3 Microbiology and Pathology
1.0 IMMUNOLOGY AND IMMUNOPATHOLOGY
1.1 Host Defense Mechanisms
A. Anatomical barriers
1. Skin
C. Innate immune response
1. Acute inflammation
a. Early immune response to injury or infection includes:
(1) Edema—caused by the increased vascular permeability of endothelial cells. Initially, the arterioles briefly vasoconstrict. This is followed by vasodilation and increased permeability of the endothelium. Fluid then moves from the circulation into the interstitial tissue, resulting in hyperemia and local edema. These actions are described by the four classic signs of inflammation: tumor (swelling), rubor (redness), calor (heat), and dolor (pain).
2. Chronic inflammation
3. Granulomatous inflammation
b. Granulomas are areas that the immune system “walls off” if phagocytes fail to destroy foreign particles or microbes present in it.
c. Inflammatory mediators include a dense concentration of macrophages, fibroblasts, lymphocytes, and (less frequently) plasma cells. The continuous activation of macrophages induces them to attach to one another, assuming an epithelium-like (epithelioid) appearance; they may also fuse with each other to form multinucleated giant cells.
D. Acquired immune response
2. There are two types of specific immune responses: cell–mediated immunity, which is mediated by T cells, and humoral immunity, which is mediated by antibodies that are produced by B cells.
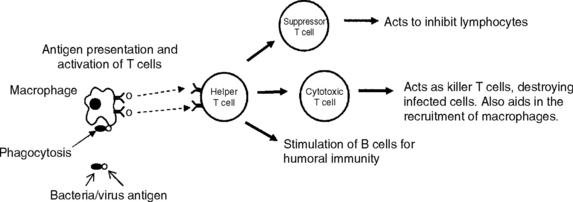
3. Cell-mediated immunity
b. Since T cells cannot directly recognize antigens, antigens must be processed and presented to them by antigen-presenting cells (APCs), such as macrophages, dendritic cells, B cells, and endothelial cells. APCs digest the antigens into small peptides and present them with a class II MHC molecule to the CD4 receptor on the helper T cell. This activates the helper T cells to release cytokines that cause inflammation and the activation of other T cells, B cells, and macrophages (Figure 3-1).
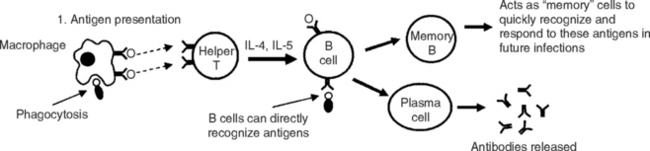
4. Humoral immunity (antibody-mediated immunity)
a. This branch of the specific immune response serves two purposes:
b. Antigens are first recognized by macrophages or directly by B cells. Like cell-mediated immunity, the macrophage will process and present the antigens to helper T cells. This causes them to secrete cytokines, interleukin-4 (IL-4), and interleukin-5 (IL-5), which results in B-cell stimulation and growth, thus resulting in the production of specific antibodies against the antigen presented (Figure 3-2).
1.1.1 Wound healing
A. Primary wound healing
2. Timeline of cellular events:
a. First 24 hours—formation of a fibrin clot. Fibronectin, an adhesive molecule found in plasma and on cell surfaces, forms crosslinks to stabilize the clot. PMNs or neutrophils migrate to the injured site.
b. Day 1 to 2—basal cells begin to proliferate (i.e., undergo mitosis) to close the epidermal defect.
1.1.2 Immune effector cells
A. T cells
4. Can be categorized by their function, namely, regulatory or effector. The regulatory function is primarily mediated by helper T cells, which have CD4 surface receptors. The effector function is primarily mediated by cytotoxic and suppressor T cells, which contain CD8 surface receptors:
C. Mononuclear cells—monocytes (in blood) and macrophages (in tissues)
4. The body has an extensive network of macrophages known as the reticuloendothelial system. These macrophages are fixed and serve different functions, depending on their tissue location. Examples include:
6. Phagocytosis
b. Phagocytosis is a process that initiates with the formation of a membrane-bound vacuole (phagosome) around the foreign particle or microbe. The phagosome then fuses with a lysosome, which contains many degradative enzymes, resulting in the formation of a phagolysosome. This process results in the destruction of the microbe.
D. Mast cells
1. Contain surface antigen receptors, including IgE. IgE plays an important role in type I immediate hypersensitivity reactions.
1.1.3 Cytokines
A. Cytokines are inflammatory mediators that are released by a variety of cells, such as macrophages or lymphocytes, to regulate immune responses. Think of them as the words that immune cells use to communicate with each other.
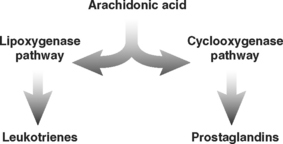
D. Prostaglandins (PGs) and leukotrienes (LTs)—mediators of the inflammatory response. PGs and LTs are metabolites of arachidonic acid. They are produced by the cyclo-oxygenase and the lipoxygenase pathway, respectively (Figure 3-3). General actions of these cytokines include vasoconstriction, bronchoconstriction, and increased inflammatory activity.
| CYTOKINE | SOURCE | ACTIONS |
|---|---|---|
| IL-1 | Macrophages | Stimulate cell activity or production of mediators in a variety of cells, including lymphocytes, macrophages, and endothelial cells. They also cause fever. |
| IL-2 | Helper T cells | Activate helper and cytotoxic T cells. |
| IL-3 | Activated T cells | Stimulate production of RBCs in bone marrow. |
| IL-4 | Helper T cells | Stimulate B cell growth and production of IgE and IgG. |
| IL-5 | Helper T cells | Stimulate B cell differentiation into plasma cells, activity of eosinophils, and production of IgA. |
TABLE 3-2 IMPORTANT INTERFERONS AND THEIR ACTIONS
| CYTOKINE | SOURCE | ACTIONS |
|---|---|---|
| INF-α | Leukocytes | Inhibit viral growth |
| INF-β | Fibroblasts | Inhibit viral growth |
| INF-γ | Helper T cell | Strong activator of macrophages, important in cell-mediated immunity |
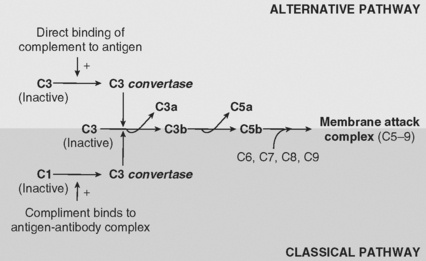
1.1.4 Complement System
A. Consists of a group of nearly 30 preformed serum and membrane proteins found in blood serum or on cell surfaces. They become activated through protease activity in a cascading order.
B. Main function is to generate reaction products that enhance antigen clearance and stimulate an inflammatory response. It achieves this by the following actions:
2. Opsonization—specific complement proteins (C3b), or opsonins, bind to the surfaces of microbes or foreign particles to encourage their phagocytosis.
C. The complement cascade: two pathways (Figure 3-4):
1. The alternative pathway—complement becomes activated by direct contact with the microbe or injured site. C3 binds directly to the surface antigen, activating the complement system.
1.1.5 Immunoglobulins (Antibodies)
A. Antibody effector functions include:
1. Neutralization—by binding directly to the antigen, the antibody neutralizes the antigen by preventing it from further interaction with other cells.
B. Antibodies can also cause agglutination of antigens (i.e., antigens clump together). The classic example of this is blood typing, where blood type is determined by agglutination of RBCs to specific agglutins.
C. Immunoglobulin classes
2. IgA
3. IgM
1.2 Hypersensitivity
A. Type I immediate hypersensitivity
2. A hyperresponse of the immune system caused primarily by the production and accumulation of IgE antibody.
3. The accumulation of IgE requires prior sensitization or exposure to a specific allergen. Reexposure of the allergen causes it to bind to IgE receptors on mast cells, resulting in large releases of inflammatory mediators.
4. Two subtypes:
a. Atopic allergies
(2) Family members display a strong hereditary predisposition to allergy sensitization, which may result from a genetic defect affecting the regulation of the IgE response.
B. Type II antibody-dependent cytotoxic hypersensitivity
C. Type III immune-complex mediated hypersensitivity
2. Antigen–antibody interactions result in the formation of immune complexes. These complexes become trapped along the vascular walls, activating complement and the immune response. Damage to the blood vessel walls occurs primarily from phagocytosis of the immune complex by the cells of the reticuloendothelial system.
3. Important examples:
a. Arthus reaction
D. Type IV delayed (cell-mediated) hypersensitivity
1. There are no antibody mediators. Helper T cells are the main mediators in delayed hypersensitivity.
2. Antigens are presented by antigen-presenting cells to helper T cells. The activated helper T cells release cytokines to activate the immune response, including stimulating macrophages to increase their release of lytic enzymes. Note: the leakage of these enzymes may result in tissue damage.
1.3 Immunopathology
A. Bruton’s agammaglobulinemia
C. DiGeorge’s syndrome
E. Angioedema
1. Acquired angioedema is caused by a deficiency of the complement inhibitor, C1-INH, which inhibits the conversion of C1 to C1 esterase. Note: angioedema can also be caused by allergic reactions and may be seen in patients taking certain medications, such as angiotensin-converting enzyme (ACE) inhibitors.
F. Chronic granulomatous disease
G. Autoimmune diseases
1. Systemic lupus erythematosus (SLE or lupus)
c. Characterized by the presence of antinuclear antibodies (ANAs). Common ANA findings include anti-DNA, anti-RNA, and anti-Sm antigen. ANAs can form immune complexes in the microvasculature of many organ systems, including:
d. Raynaud’s phenomenon may be seen in patients. This describes when a patient’s fingertips or toes become white and blue upon exposure to cold temperatures, due to a decrease in blood flow. Note: Raynaud’s phenomenon is also seen in patients with CREST syndrome (calcinosis, Raynaud’s syndrome, esophageal dysmotility, sclerodactyly, and telangiectasia) or acrosclerosis.
2.0 GENERAL MICROBIOLOGY
2.1 Biology of Micro-Organisms
2.1.1 Bacteria
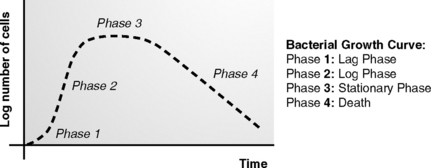
A. Growth of bacteria—can be divided into four phases (Figure 3-5):
2. Phase 2: log phase—period when bacteria grow exponentially, via rapid cell division (binary fission, when a parent cell divides into two separate cells). This exponential growth results in a very rapid increase of the number of bacteria present. Note: penicillins act on this phase.
B. Classification of bacteria
1. Classification by oxygen metabolism
C. Classification by gram-staining
2.2 Bacterial Cell Walls and Their External Surfaces
All bacteria are surrounded by a cell wall except Mycoplasma. They only have a cell membrane.
A. Cell wall—a multilayered structure located external to the cytoplasmic membrane
1. Cell wall characteristics of gram-positive bacteria:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses