Coronal Polishing and Dental Sealants
Learning Objectives
1 Pronounce, define, and spell the Key Terms.
2 Explain the difference between a prophylaxis and coronal polishing.
3 Explain the indications for and contraindications to a coronal polish.
4 Name and describe the types of extrinsic stains.
5 Describe the two categories of intrinsic stains.
6 Describe four types of abrasives used for polishing the teeth.
7 Demonstrate the grasp and positioning for the prophy angle.
8 Demonstrate the fulcrum or finger rest used in each quadrant during a coronal polish procedure.
10 In states where it is legal, demonstrate on a typodont the coronal polishing technique.
11 Explain the purposes for the placement of dental sealants.
Key Terms
Air-Powder Polishing
Calculus
Clinical Crown
Dental Sealants
Endogenous
Etching
Exogenous
Fulcrum
Light-Cured
Oral Prophylaxis
Pits and Fissures
Rubber Cup Polishing
Coronal Polishing
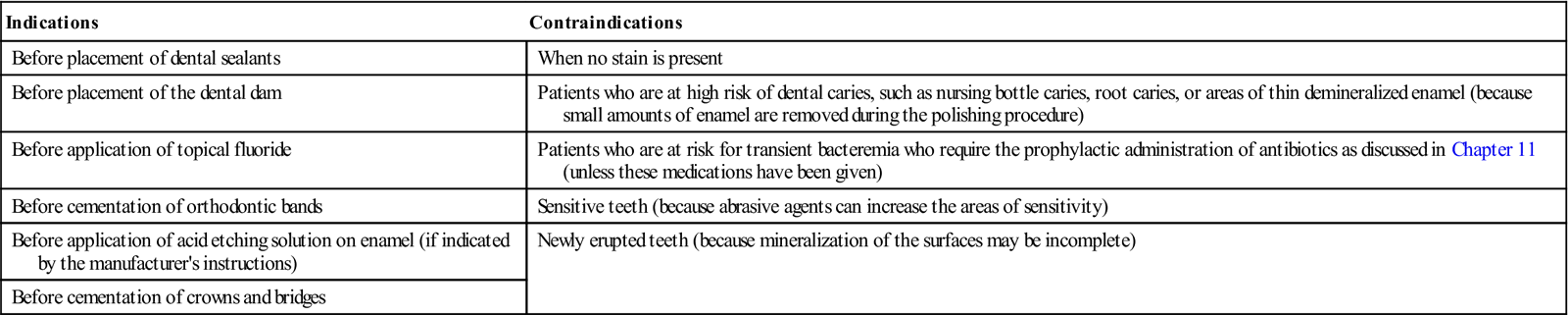
Coronal polishing (rubber cup polish) is used to remove plaque and stains from the coronal surfaces of the teeth. This is done with the use of a dental handpiece, a rubber cup, and an abrasive agent. There are specific indications for and contraindications to doing a coronal polish (Table 18-1).
TABLE 18-1
Indications and Contraindications to Coronal Polishing
< ?comst?>
| Indications | Contraindications |
| Before placement of dental sealants | When no stain is present |
| Before placement of the dental dam | Patients who are at high risk of dental caries, such as nursing bottle caries, root caries, or areas of thin demineralized enamel (because small amounts of enamel are removed during the polishing procedure) |
| Before application of topical fluoride | Patients who are at risk for transient bacteremia who require the prophylactic administration of antibiotics as discussed in Chapter 11 (unless these medications have been given) |
| Before cementation of orthodontic bands | Sensitive teeth (because abrasive agents can increase the areas of sensitivity) |
| Before application of acid etching solution on enamel (if indicated by the manufacturer’s instructions) | Newly erupted teeth (because mineralization of the surfaces may be incomplete) |
| Before cementation of crowns and bridges |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Coronal polishing is not a substitute for an oral prophylaxis. An oral prophylaxis, commonly known as a prophy or a cleaning, is the complete removal of calculus, debris, stain, and plaque from the teeth. (Calculus is a hard mineralized deposit attached to the teeth.) In almost every state, the dentist and the registered dental hygienist are the only members of the dental team licensed to perform an oral prophylaxis.
In some states, coronal polishing is delegated to registered or to expanded function dental assistants who have had special training in this procedure. Coronal polishing is strictly limited to the clinical crowns of the teeth. (The clinical crown is that portion of the tooth that is visible in the oral cavity.)
Selective Polishing
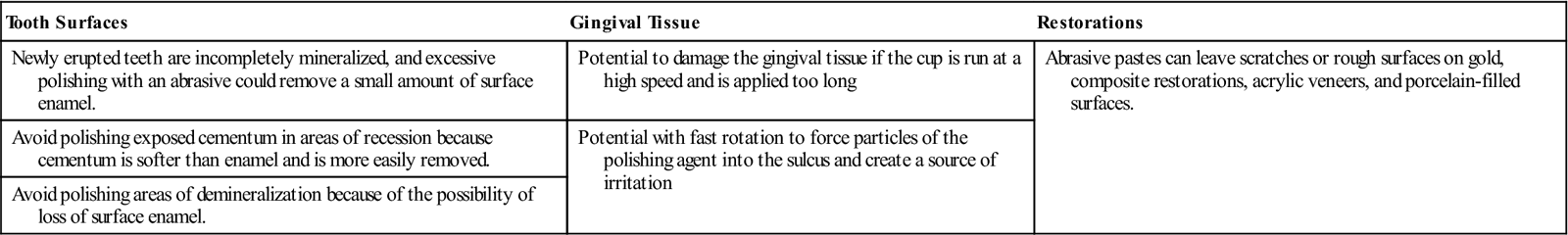
Selective polishing means that only those teeth or surfaces with stain are polished. This is done to avoid removing small amounts of enamel from the surface of the tooth with the abrasive agent during coronal polishing. The principle of selective polishing is to refrain from polishing unless necessary. The needs of the patient must always be reviewed before stain removal is performed (Table 18-2 and Box 18-1).
TABLE 18-2
Possible Damaging Effects of Coronal Polish
< ?comst?>
| Tooth Surfaces | Gingival Tissue | Restorations |
| Newly erupted teeth are incompletely mineralized, and excessive polishing with an abrasive could remove a small amount of surface enamel. | Potential to damage the gingival tissue if the cup is run at a high speed and is applied too long | Abrasive pastes can leave scratches or rough surfaces on gold, composite restorations, acrylic veneers, and porcelain-filled surfaces. |
| Avoid polishing exposed cementum in areas of recession because cementum is softer than enamel and is more easily removed. | Potential with fast rotation to force particles of the polishing agent into the sulcus and create a source of irritation | |
| Avoid polishing areas of demineralization because of the possibility of loss of surface enamel. |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Stains of the Teeth
Stains are primarily esthetic problems and vary in type and difficulty of removal. Food, chemicals, and bacteria cause stains.
Stains of the teeth occur in three basic ways:
• Stain adheres directly to the surface of the tooth.
Before coronal polishing is undertaken to remove stains, it is important to distinguish between extrinsic and intrinsic stains.
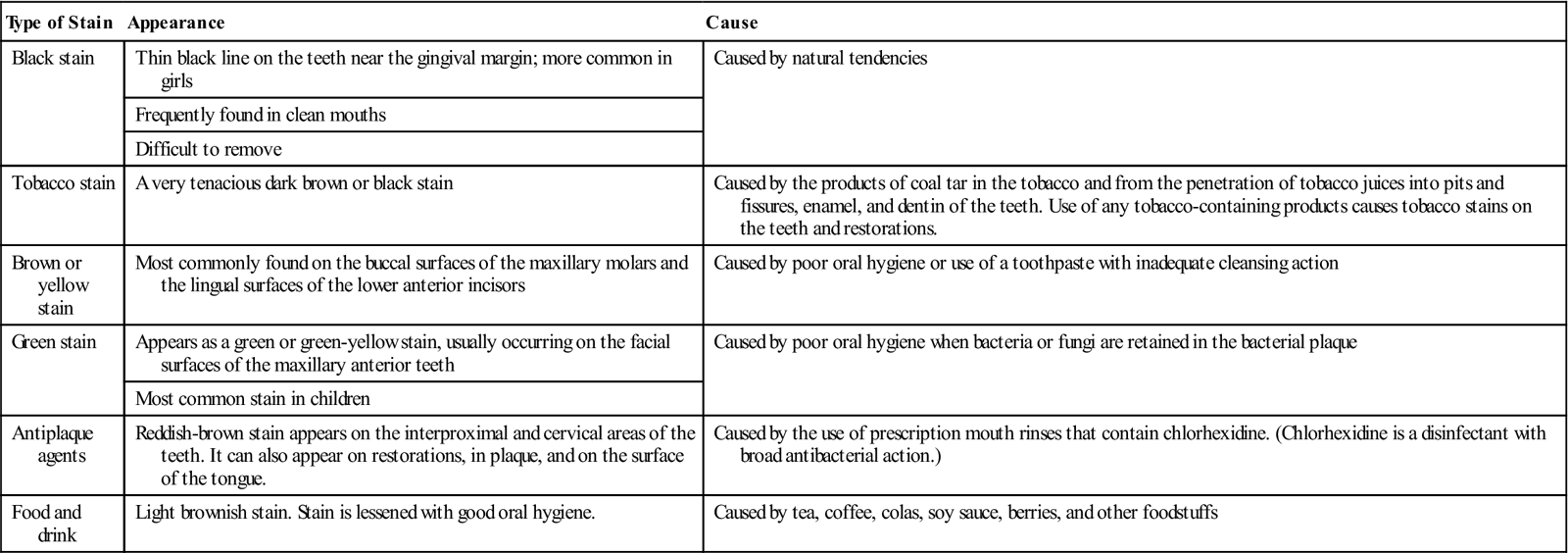
Extrinsic stains are those that occur on the external surfaces of the teeth and may be removed by scaling and/or polishing (Table 18-3).
TABLE 18-3
< ?comst?>
| Type of Stain | Appearance | Cause |
| Black stain | Thin black line on the teeth near the gingival margin; more common in girls | Caused by natural tendencies |
| Frequently found in clean mouths | ||
| Difficult to remove | ||
| Tobacco stain | A very tenacious dark brown or black stain | Caused by the products of coal tar in the tobacco and from the penetration of tobacco juices into pits and fissures, enamel, and dentin of the teeth. Use of any tobacco-containing products causes tobacco stains on the teeth and restorations. |
| Brown or yellow stain | Most commonly found on the buccal surfaces of the maxillary molars and the lingual surfaces of the lower anterior incisors | Caused by poor oral hygiene or use of a toothpaste with inadequate cleansing action |
| Green stain | Appears as a green or green-yellow stain, usually occurring on the facial surfaces of the maxillary anterior teeth | Caused by poor oral hygiene when bacteria or fungi are retained in the bacterial plaque |
| Most common stain in children | ||
| Antiplaque agents | Reddish-brown stain appears on the interproximal and cervical areas of the teeth. It can also appear on restorations, in plaque, and on the surface of the tongue. | Caused by the use of prescription mouth rinses that contain chlorhexidine. (Chlorhexidine is a disinfectant with broad antibacterial action.) |
| Food and drink | Light brownish stain. Stain is lessened with good oral hygiene. | Caused by tea, coffee, colas, soy sauce, berries, and other foodstuffs |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Intrinsic stains are those that occur within the enamel and cannot be removed by polishing (Table 18-4). Intrinsic stains may be endogenous (occurring during tooth development), or they may be exogenous (occurring after eruption).
TABLE 18-4
| Type of Stain | Appearance | Cause |
| Pulpless teeth | Not all pulpless teeth discolor. A wide range of colors exists: light yellow, gray, reddish brown, dark brown, or black; sometimes an orange or greenish color is seen. | Blood and pulpal tissue break down as a result of bleeding in the pulp chamber, or death of the pulp tissue. Pigments from the blood and tissue penetrate the dentin and show through the enamel. |
| Tetracycline antibiotics | Light green to dark yellow or a gray-brown. Discoloration depends on the dosage, the length of time the drug was used, and the type of tetracycline. | Can occur in the child when the mother is given tetracycline during the third trimester of pregnancy or when given in infancy and early childhood |
| Dental fluorosis | Also termed “mottled enamel,” it results from ingestion of excessive fluoride during the mineralization period of tooth development. | Varying degrees of discoloration ranging from a few white spots to extensive white areas or distinct brown stains (Fluorosis is discussed and illustrated in Chapter 17.) |
| Imperfect tooth development | Teeth are yellowish-brown or gray-brown. Teeth appear translucent or opalescent and vary in color. | May result from genetic abnormality or environmental influences during development |
| Silver amalgam | Appears as a gray or black discoloration around a restoration | Metallic ions from the amalgam penetrate into the dentin and enamel. |
| Other systemic causes | Appears as a yellowish or greenish discoloration in the teeth | Conditions of prolonged jaundice early in life and erythroblastosis fetalis (Rh incompatibility) |
Methods of Removing Plaque and Stain
Every stain removal technique has the potential for damage by removing a small amount of enamel from the surfaces of the teeth being polished. There is also the potential for injury to the gingivae; therefore these techniques must always be carried out with the utmost caution.
Two methods of stain removal are air-powder polishing and the rubber cup polishing technique.
Remember, you must check the regulations in your state to see if coronal polishing can be delegated to a qualified dental assistant, and if so, which technique is permitted.
Air-Powder Polishing
The air-powder polishing technique uses a specially designed handpiece with a nozzle that delivers a high-pressure stream of warm water and sodium bicarbonate. The powder and water, under high pressure, remove stain rapidly and efficiently; the flow rate is adjusted to control the rate of abrasion.
Rubber Cup Polishing
Rubber cup polishing is the most common technique for removing stains and plaque and for polishing teeth. An abrasive polishing agent is placed in a rubber polishing cup that is rotated slowly and carefully by a prophy angle attached to the slow-speed handpiece. This is the form of coronal polishing that is described in this chapter.
Equipment for Rubber Cup Coronal Polishing
Polishing Cups
Soft, webbed polishing cups are used to clean and polish the smooth surfaces of the teeth (Figure 18-1). The polishing cup is attached to the reusable prophy angle by a snap-on or screw-on attachment.

Polishing cups are made from both natural and synthetic rubber. Natural rubber polishing cups are more resilient and do not stain the teeth. Synthetic rubber polishing cups are stiffer than natural polishing cups. If synthetic polishing cups are used, white synthetic cups are preferable because black synthetic cups may stain the teeth. Synthetic polishing cups should be used for patients with an allergy to latex products.
Prophylaxis Angle and Handpiece
The prophylaxis angle, commonly called a prophy angle, attaches to the slow-speed handpiece (see Chapter 19). The reusable prophy angle must be properly cleaned and sterilized after each use. (Handpiece maintenance is discussed in Chapter 19.) When attaching the polishing cup or brush to the reusable type of prophy angle, be certain that the polishing cup or brush is securely fastened. If a polishing cup or brush falls off during the procedure, the patient could swallow or inhale it.
A disposable angle is available that is discarded after a single use. This disposable angle is manufactured with a polishing cup or a brush already attached.
Handpiece Grasp
The handpiece and prophylaxis angle are held in a pen grasp with the handle resting in the V-shaped area of the hand between the thumb and index finger (Figure 18-2). A proper grasp is important because if the grasp is not secure and comfortable, the weight and balance of the handpiece can cause hand and wrist fatigue (Box 18-2).
Fulcrum and Finger Rest
The terms fulcrum and finger rest are used interchangeably to describe the placement of the third, or ring, finger of the hand that is holding the instrument or handpiece.
The fulcrum provides stability for the operator and must be placed in such a way as to allow movement of the wrist and forearm.
The fulcrum is repositioned throughout the procedure as necessary. The fulcrum may be intraoral or extraoral, depending on a variety of circumstances such as:
Improper movement of the hand and fingers greatly increases operatory fatigue and over time can cause painful inflammation of the ligaments and nerves of the wrist.
Bristle Brushes
Bristle brushes are made from natural or synthetic materials and may be used to remove stains from deep pits and fissures of the enamel surfaces. Bristle brushes can cause severe gingival lacerations and must be used with special care (Box 18-3). Brushes are not recommended for use on exposed cementum or dentin because these surfaces are soft and are easily abraded.
Abrasives
Dental abrasives (polishing materials) are used to remove stain and to polish natural teeth, prosthetic appliances, restorations, and castings.
Abrasives are available in various grits. (Grit refers to the degree of coarseness of an abrasive agent.) Abrasives are available in extra coarse, coarse, medium, fine, and extra fine. The coarser the agent, the more abrasive the surface.
Even a fine-grit abrasive agent removes small amounts of the enamel surface. Therefore the goal is to always use the abrasive agent that produces the least amount of abrasion to the tooth surface (Box 18-4).
Abrasives are available in commercial premixed pastes or in powders that are mixed with water or mouthwash to form slurry used in the polishing cup. Powder abrasives should be as wet as possible (but not runny) to minimize frictional heat. If the mixture is too wet, there will be splatter and difficulty in keeping the material in the cup. The commercial type of premixed paste is packaged ready to use.
Table 18-5 contains some of the most commonly used dental abrasives.
TABLE 18-5
| Agent | Action |
| Silex | Fairly abrasive and used for cleaning more heavily stained tooth surfaces |
| Super-fine silex | Used for removal of light stains on tooth enamel |
| Fine pumice | Mildly abrasive and used for more persistent stains, such as tobacco stains |
| Zirconium silicate | Used for cleaning and polishing tooth surfaces (this material is highly effective and does not abrade tooth enamel) |
| Chalk | Also known as whiting; chalk is precipitated calcium carbonate (it is frequently incorporated into toothpaste and polishing pastes to whiten the teeth) |
| Commercial premixed preparations | Contain an abrasive, water, a humectant (to keep the preparation moist), a binder (to prevent separation of the ingredients), flavoring agents, and color. Some commercial preparations are available in small plastic containers or individual packets that contribute to the cleanliness and sterility of the procedure. |
| Fluoride/> |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



