chapter 3 Patient Medical History for Dental Implant Surgery
Treatment planning for implants can begin only when the clinician has determined that the patient is in good general health and is psychologically, functionally, anatomically, and medically a good candidate for implants. The ascendancy of implant therapy as the prosthetic standard of care for many dental conditions can be maintained only if clinicians develop comprehensive case selection criteria.1 Patient selection criteria should include a determination as to whether conventional dentures or fixed partial prostheses may be preferable to dental implants for patients with certain medical conditions (e.g., epilepsy, oral carcinoma, myocardial infarction, scleroderma, Parkinson’s disease, tardive dyskinesias).2 In addition to classifying patients as totally or partially edentulous, the clinician must evaluate patients’ current dental condition through intraoral examinations, charting, diagnostic casts, photographs, periapical and panoramic radiographs, and other diagnostic aids. These are needed to determine not only the quality and quantity of alveolar bone but also the existence of malocclusion, caries, periapical lesions, and periodontal disease.3–5 Information gathered during the clinical examination is of great importance, and this examination should be done meticulously and routinely with every patient. It should always start with assessment of the patient’s extraoral conditions and palpation of the face and neck, with attempts to detect any abnormalities in glands or lymph nodes. Intraoral examinations should include visualization of every single area of the oral cavity lined with mucosa—the tongue, the throat—and, finally, an evaluation of the condition of the teeth. All this important information should be written in the patient’s chart immediately after the examination.
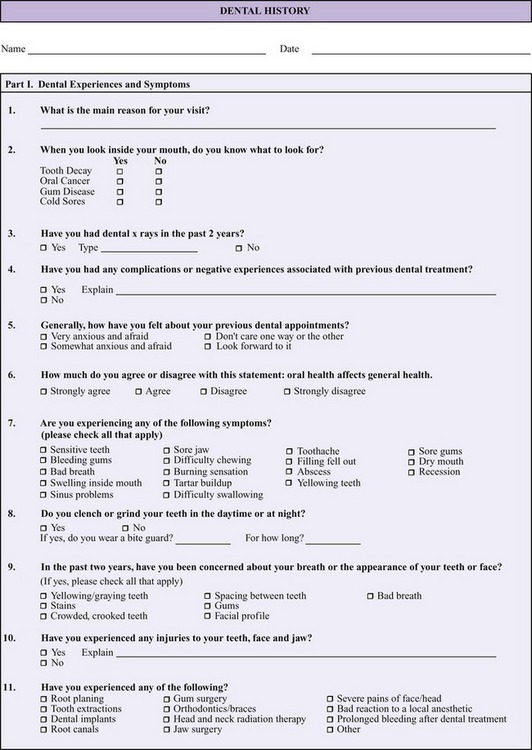
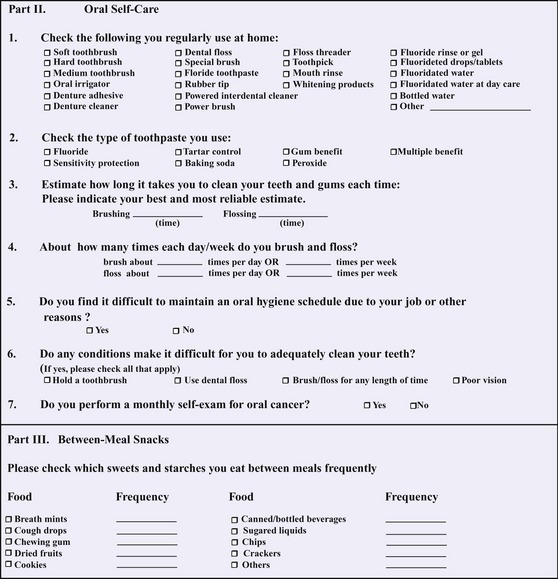
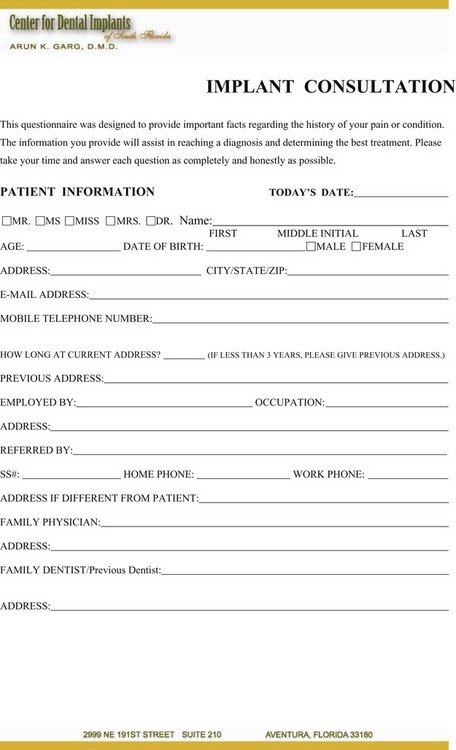
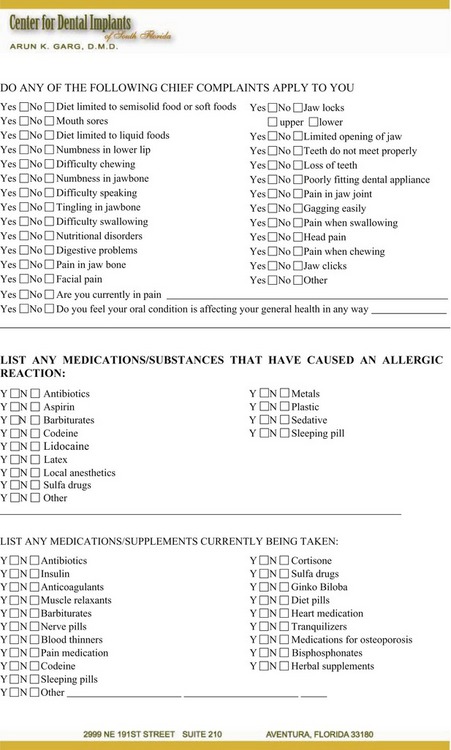
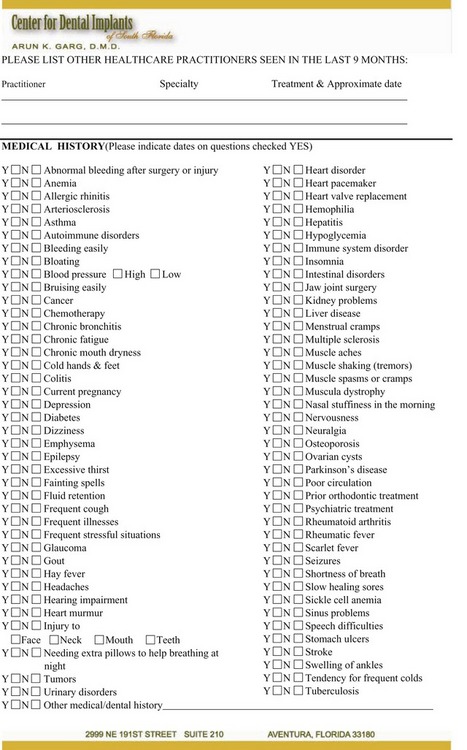
Additionally, the implantologist must obtain a complete patient medical history in order to determine proper treatment planning.2,6–9 Many dentists use the classification of physical status established by the American Society of Anesthesiology (ASA) to determine the planning and treatment of patients affected by systemic disease and sequelae.9 Very few medical conditions preclude implant placement, provided that the patient’s general health is adequate to withstand the required surgical and reconstructive procedures. However, specific medical conditions can minimize implant success, so the clinician must be diligent in obtaining factual information about patient history through an inclusive dental (Figure 3-1) and medical history form (Figure 3-2), patient interview, and consultation with the patient’s physicians and therapists. A review of how and why this patient information is gathered can help the dental practitioner more clearly understand the importance of the patient’s medical history to the success of dental implant procedures.
Dental and Medical History Form
The purpose of the dental and medical history form is to obtain information from the patient that will enable the clinician to provide dental care compatible with the patient’s general health. The patient must be convinced and confident that providing accurate information is essential, because incorrect information could endanger not only the successful outcomes of dental procedures but also the patient’s health. Of course, practitioner confidence, based on sound diagnostic practice and guidelines, can directly mirror patient confidence. For example, a 2005 study in Australia investigated the confidence in diagnosis and management of periodontal disease by dental practitioners, to determine if national guidelines on periodontal record keeping were being followed and to improve the periodontal knowledge of dentists.10 Although the study concluded that most dentists surveyed were confident when diagnosing periodontal disease, as well as treating the more common types of the disease, some dentists were not following minimum standards for periodontal record keeping. Therefore, thoroughness in dental record keeping can be an important factor in instilling patient and practitioner confidence. Additionally, along with clinician knowledge and experience, communication skills can play a key role in building patient trust in clinical procedures and practice.11
The patient’s physical status will determine whether routine dental therapies can be undertaken with or without modifications, limitations, or other special considerations regarding, for example, the duration of therapy,12 asepsis and sterilization preventative measures,13 and use of sedation.14–16 Patient medical history is just one of many factors often included during patient treatment to determine the increased risk for complications, along with other categories such as demographics, implant specifics, anatomical considerations, prosthetics, and reconstruction.12
It is also important for the practitioner to realize that patients of advanced age may present the dental team with several concerns not necessarily related to general health.9 The clinician must be aware of the physical, metabolic, and endocrine changes associated with aging and how these changes may affect implant treatment.17–19 Persons over 65 (and the fastest growing segment of the population, those between 85 and 100) often are affected by medical conditions that prevent them from exercising proper oral hygiene. Such diseases include Parkinson’s disease, cerebrovascular accident, Alzheimer’s disease, and major depressive disorder.9
Medical History
General medical conditions that minimize implant success include metabolic disorders (diabetes 1 and 2), osteoporosis, osseous metabolic disturbances (e.g., osteomalacia, osteitis deformans, Paget’s disease, osteogenesis imperfecta, osteopetrosis), hematologic disorders (e.g., anemia), disorders involving leukocytes (e.g., leukemia), disorders involving the blood clotting system (e.g., hemophilia), cardiac and circulatory diseases, collagen disorders (e.g., scleroderma), current medications (e.g., corticosteroids, immunosuppressives, antibiotics), and age-related elements (e.g., still-growing patients, advanced age)4 (Figure 3-3). Specific medical conditions that minimize implant success include uncontrolled diabetes, alcohol addiction, drug addiction, blood dyscrasias, and regular intake of corticosteroid or immunosuppressive drugs. Consequently, the following question areas should be included on the form: changes in health within the last year, last physical examination, current physician care and medication (including regularly taken herbal medications or drugs—legal or illegal—ingested within the last 48 to 72 hours), treatment for cardiovascular ailments (rheumatic fever, heart murmur, pacemaker, angina) and hypertension, stomach or intestinal disease, blood-related ailments (abnormal blood pressure, anemia), pulmonary ailments (asthma, hay fever), cancer (radiation, chemotherapy), diabetes, hepatitis, kidney disease, sexually transmitted disease (STD) (venereal disease, AIDS), stroke, convulsions, arthritis, allergies to medications (local anesthetics, antibiotics, aspirin, iodine), major operations, head and neck injury, smoking and chewing tobacco, alcohol, or drug addiction, mental status (psychiatric care, counseling), and, for women, current pregnancy, nursing, menstrual conditions, birth control pills/chemicals, and menopause. Intravenous administration of bisphosphonates (to treat osteoporosis, Paget’s disease, certain symptoms of multiple myeloma, and so on) has resulted in particularly alarming side effects, prompting the U.S. Food and Drug administration to warn health professionals in 2005 that patients taking bisphosphonates should not undergo invasive dental procedures: since 2003, 217 patients taking bisphosphonates have developed osteonecrosis of the jaw (gum infection, drainage, and poor healing; numbness, heaviness, pain, or swelling in the jaw; and exposed bone). Oral lesions associated with bisphosphonate use resemble osteonecrosis from radiation. Reports in the scientific literature have indicated a risk for development of osteonecrosis in patients taking intravenous and oral drugs for osteoporosis. The question remains as to the risk associated with oral forms of drugs for osteoporosis, including alendronate (Fosamax; Merck Co, West Point, VA), risedronate (Actonel), and ibandronate (Boniva; Roche Laboratories Inc, Nutley, NJ).
In addition to the above questions, the patient should be asked if anything not covered should be brought to the dentist’s attention. Changes in health status should be reported to the dental office. A 2005 retrospective cohort study attempted to determine guidelines for treatment planning based on rates of dental implant failure.20 To determine risk factors, the study examined data regarding patient gender and age, implant location, bone quality and volume, and medical history. Although the study concluded that the overall failure of dental implants is low and that no contraindications to implant placement can be considered absolute, certain conditions nonetheless were associated with significantly increased risk for failure; the conditions that dentists should consider during treatment planning and should include in the process of patient informed consent include being over 60 years of age, smoking, having a history of diabetes or radiation to the head and neck, and being menopausal and receiving hormone replacement therapy.20
Another later 2005 study provides conclusions based on a literature review centered on the success or failure of dental implants.21 The purpose of the study was to aid the dentist in recommending patients for implant placement. Implant success predictors included bone quantity and quality, age of the patient, experience of the dentist, implant location, implant length, axial loading of the implant, and maintenance of oral hygiene. The main predictors for implant failure included poor bone quality, chronic periodontitis, systemic disease, smoking, caries or infection that was unresolved, advanced age, location of the implant, short implants, acentric loading, inadequate implant number, parafunctional habits, and the absence or loss of integration related to hard and soft tissue conditions.
Diabetes Mellitus
Diabetes mellitus (Type 1, insulin dependent; Type 2, non-insulin dependent; and gestational) is a systemic disorder whose sequelae include alterations in wound healing; therefore, the effects of diabetes mellitus on osseointegration of implants have received considerable attention in the literature (Figure 3-4). As life expectancy continues to rise in populations worldwide, particularly in the developed world, dentists are more and more likely to treat patients who have developed diabetes mellitus. Studies have been inconclusive, showing rival failure rates between controlled diabetics and non-diabetic controls.22 One prospective study’s assessment of dental implants in type 2 diabetic patients showed no statistically significant difference in rates of failure of three different implants systems;23 another study conducted the same year (2000), however, revealed that Type 2 diabetic patients appear to have more implant failures than non-diabetic ones.24 A 2002 study concluded that diabetes mellitus should no longer be considered a contraindication for the placement of implants as long as the patient maintains control of blood sugar levels and is willing to follow a proper oral hygiene regimen25 (Table 3-1).
| HBA1C(%) | AVERAGE BLOOD SUGAR (mg/dl) |
|---|---|
| 6 | 120 |
| 7 | 150 |
| 8 | 180 |
| 9 | 210 |
| 10 | 240 |
| 11 | 270 |
| 12 | 300 |
A histomorphometric evaluation of new bone formation in diabetic rats into which were placed temporary implants revealed that new bone formation in cortical and periosteal regions did not differ significantly between the control group and the diabetic group; however, significant differences did result in medullar canal and in the bone-to-implant contact in the medullar portion.26 Another 2005 study using diabetic rats confirmed the inhibiting effects of diabetes on osseointegration, and further showed that the adverse effects could be marginalized to a significant extent by the use of aminoguanidine systemically, and by the use of doxycycline to a much lesser extent.27 A 2005 study to evaluate histologically the bone-to-implant contact in diabetes-induced rats after osseointegration had begun (uncontrolled diabetes vs. insulin-controlled) showed that bone-to-implant contact was maintained in the insulin-controlled cohort over four months; there was a decrease in contact, however, in the rats whose diabetes remained uncontrolled.28
Dental patients with diabetes mellitus should be treated according to guidelines that include a morning appointment, non-interruption of lifestyle, a good breakfast, patient-administered insulin, stress (anxiety, pain) reduction in the dental office, breaks during treatment, patient observation for hypoglycemic event, antibiotics for active infections, postoperative diet restrictions, insulin adjustment, and the absence of aspirin for postoperative pain.9
There is a correlation between A1c levels and average blood sugar levels as follows:
The American Diabetes Association currently recommends an A1c goal of less than 7.0%.
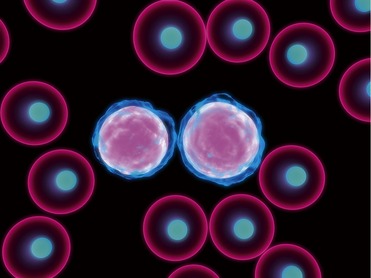
Blood Dyscrasias
An assortment of blood dyscrasias can affect healing in the dental patient (Figure 3-5). Definitions of blood dyscrasias include neutropenia, severe neutropenia, thrombocytopenia, hemolytic anemia, aplastic anemia, pancytopenia, and bicytopenia.29 The risk for severe blood dyscrasia (fivefold increases) has been associated with antibiotic use, including cephalosporins (highest risk), macrolides, penicillins, and quinolones.29 Various blood dyscrasias have been associated with other systemic disorders (diabetes mellitus, hormonal changes, HIV infection) affecting the course and severity of periodontal disease due to subsequent alteration of inflammatory responses in the oral cavity.30 Of particular concern for the dentist is the association of blood dyscrasias with mouth ulcerations.31 Despite the potential complications from bleeding related to surgical and restorative procedures associated with dental implants, patients with classic hemophilia can experience unimpaired function through the use of serial extractions and chairside temporization, allowing the dental surgeon to place implants with precision.32
Regular Intake of Corticosteroid or Immunosuppressive Drugs
Corticotherapy can be used to treat a variety of autoimmune connective tissue diseases, cancer, blood dyscrasias, and patients who have undergone transplantation. Acute adrenal cortical failure could result from the stress of dental treatment for some patients; prevention and alternative corticoid therapies are possible remedies for the dental patient.33 The history of liver transplantation since the mid-1980s has seen the increased use of immunosuppressive drugs to boost the success rate of such operations; however, studies have documented that the use of immunosuppressors such as cyclosporine and tacrolimus can adversely affect the buccodental health of liver transplant patients, including gingival overgrowth, gingival recession, and dental mobility.34,35 Immunosuppressive therapy can also affect bone metabolism.
A 2001 rabbit study investigated the results on bone surrounding titanium implants after the administration and withdrawal of cyclosporin A (CsA)/nifedipine, to determine changes and their reversibility, suggesting a significant decrease in treated animals within the bone area within the limits of the threads of the implant.36 A 2003 rabbit study attempted to evaluate the influence of the administration of CsA on the bone tissue around titanium implants; the study’s intergroup analysis showed that the removal torque and the percentage of bone contact with the implant surface for the CsA group were significantly lower than for the cytotoxic T lymphocyte (CTL) group after 12 weeks, suggesting that long-term administration of CsA may negatively influence bone healing around implants.37 However, the aim of another 2003 study was to evaluate the influence of the administration and withdrawal of CsA/nifedipine on bone density in a lateral area adjacent to implants placed in rabbits; it was determined that short-term immunosuppressive therapy may not negatively influence the density of the preexisting bone around titanium implants.38
Cardiovascular Ailments and Hypertension
Because cardiac disease remains the leading cause of death in the United States, a patient’s indication of a history of cardiac disease should lead the dentist to conduct a thorough inquiry into the patient’s present cardiac status; further questioning and the dentist’s knowledge of types of cardiac disease will help determine the peri-operative treatment planning for implant placement39 (Figure 3-6). Four general categories of cardiac disease include ischemic, valvular, arrhythmic, and myopathic; cardiac status can be measured in a number of ways, including pulse rate and rhythm, blood pressure, respiratory rate, cyanosis, clubbing of fingernails, and pedal edema.39 Contraindications for implant surgery may include recent myocardial infarction and congestive heart failure, unstable coronary syndrome, unstable angina pectoris, significant arrhythmia, and severe valvular disease.9 A 1998 study focusing on the detection of medically compromised dental patients in The Netherlands classified patients according to the ASA risk score system, modified for dental treatment; an inventory of the number and nature of medical problems and the modified ASA risk score />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses