Bone diseases of radiological importance
Introduction
Using the atlas approach adopted in Chapter 24, an example of each of the conditions is shown together with a summary of the main radiographic features seen in the skull and facial skeleton. It is worth remembering that bone is a constantly changing, dynamic tissue. Thus diseases of bone can present a spectrum of radiographic appearances depending on the behaviour and maturity or stage of the disease and/or lesion(s). The examples shown represent only a small part of that spectrum.
Developmental or genetic disorders
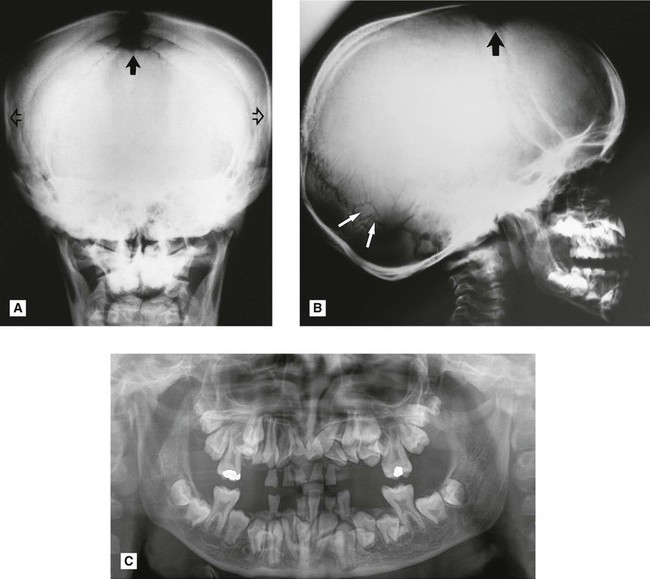
Cleidocranial dysplasia
This is a rare developmental disturbance affecting the skull and clavicles. The abnormalities of dentition can be gross but usually affect only the permanent teeth. Examples are delayed eruption and multiple supernumeraries (see Fig. 28.1).
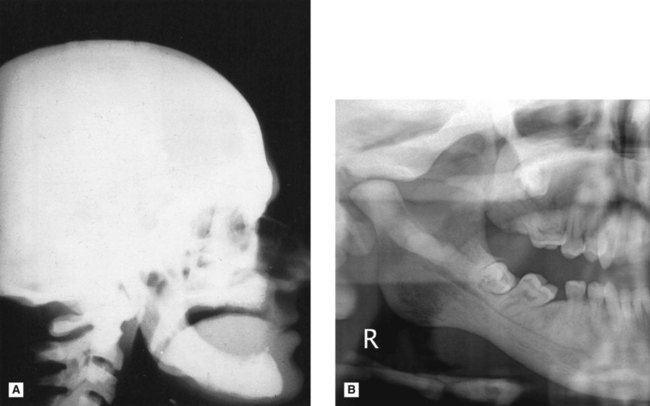
Osteopetrosis (Albers–Schönberg disease)
This hereditary disease is characterized by sclerosis of the skeleton (so called marble bones), fragile bones and secondary anaemia. Bone formation is normal but bone resorption is reduced, resulting in the presence of excessive calcified tissue and lack of marrow space (see Fig. 28.2). Cranial base changes may produce compression of the cranial nerves.
Main radiographic features
Infective or inflammatory conditions
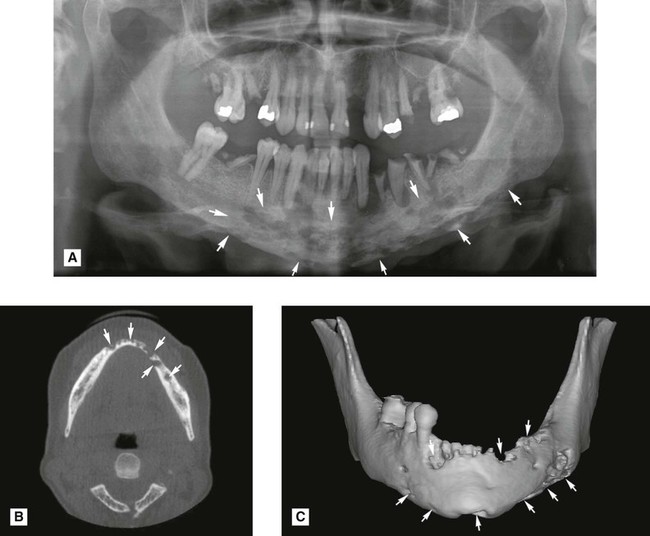
Osteomyelitis
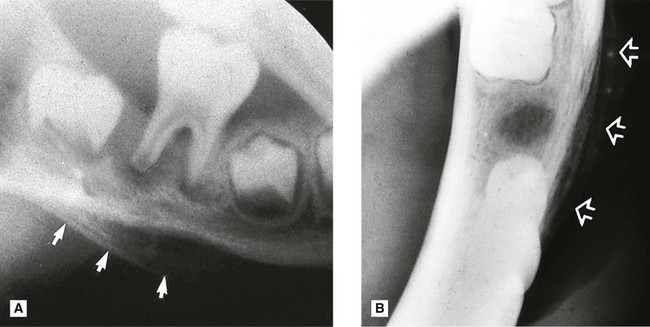
This spreading, progressive inflammation of bone and bone marrow, more frequently affects the mandible than the maxilla. It is caused usually by local factors such as periapical infection, pericoronitis, acute periodontal lesions, extractions or trauma. The inflammatory response may be acute or chronic depending on the virulence of the infecting organism and the resistance of the patient. It results ultimately in the destruction of the infected bone (see Figs 28.3 and 28.4). The reaction of the surrounding bone and periosteum is very variable and often age-related. There may be surrounding sclerosis of the bone forming poorly defined patchy opacity. Sequestra (small pieces of necrotic bone) can be exfoliated over a period of several weeks. The periosteum around the affected area can lay down new bone (the so-called periosteal reaction). In children this can be pronounced and is described as proliferative periostitis. This typically affects the mandible in young girls, following apical or pericoronal infection associated with the lower first molar producing a non-tender, bony hard swelling of the lower border. Radiographically the proliferative periostitis results in a laminated, so called onion-skin, appearance (see Fig. 28.5).
Main radiographic features of acute osteomyelitis
• Ragged, patchy or moth-eaten areas of radiolucency – the outline of the area of destruction is irregular and poorly defined
• Evidence of small radiopaque sequestra of dead bone occasionally within the radiolucency
• Evidence of new subperiosteal bone formation, usually beyond the area of necrosis, particularly along the lower border of the mandible.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses