chapter 26 Intravenous Moderate Sedation: Techniques of Administration
Techniques of intravenous (IV) moderate sedation are discussed in this chapter employing the drugs presented in Chapter 25. In this fifth edition, two techniques of IV sedation, the classic Jorgensen technique and IV promethazine, have been deemphasized, having been supplanted by techniques involving benzodiazepines that are discussed later.
MONITORING DURING INTRAVENOUS SEDATION
Whenever drugs are administered parenterally, it is of paramount importance that the patient be monitored closely. Guidelines for monitoring during moderate sedation have been developed.1–7 Every dentist must adhere to those regulations regarding monitoring that have been established by the dental governing body in the state or province in which they are licensed to practice.
The following represents this author’s recommendation for monitoring during IV moderate sedation:
The following monitoring devices are available (see discussion in Chapter 5):
The pretracheal stethoscope is recommended for use during IV moderate sedation procedures. It is both effective and inexpensive. The pulse oximeter has become a standard monitoring device during IV moderate sedation. Functioning as a continuous monitor of arterial oxygen (O2) saturation and heart rate, the pulse oximeter represents the standard of care for monitoring during parenteral sedation. As an aside, recent graduates from U.S. dental schools who use IV moderate sedation would not even consider starting an IV sedation case in the absence of an oximeter.8 End-tidal CO2 monitors (capnographs) are rapidly gaining entry into the monitoring armamentarium of dentists using general anesthesia or IV deep sedation and somewhat more gradually for IV moderate sedation. The ECG is less essential during parenteral sedation procedures than are techniques for monitoring the respiratory system. The ECG, though desirable, should be considered an optional monitor for IV moderate sedation. Regulatory bodies in a number of states have mandated the use of an ECG during IV moderate sedation.
BASIC INTRAVENOUS MODERATE SEDATION TECHNIQUES
These sedation techniques form the backbone of IV moderate sedation. Knowledge of these techniques will enable the trained dentist to meet the needs of a dental or surgical procedure of any duration, achieving satisfactory sedation for virtually all patients requiring IV moderate sedation (Box 26-1).
The Jorgensen technique is, arguably, the original IV moderate sedation technique.9 Despite efforts at modifying (e.g., improving) it, the original Jorgensen technique is still used, providing excellent sedation with few reports of any significant complications. The primary indication for the Jorgensen technique is a dental procedure requiring 2 or more hours to complete. Since the introduction of the benzodiazepines, especially midazolam, and because of the inability to reverse the clinical actions of pentobarbital, use of the Jorgensen technique has decreased. For an in-depth discussion of the Jorgensen technique, the reader is referred to earlier editions of this textbook.10 The Jorgensen technique is discussed later in this chapter.
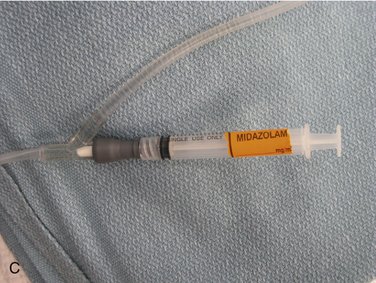
IV moderate sedation using a benzodiazepine has replaced the Jorgensen technique as the most popular technique in dentistry.11 IV benzodiazepine sedation meets the needs of contemporary dental practice (i.e., sedation for approximately 1 hour). Midazolam, introduced in the United States in 1985, has supplanted diazepam to become the most used IV technique in the area of 1-hour IV moderate sedation.11
Midazolam or Diazepam?
Patients who are receiving benzodiazepines orally for prolonged periods may exhibit a tolerance to the IV administration of diazepam or midazolam. Robb and Hargrave12 reported three cases of patients who required doses of 47 and 50 mg midazolam, 26 mg midazolam, and 30 and 34 mg midazolam for IV sedation. Discontinuance of the oral benzodiazepine produced a return to more normal response.
