Periodontics
Learning Objectives
1 Pronounce, define, and spell the Key Terms.
2 Explain the significance of plaque and calculus in relation to periodontal disease.
3 Name and describe the five case types of periodontal disease.
4 Explain the procedures necessary for a comprehensive periodontal examination.
5 Describe how radiographs are used in periodontics.
6 Identify the instruments used in periodontics and explain the indications for their use.
7 Discuss the advantages and disadvantages of the ultrasonic scaler.
8 Name and describe the types of periodontal surgeries.
Key Terms
Gingival Graft
Gingivectomy
Gingivitis
Gingivoplasty
Mobility
Ostectomy
Osteoplasty
Periodontal Flap Surgery
Periodontal Pocket
Periodontist
Periodontitis
Periodontium
Sulcus
Supragingival/Subgingival Calculus
Ultrasonic Scaler
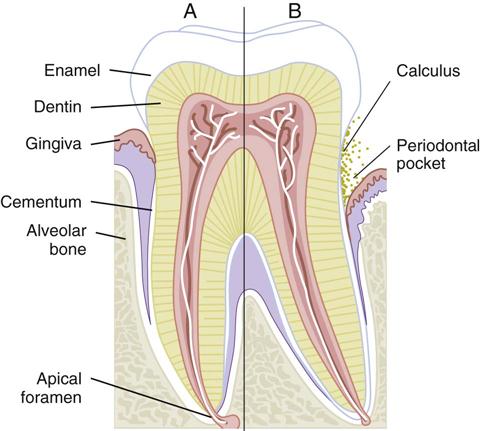
Periodontal diseases are the leading cause of tooth loss in adults. Fortunately, with early detection and treatment of periodontal disease, it is now possible for most people to keep their teeth for a lifetime. The periodontist (a dentist with advanced training in the specialty of periodontics) deals with the causes, prevention, and treatment of diseases of the tissue of the periodontium. The periodontium consists of the tissue that surrounds and supports the teeth (Figure 24-1 and Table 24-1).
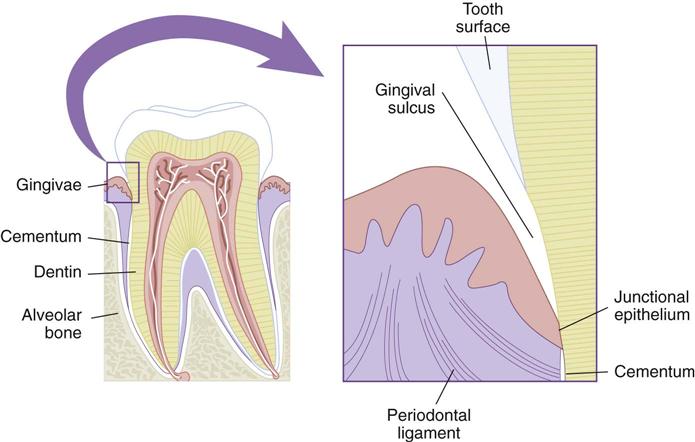
TABLE 24-1
Structures of the Periodontium
| Name | Description |
| Gingivae | Commonly referred to as “gums.” This mucosa covers the alveolar process of the jaws and surrounds the necks of the teeth. |
| Epithelial attachment | Tissue at the base of the sulcus where the gingiva attaches to the tooth |
| Sulcus | Space between the tooth and the free gingiva |
| Periodontal ligaments | Dense connective fibers that connect the cementum covering the root of the tooth with the alveolar bone of the socket wall |
| Cementum | Covers the root of the tooth. The primary function of cementum is to anchor the tooth to the bony socket with the attachments of the periodontal ligaments. |
| Alveolar bone | The bone that supports the tooth in its position within the jaw. The alveolar socket is the cavity in the bone that surrounds the tooth. |
Periodontal Diseases
Most periodontal diseases begin as an inflammation caused by an accumulation of bacterial plaque (see Chapter 17 for a discussion of plaque and calculus formation) adhering to the teeth, to calculus, and to fixed and removable restorations. Periodontal diseases and dental caries are infectious diseases caused by pathogenic (disease-causing) microorganisms found in microbial plaque. Calculus is mineralized microbial plaque. General oral health depends on the daily removal of bacterial plaque deposits.
Periodontal diseases may also be caused by other conditions in the mouth and by systemic conditions, such as hormonal disturbances (Table 24-2 and Box 24-1).
TABLE 24-2
Common Risk Factors for Periodontal Disease
| Risk Factor | Rationale |
| Smoking | Smokers have greater loss of attachment, bone loss, periodontal pocket depths, calculus formation, and tooth loss. Periodontal treatments are less effective in smokers than in nonsmokers. |
| Diabetes mellitus | Diabetes is a strong risk factor for periodontal disease. Individuals with diabetes are 3 times more likely to have attachment and bone loss. Persons who have their diabetes under control have less attachment and bone loss than those with poor control. |
| Poor oral hygiene | Lack of good oral hygiene increases the risk of periodontal disease in all age groups. Excellent oral hygiene greatly reduces the risk of severe periodontal disease. |
| Osteoporosis | An association has been noted between alveolar bone loss and osteoporosis. Women with osteoporosis have increased alveolar bone resorption, attachment loss, and tooth loss compared with women without osteoporosis. Estrogen deficiency has been linked to decreases in alveolar bone. |
| HIV/AIDS | Gingival inflammation is increased around the margins of all teeth. Often patients with HIV/AIDS will develop necrotizing ulcerative periodontitis (NUP). |
| Stress | Psychological stress is associated with depression of the immune system, and studies show a link between stress and periodontal attachment loss. Research is ongoing to determine the link between psychological stress and periodontal disease. |
| Medications | Some medications, such as tetracycline and nonsteroidal anti-inflammatory drugs (NSAIDs), have a beneficial effect on the periodontium, and others have a negative effect. Decreased salivary flow (xerostomia) can be caused by more than 400 medications, including diuretics, antihistamines, antipsychotics, antihypertension agents, and analgesics. Antiseizure drugs and hormones such as estrogen and progesterone can cause gingival enlargement. |
| Local factors | Overhanging restorations, subgingival placement of crown margins, orthodontic appliances, and removable partial dentures also may contribute to the progression of periodontal disease. |
Description of Periodontal Disease
Periodontal disease is described in terms of the severity of the disease and how much of the mouth is affected:
• If less than 30% of sites in the mouth are affected, the disease is considered localized.
• If more than 30% of sites in the mouth are affected, the disease is considered generalized.
The severity of the disease is determined by the amount of lost attachment, as follows:
The American Academy of Periodontology has identified seven basic case types of periodontal disease based on the severity of the disease and the amount of tissue destruction that has occurred at the time of examination.
Signs and Symptoms
The following signs and symptoms are seen most often in patients with periodontal disease:
• Red, swollen, or tender gingiva
• Bleeding gingiva while brushing or flossing
Gingivitis
Gingivitis is inflammation of the gingival tissue (Figure 24-2). It is perhaps the most common human disease and is among the easiest to treat and control. The gingivae appear red and swollen and have a tendency to bleed easily. Gingivitis is directly related to the presence of bacterial plaque on the tooth surface and the amount of time that the plaque is allowed to remain undisturbed. Plaque is discussed in Chapter 17.

Periodontitis
Periodontitis occurs as the infection from the gingivae progresses into the alveolar bone.
Periodontitis is divided into case types according to the severity of the disease and the amount of tissue destruction that has occurred at the time of the examination. Periodontitis usually occurs in older individuals and is often referred to as adult-onset periodontitis. However, periodontitis is also found in children.
Periodontal Examination
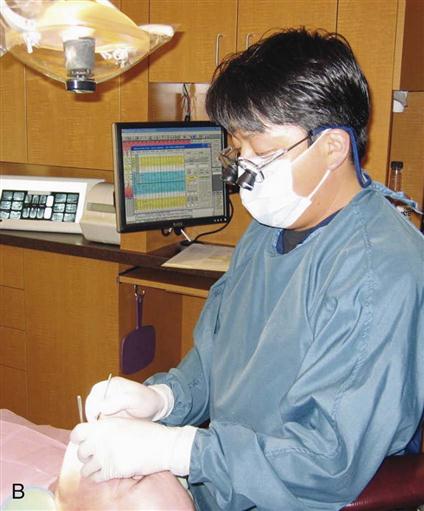
In addition to a thorough dental examination as described in Chapter 12, specialized procedures are necessary to diagnose and plan appropriate treatment for periodontal disease. A periodontal examination includes medical and dental histories, radiographic evaluations, examination of the teeth, examination of the gingivae and supporting structures, and periodontal charting, which consists of pocket readings and taking note of furcations, tooth mobility, exudate (pus), and gingival recession (Figure 24-3, A and B).
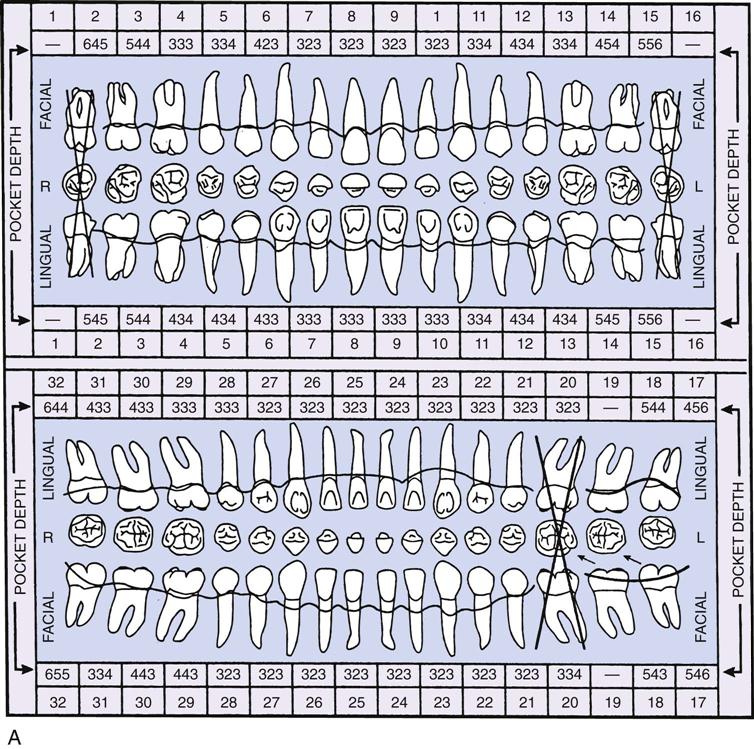
(Courtesy Patterson Office Supplies, Champaign, Illinois.)
B, A periodontal chart on a computer screen. This periodontist can easily refer to the chart as he treats the patient. (B, From Bird DL, Robinson DS: Modern dental assisting, ed 10, St Louis, 2012, Saunders.)
Radiographs
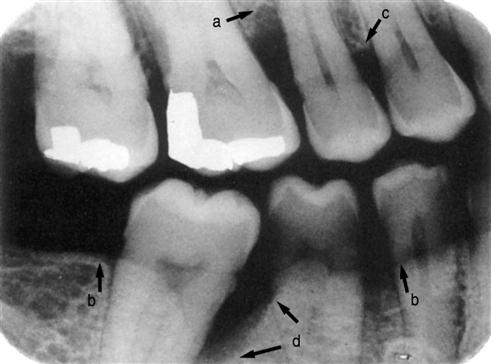
Radiographs are a valuable aid for evaluating periodontal disease. The accuracy of the radiographs is critical in the diagnosis of periodontal disease because a distortion can result in a diagnostic error (Figure 24-4).
Examination of the Teeth
The examination of the teeth focuses on indications of periodontal disease or factors that could contribute to periodontal disease (Table 24-3).
TABLE 24-3
Dental Conditions That Contribute to Periodontal Disease
| Condition | Description |
| Pathologic migration | A shift in the position of the teeth that can be caused by loss of periodontal support |
| Clenching or grinding (bruxism) | These oral habits place excessive biting forces on the teeth and may accelerate bone loss. |
| Defective restorations or bridge work | May retain plaque and increase the risk of periodontal disease |
| Mobility | Movement of the tooth within its socket. All teeth have a very small degree of natural mobility (see Figure 24-5). Mobility is recorded with the following scale: 0, normal; 1, slight mobility; 2, moderate mobility; 3, extreme mobility. |
| Occlusal interferences | Areas on a tooth that prevent the teeth from occluding properly. These do not directly cause periodontal disease but can contribute to mobility, tooth migration, and temporomandibular joint pain. |
Mobility
All teeth have a slight normal mobility (tooth movement in the socket) because of the function of the periodontal membrane. Excessive mobility can be an important sign of periodontal disease (Figure 24-5). The following scale is used to record the degree of mobility.
Examination of the Gingivae and Supporting Structures
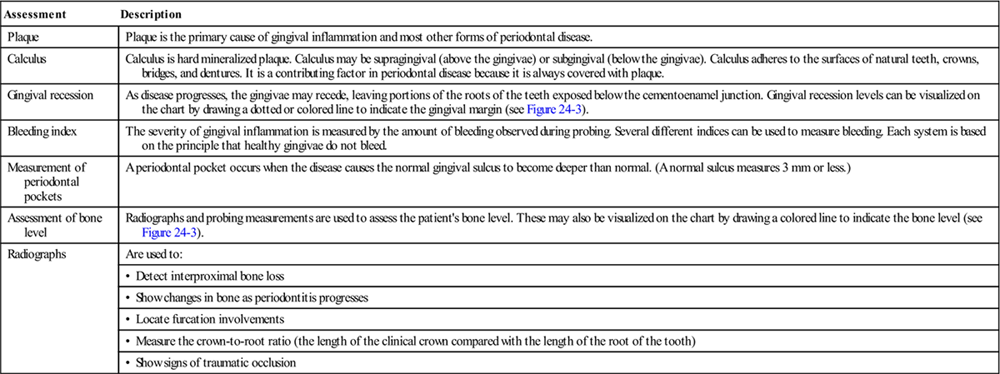
The periodontal examination includes an assessment of the amounts of plaque and calculus, and of changes in gingival health, as well as assessment of bleeding at the bone level and detection of periodontal pockets (Figure 24-6). A periodontal pocket occurs when disease causes the normal gingival sulcus to become deeper than normal (a normal sulcus measures 3 mm or less) (Table 24-4).
TABLE 24-4
Examination of the Gingivae and Supporting Tissue
< ?comst?>
| Assessment | Description |
| Plaque | Plaque is the primary cause of gingival inflammation and most other forms of periodontal disease. |
| Calculus | Calculus is hard mineralized plaque. Calculus may be supragingival (above the gingivae) or subgingival (below the gingivae). Calculus adheres to the surfaces of natural teeth, crowns, bridges, and dentures. It is a contributing factor in periodontal disease because it is always covered with plaque. |
| Gingival recession | As disease progresses, the gingivae may recede, leaving portions of the roots of the teeth exposed below the cementoenamel junction. Gingival recession levels can be visualized on the chart by drawing a dotted or colored line to indicate the gingival margin (see Figure 24-3). |
| Bleeding index | The severity of gingival inflammation is measured by the amount of bleeding observed during probing. Several different indices can be used to measure bleeding. Each system is based on the principle that healthy gingivae do not bleed. |
| Measurement of periodontal pockets | A periodontal pocket occurs when the disease causes the normal gingival sulcus to become deeper than normal. (A normal sulcus measures 3 mm or less.) |
| Assessment of bone level | Radiographs and probing measurements are used to assess the patient’s bone level. These may also be visualized on the chart by drawing a colored line to indicate the bone level (see Figure 24-3). |
| Radiographs | Are used to: |
| • Detect interproximal bone loss | |
| • Show changes in bone as periodontitis progresses | |
| • Locate furcation involvements | |
| • Measure the crown-to-root ratio (the length of the clinical crown compared with the length of the root of the tooth) | |
| • Show signs of traumatic occlusion |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
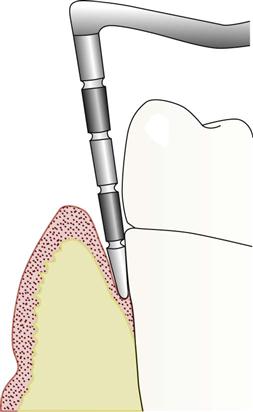
Probing Periodontal Pockets
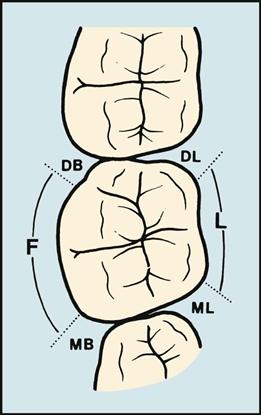
The depth of the periodontal pocket is measured by using a periodontal probe (Figure 24-7). The dentist or dental hygienist will take six measurements for each tooth (Figure 24-8). The dental assistant records the deepest measurement on each surface on the patient’s periodontal chart. The surfaces measured are:
Periodontal Probes
Periodontal probes, which are calibrated in millimeters, are used to locate and measure the depth of periodontal pockets (Figure 24-9). On some, the tip is color-coded to make the measurements easier to read.

The manual probe is tapered to fit into the gingival sulcus and has a blunt or rounded tip. This probe is available in many designs, and selection depends on personal preferences of the operator.
Automated computerized probes are extremely accurate electronic devices used to measure the depth of periodontal pockets. With the probe, a thin wirelike device is inserted into the sulcus, and data are recorded by a microcomputer. Voice-activated recording systems are becoming popular in periodontal assessment. The operator will speak the measurement, and the />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses