Chapter 3
Preservative Operative Intervention. How to Intervene?
Aim
Deciding how best to intervene and prepare teeth if operative management of dental caries is indicated is an everyday scenario for the practitioner. The aim of this chapter is to consider several techniques for preparing teeth for the placement of a direct restoration.
Outcome
This section familiarises practitioners with:
-
how to intervene and prepare teeth
-
traditional tooth preparation techniques
-
micro-preparation techniques
-
chemomechanical methods of caries removal
-
sonic tooth preparation
-
air abrasion
-
the use of magnification.
Tooth Preparation
The general overriding principle when operative intervention is indicated is that ideally the preparation should be only as large as the lesion itself. It is anticipated that the strict requirement to remove all caries (i.e. affected but uninfected dentine) is changing, although it is currently accepted practice to remove all softened dentine and to ensure the amelodentinal junction (ADJ) is clear of caries once tooth preparation is complete.
Occlusal preparation
Information about the extent and depth of the lesion can be gained from any pre-operative radiographs that are available. Whilst this is useful, it is important to remember that this is always an under-representation of the true extent of the lesion. The lesion is accessed with a bur and the preparation extended until all affected fissures have been removed and the ADJ appears normal, with no visual evidence of caries. Sound fissures are not removed and if two lesions are present they are treated separately.
Fissures that are decalcified but not cavitated at the edge of the lesion can be left and the fissure sealed after the restoration has been placed, or as part of the restorative process. If amalgam is used, a cavosurface margin of 90–110° is required. Undermined enamel at the margins should be removed, as the restorative material will not support it, with possible fracture subsequently. In contrast, preparations for resin composite require the removal of friable enamel only, as unsupported, but firm enamel can be supported by the restorative material and may be left.
Bevels at the margins of the preparation are contraindicated for either material as they result in thin sections of the material at the preparation margin. These can fracture off under normal occlusal loading, providing a niche for stain build-up or acting as a plaque-retention factor. Another practitioner might misdiagnose these stained marginal fractures as secondary caries and replace the restoration unnecessarily.
Fissure sealing of minimal occlusal resincomposite restorations is good practice and places the unaffected fissures out of reach of further carious attack if the sealant is placed carefully. Any early initial caries in the fissure will “burn out” as further substrate in the form of fermentable carbohydrate is denied to the lesion. It has also been shown that there is some advantage in terms of enhanced longevity to fissure-sealing teeth after amalgam restorations have been placed using an unfilled resin system.
In theory, amalgam restorations require an undercut to retain them and traditionally this was built into preparations with inverted cone burs. In practice, if fissure burs are used, the nylon chuck of the modern air turbine hand-piece allows the bur to rotate eccentrically and undercut is automatically incorporated into the preparation during tooth preparation. It is preferable, however, to use a small pear-shaped bur, which will by its very nature preserve occlusal tissue and build in undercuts. A pear-shaped bur has a shape similar to that of the lesion of caries. The continued use of inverted cone burs will further weaken cusps in teeth with large occlusal and/or proximal preparations, especially if there are buccal and lingual or palatal extensions to the preparation. Consequently, their continued use cannot be justified.
Proximal preparations in posterior teeth
Lesions of proximal caries in posterior teeth are notoriously difficult to treat, especially at the initial stage, with damage to adjacent teeth relatively common when proximal lesions are prepared with traditional techniques. It is important to distinguish between occlusal and proximal preparations in that a proximal preparation may have an occlusal dimension, but frequently there is no occlusal caries. The belief that occlusal dovetails are required for retention of proximal amalgam restorations is no longer valid. Whilst adjacent occlusal and proximal lesions that have coalesced in premolar teeth are often treated together for convenience, this is not the case for permanent molar teeth in that a lower molar may have up to four restorations: namely, one or two proximal and one or two occlusal restorations.
The options for accessing a proximal lesion in a posterior tooth include approaching the lesion from the following directions:
-
Occlusally, by cutting through the marginal ridge.
-
Occlusally, leaving the marginal ridge intact via a tunnel preparation.
-
Buccally or lingually. This is usually limited to situations where teeth are tilted lingually and where an occlusal approach would result in the removal of considerable sound tooth substance.
-
Directly as a single surface, which is possible if the adjacent tooth is missing. In this case, the tooth is prepared in the same way as for the treatment of cervical or smooth surface caries.
The majority of proximal lesions are accessed from an occlusal direction, which is probably because the majority of dental schools have traditionally recommended this approach. It is helpful to consider whether it is necessary to remove the marginal ridge to access the lesion and explore whether a buccal or facial approach is possible. Tunnel approaches to access proximal lesions are technically difficult and tend to be unsuccessful in the long term, especially in premolar teeth, with fracture of the marginal ridge being a common clinical finding. Concerns have also been expressed about an operator’s ability to clear the ADJ in the coronal part of the proximal preparation of caries, let alone adequately adapt the restorative material to the preparation to ensure a good tooth-restorative marginal seal – which is most important if there is some residual caries left in the preparation.
The preparations for amalgam and resin composite restorations are subtly different. However, it is still a prerequisite to break through the contact point and into the embrasure such that all contact with the adjacent tooth is removed. A common fault is not to break through the contact point. This is problematic as caries by definition is always found below the contact point.
Proximal preparations for a resin composite restoration should have a scoop form produced using a pear-shaped bur. The proximal walls are bevelled with a reciprocating handpiece or gingival margin trimmers extending the preparation just into the embrasure. Again, all friable enamel is removed but firm unsupported enamel can be left, as the restorative material will support this. No further additional preparation is required to enhance retention.
Preparations for amalgam restorations, in contrast, have a scoop-box form, which converges towards the occlusal aspect of the preparation. Again, the preparation just extends into the embrasure, although the requirement to have a certain depth (1.5 mm) of amalgam and a cavosurface margin of 90-110° makes the preparation necessarily more destructive than that required for a resincomposite restoration placed to restore a similar-sized lesion. For this reason alone, the use of amalgam in the initial operative management of an early proximal lesion that requires restoration cannot be justified. All unsupported enamel is removed, ideally with hand instruments (for example, gingival margin trimmers or alternatively safe-sided sonic preparation tips) as the use of burs to adjust proximal margins can result in damage to the adjacent tooth. If the preparation includes an occlusal lesion so that a mesio or disto-occlusal restoration is planned, further retention features are unlikely to be required. If, however, there is no occlusal lesion (i.e. a slot preparation where the marginal ridge has been removed for access to the proximal lesion), it is necessary to incorporate additional retention features in the form of retention grooves in the buccal and lingual walls of the proximal box. These grooves are prepared with a small rose-head slow-speed bur. No further preparation, other than careful finishing of the margins, is necessary.
Proximal preparations in anterior teeth
Anterior proximal lesions are universally restored with a tooth-coloured restorative material and the tooth is prepared accordingly. The lesions can be accessed:
-
Labially or lingually/palatally. A lingual or palatal approach is preferable as it leaves the buccal enamel intact. If a buccal approach is indicated, it is important to minimise the buccal extent of the restoration, as the material will be susceptible to staining and discolouration. Note that unsupported buccal enamel can be left, providing it is not friable, as the restorative material will support the tooth tissue if resin-bonded. For this reason the use of resin composite is strongly recommended in anterior proximal lesions.
-
Directly as a single surface, which is possible if the adjacent tooth is missing. In this case, the tooth is prepared in the same way as in the treatment of cervical or smooth surface caries.
Cervical or smooth surface preparations
These lesions only require operative intervention when attempts to arrest the lesion have failed and there is evidence of cavitation and/or lesion progression. Operative intervention is limited to accessing the lesion and extending the preparation until the ADJ is clear of caries. Caries in the deeper aspects of the preparation can then be addressed accordingly.
Managing Deep Caries
It is now accepted that in an established carious cavity softened dentine precedes discoloured dentine, which precedes infected dentine. The speed at which an individual lesion advances depends on the extent to which the effect of bacterial acids and proteases are opposed by pulpal fluid pressure, and dentine permeability. It should be noted, however, that dental caries must be within 0.5 mm of the pulp before hyperaemia and/or pulpitis will occur. It is always preferable to manage a lesion without exposing the dental pulp, possibly by using an indirect pulp-capping technique. Direct pulp-capping techniques are required when the pulp is exposed by trauma or caries. Carious exposures can be reduced by a stepwise approach to caries excavation (Fig. 3-1).
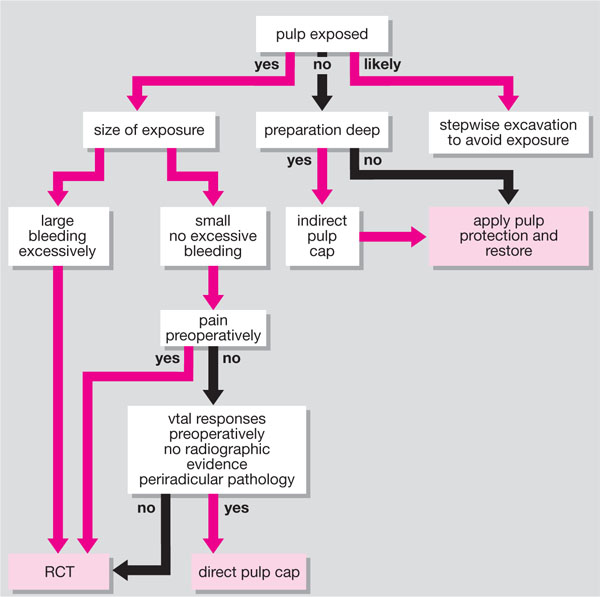
Fig 3-1 Algorithm for the management of deep caries.
Direct pulp capping
Direct pulp capping is defined as the application of material (usually hard-setting calcium hydroxide cement) to a pulp exposed by caries or trauma. This procedure is more likely to be successful if there is no history of recurring or spontaneous pain and preoperatively there is:
-
“normal” vitality
-
absence of tenderness to percussion
-
no radiographic evidence of periradicular pathology
-
clinically a pink pulp is found, which bleeds if touched but not excessively.
The age of the pulp is also important in that younger pulps are more likely to respond positively to direct pulp-capping techniques. Biologically young pulps can be identified radiographically by an obvious pulp chamber and patent root canals. The previous restorative experience of a tooth is equally important.
Teeth with a history of pain are more likely to have bacterial invasion of the pulp and these teeth will inevitably require endodontic therapy. The position of the exposure will have an effect on the success of the procedure. The exposure should have no pulp chamber coronal to it. A cervical lesion, for example, if treated with a direct pulp cap, will heal by laying down reactionary dentine, which will interrupt the blood supply to the coronal pulp tissue leading to necrosis. If there is pulp chamber coronal to the exposure it would be sensible to consider endodontic therapy, as failure to initiate endodontics may result in a worsened prognosis due to dystrophic calcification.
The material of choice for direct pulp capping is hard-setting calcium hydroxide cement, although there is currently considerable interest in mineral trioxide aggregate (MTA) as a pulp-capping agent. It has superior therapeutic properties when compared with hard-setting calcium hydroxide cement, but it is difficult to handle and currently has a long setting reaction, which may be considered to limit its use as a pulp-capping agent.
There is little information in the literature regarding success rates for direct pulp-capping treatments. It would seem that success rates are higher for traumatic exposures than when carious exposures are treated. Further research is needed to give clearer indications as to the prognosis for pulp caps. Teeth treated in this way will always require monitoring for loss of vitality and continuing symptoms, let alone radiographic evidence of periradicular periodontitis. It is suggested that prompt endodontic therapy is indicated for teeth that have pulp caps and develop symptoms, especially if there is radiographic evidence of progressive obliteration of the root canal system.
Indirect pulp capping
Indirect pulp capping is defined as the application of therapeutic material (usually hard-setting calcium hydroxide cement) to dentine that is affected by caries but not />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