Intravenous Benzodiazepine (Midazolam or Diazepam)
Preliminary Appointment
Informed Consent
If the IV route is selected, informed consent must be provided to the patient, describing the IV procedure, its alternatives (e.g., IM, general anesthesia), and the most likely complications associated with its use. The patient signs the consent form, which is then added to the patient’s dental record. A specific informed consent for IV sedation should be signed before each IV procedure when multiple IV sedation visits are planned.13
Recording of Baseline Vital Signs
Baseline vital signs are obtained at this visit if they have not been previously recorded.
Preoperative Instructions
The following is an example of preoperative instructions for IV moderate sedation:
When oral sedation is prescribed preoperatively, an escort must drive the patient to the office.
COMMENT: Research has demonstrated that morbidity and mortality following anesthesia in patients with upper respiratory infections (URIs) are significantly greater in the time following the patient’s apparent “recovery” from the URI.14 Most of this morbidity is related to respiratory disease.
Day of Treatment
During this time, the assistant will prepare the IV infusion and drugs for use (see Chapter 24). Once all is ready, the patient is asked to visit restroom to void, if necessary, following which the patient is taken to the treatment room and seated in a semiupright (comfortable) position. The availability of the patient’s escort should be determined at this time.
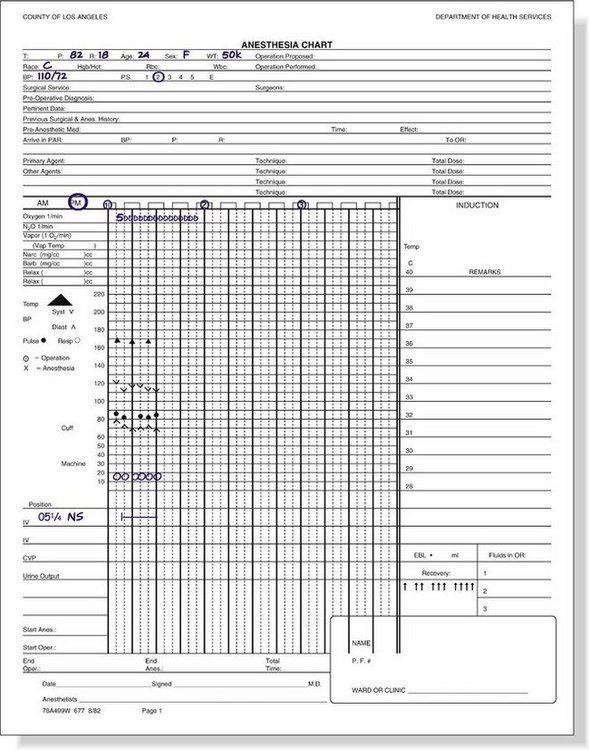
Once the patient is seated in the dental chair, monitors are placed, and preoperative vital signs are monitored and recorded on the anesthesia record sheet (Figure 26-1). Ideally the blood pressure cuff is placed on the arm opposite the working side of the dentist, remaining in place throughout the procedure. If used, the pretracheal stethoscope and ECG electrodes are applied along with the pulse oximeter or end-tidal CO2 monitor. A nasal cannula or nasal hood is positioned, and a 3- to 6-L/min flow of O2 is administered throughout the IV procedure.
Because of an increased risk of phlebitis when diazepam is administered, it is suggested that, when possible, smaller veins, such as those on the dorsum of the hand or wrist, be avoided when venipuncture is performed.15,16 This is not necessary with midazolam. Because midazolam is water soluble, phlebitis is uncommon, and venipuncture may be established at any available site, including the dorsum of the hand and wrist. Venipuncture is completed, and the IV infusion is established and secured (see Chapter 24).
Midazolam
Drug Administration
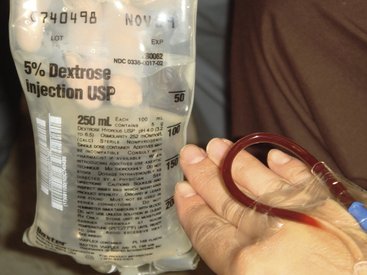
Immediately before beginning drug administration, the assistant or dentist should make one final check to confirm that the IV infusion is still patent. By squeezing the flash bulb of the tubing or holding the bag of IV solution below the level of the patient’s heart, a return of blood into the tubing should be noted, a sign of a still patent IV line (Figure 26-2).
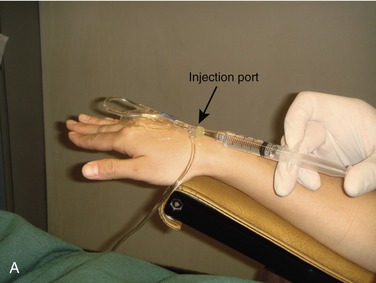
A test dose of 0.2 ml (each small delineation on the 3-ml or 5-ml syringe is 0.2 ml) is administered to determine whether any unusual response (e.g., hypersensitivity, allergy) is to develop (Figure 26-3).
Intraoperative Period
Local anesthetic is administered to the patient exactly as it would be if the patient was not sedated. This includes the use of topical anesthetic and all of the other steps involved in the atraumatic administration of local anesthesia.17 The patient may react to any pain associated with the local anesthetic injection, but this usually is nothing more than a slight moan, grimace, or minor movement. Adequate time should be allowed for the local anesthetic to take effect (3 to 5 minutes) before starting the planned procedure.
During the first 1 to 5 minutes following IV midazolam titration, the level of sedation (CNS depression) is greatest. Although overresponse to the drug can occur, the patient who has overresponded to midazolam will be somewhat sluggish in response to verbal commands, such as “open your mouth.” For this reason, the use of a mouth prop should be considered, at least at the outset of the IV moderate sedation procedure. Within 5 to 10 minutes, the depth of sedation has usually lessened so that the patient’s mouth can be voluntarily kept open. A rubber bite block with a piece of string (dental floss) tied around it or a ratchet type of (Molt) mouth prop may be used at this time (Figure 26-5).
Lack of response to verbal command or, more significantly, a lack of response to a painful stimulus (i.e., local anesthetic injection) may indicate that the patient is overly sedated. Lack of response to sensory stimulation is always reason for the dentist to stop treatment and reevaluate the patient’s level of consciousness and airway and ventilatory status (e.g., to “rescue” the patient from unintended entry into the next level of sedation [deep]).18
Treatment begins at this time. Because of the 45- to 60-minute duration of sedation provided by IV midazolam, the dental treatment should be planned to fit into this time period. Midazolam produces a period of anterograde amnesia in most patients, lasting for most of the duration of the dental procedure (if not longer).18 Potentially painful or traumatic procedures completed during this time will likely not be remembered by the patient later, though they will still respond to the stimulus in a somewhat normal manner when they occur.
It is uncommon for a patient to require a second dose of midazolam if the duration of the planned procedure was appropriate (about 1 hour). As discussed in Chapter 25, midazolam sedation may be divided into several phases: stage 1: (minutes 1 to 10) good sedation plus amnesia; stage 2: (minutes 11 to 30) “OK” sedation plus amnesia; stage 3: (minutes 31 to 45) sedation wanes (patient more alert), amnesia still present; and stage 4: (minutes 46 to 60): clinical recovery of patient, amnesia may still be present. With entry into the third phase, the patient may opine that he or she feels “normal” once again, and the dentist might be tempted to administer additional midazolam. However, by this time, treatment should be nearing completion, the procedure performed is usually atraumatic, the patient has effective pain management (local anesthesia), and although the patient feels normal, he or she is still anxiety free, if not visibly sedated. Readministration of midazolam is rarely necessary in this typical 1-hour IV moderate sedation procedure.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses