTERIOR PITUITARY HYPERFUNCTION – GIGANTISM AND ACROMEGALY
Overproduction of growth hormone by the anterior pituitary during the period of skeletal growth causes gigantism. Overgrowth of the skeleton and soft tissues causes the patient to become a giant. Acromegaly usually develops later.
After the epiphyses have fused, an adenoma of growth hormone cells causes acromegaly. There is renewed growth, particularly of the jaws, hands and feet. The condylar growth centre becomes active and the mandible becomes enlarged and protrusive (Fig. 31.1). Radiographically, the whole jaw is lengthened and the angle becomes more oblique (Fig. 31.2). The jaw and other bones are also made thicker by subperiosteal bone deposition. The teeth become spaced or, if the patient is edentulous, dentures cease to fit the growing jaw. The hands and feet become spade-like (Fig. 31.3). Overgrowth of soft tissues causes thickening and enlargement of the facial features, particularly the lips and nose.
 |
| Fig. 31.1
Acromegaly. The typical facial appearance, resulting from excessive mandibular growth.
|
 |
| Fig. 31.2
Acromegaly. The mandible is enlarged with an elongated ramus and increased obliquity of the angle. The pituitary fossa is also enlarged due to the tumour causing the disease.
|
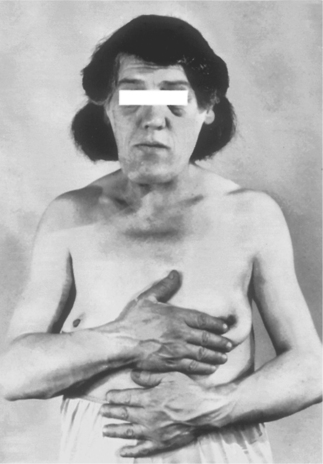 |
| Fig. 31.3
Acromegaly. The jaw is enlarged and protrusive, the features thickened and the hands broad and spade-like. (Taken before the advent of colour photography.)
|
Headaches and visual disturbances due to the pituitary tumour are common. Later, weakness and often diabetes mellitus develop. Blindness due to pressure of the tumour on the optic chiasma may develop. Hypertension is common and may be associated with cardiomyopathy and dysrhythmias. Irradiation or trans-sphenoidal resection of the pituitary tumour may relieve the symptoms.
Dental considerations
Orthognathic surgery may be considered to improve the appearance. There is a risk of postoperative airways obstruction, particularly because the glottis is narrowed and the large tongue may press back on to the pharynx. Close observation is therefore needed to release the dental ligatures in emergency or asphyxia will result. Systemic complications as described above can also affect dental management. Otherwise, there is no special risk from local analgesia or sedation.
THYROID DISEASE
Hyperthyroidism
Hyperthyroidism (Box 31.1) is most common in young adults, particularly women. There is usually a diffuse goitre and the disease is typically autoimmune with thyroid-stimulating autoantibodies. Less frequently, the cause is a toxic (hyperthyroid) goitre due to hormone-producing adenomas.
Box 31.1
Important features of hyperthyroidism
• Irritability and anxiety
• Loss of weight
• Exophthalmos (Fig. 31.4)
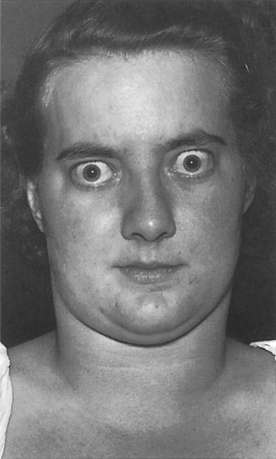 |
| Fig. 31.4
Thyrotoxicosis. Exophthalmos is typical but the enlarged thyroid is not conspicuous. The patient had not then started to lose weight. (Taken before the advent of colour photography.)
|
• Tachycardia
• Cardiovascular disease, particularly in untreated hyperthyroidism in older patients
Dental considerations
Treatment of hyperthyroid patients may be affected by several factors (Box 31.2) and, in particular, may be made difficult because of excitability and anxiety. Excessive cardiac excitability is only a theoretical contraindication to lidocaine with epinephrine and no other local anaesthetic has been shown to be safer. Conscious sedation (nitrous oxide and oxygen) is frequently helpful, but benzodiazepines may potentiate antithyroid drugs.
Box 31.2
Dental management of hyperthyroid patients
• Control of nervousness and excitability
• If clinical signs are seen but the patient is not under treatment, refer to a physician
• Avoid general anaesthesia in patients with longstanding thyrotoxicosis, particularly older patients
Hypothyroidism
Cretinism
Cretinism results from deficient thyroid activity at birth (Fig. 31.5). It is most common in areas of endemic goitre, but rare now that goitre is controlled with iodine. A cretin is occasionally the offspring of a normal mother. The main features are particularly short stature and intellectual impairment, but dental abnormalities are frequently associated (Box 31.3). In the untreated patient, sedatives and tranquillisers such as benzodiazepines can precipitate myxoedemic coma and should generally be avoided. Conscious sedation with nitrous oxide and oxygen can be given.
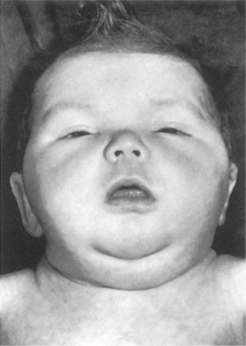 |
| Fig. 31.5
Cretinism in a child. The facial expression, excessive broadening of the features and the protruding tongue are characteristic. (Taken before the advent of colour photography.)
|
Box 31.3
Typical features of cretinism
• Skeletal development and dental eruption greatly delayed
• Impaired mental development
• Broad, rather flat face partly due to defective growth of the skull and facial bones
• Overlarge, protrusive tongue
• Dull facial expression, dry thick skin
• Short stocky build and, often, umbilical hernia
Treatment with thyroid hormone must be begun early to provide normal physical development and improvement in the mental defect.
Adult hypothyroidism
Hypothyroidism (Box 31.4) is frequently autoimmune, but can follow radioiodine treatment or excessive surgical removal of thyroid tissue for hyperthyroidism.
Box 31.4
Typical features of adult hypothyroidism
• Weight gain
• Slowed activity and thought
• Dry skin and hair loss
• Intolerance of cold
• Susceptibility to ischaemic heart disease
Aspects of dental management of hypothyroidism are summarised in Box 31.5.
Box 31.5
Dental management of hypothyroidism
• Avoid sedatives including diazepam, opioid analgesics and general anaesthetics because of the risk of myxoedemic coma
• Anaemia or ischaemic heart disease may require modification of dental treatment
• Local anaesthesia always preferable
• Nitrous oxide/oxygen sedation acceptable
• Sjögren’s syndrome occasionally associated and requires treatment
Lingual thyroid
Thyroid tissue is occasionally present in the tongue as a result of imperfect descent of the anlage into the neck. Females are mainly affected. Clinically, it usually causes an asymptomatic midline, purplish soft swelling, but may cause dysphagia. It may not be recognised for thyroid tissue until after biopsy which may cause considerable bleeding. Otherwise, the nature of the swelling may be determined by I 131 or technetium scanning, or by CT or MRI. Scanning of the neck to ensure the presence of a thyroid gland is therefore essential before the lingual thyroid is removed. However, this may have to be done anyway if it is causing significant obstruction. If no normally positioned thyroid tissue is present, life-long thyroxine supplementation is then given. Malignant change in ectopic thyroid is rare.
PARATHYROID DISEASE → Summary p. 173
Hyperparathyroidism
This uncommon disease is usually caused by an adenoma of the parathyroids. Secondary hyperparathyroidism is a reaction to low serum calcium levels caused by chronic renal failure or prolonged dialysis. Parathormone overproduction can cause decalcification of the skeleton and cyst-like areas of bone resorption (osteitis fibrosa cystica). These lesions are giant cell ‘tumours’, but are rarely seen now that hyperparathyroidism is recognised earlier by its non-specific symptoms (Ch. 10). As discussed below, hyperparathyroidism is the presenting sign of the uncommon disease, type 1 multiple endocrine neoplasia syndrome (see below).
Typical features of hyperparathyroidism are summarised in Box 31.6
Box 31.6
Typical features of hyperparathyroidism
• General malaise
• Peptic ulceration
• Bone resorption
• Renal stones or nephrocalcinosis
• Polyuria
Hyperparathyroidism-jaw tumour syndrome
Hyperparathyroidism-jaw tumor syndrome is a rare autosomal dominant disease. Its gene location is 1q21-q32 whose function is a tumor-suppressor gene whose product is parafibromin. The features include parathyroid adenomas or carcinomas, renal cysts and fibro-osseous jaw lesions. Renal, mixed and uterine tumours may be associated.
Jaw lesions are typically multiple and can involve both mandible and maxilla. Unlike sporadic hyperparathyroidism, giant cells are not the main feature. The lesions are fibro-osseous and may resemble ossifying or cementifying fibroma, non-ossifying fibroma, or even fibrous dysplasia. However, their essential features are a cellular fibrous stroma, sometimes with a suggestion of a storiform pattern containing trabeculae of bone or cementicle-like particles. Only a few giant cells may be seen among bone trabeculae. The lesions are typically sharply demarcated.
In terms of management, the main problem is that of the parathyroid and other tumours. Parathyroid adenomas usually respond to surgery, but management of parathyoid carcinoma is more difficult. The prognosis is also affected by the behaviour of associated tumours of the kidneys or uterus. Jaw lesions usually shell out quite readily but some have recurred. Otherwise, they may regress spontaneously after removal of the parathyroid tumour, though this may take months or even years.
Hypoparathyroidism
Post-surgical hypoparathyroidism
The most common cause of hypoparathyroidism is thyroidectomy. The resulting hypocalcaemia causes heightened neuromuscular excitability and tetany. These are controlled by giving the vitamin D analogue 1,25-dihydrocholecalciferol (DHCC) orally. Later, any residual parathyroid tissue undergoes compensatory hyperplasia.
Tetany
In mild cases, tetany is latent but can be triggered by tapping on the skin over the facial nerve; this causes the facial muscles to contract. In more severe cases, muscle cramps and tonic contractions of the muscles may progress to generalised convulsions. An early symptom of tetany is paraesthesiae of the lip and extremities. Tetany more frequently results from overbreathing, often neurotic in origin (hyperventilation syndrome).
Idiopathic hypoparathyroidism
Early-onset hypoparathyroidism is rare. It sometimes forms part of the polyendocrinopathy syndrome with autoantibodies to a variety of glandular tissues and deficiency states (particularly Addison’s disease) and, frequently, mucocutaneous candidosis (see below)./>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


