CHAPTER 24. Immunodeficiencies and HIV disease
Immune deficiencies can be primary or, more frequently, acquired (Box 24.1) and affect B-or T lymphocytes, or both. T lymphocytes regulate B-lymphocyte activity; T-cell defects may therefore impair antibody production as well as cell-mediated immunity. There can also be failures of production of individual immunoglobulins such as IgA, or of complement components.
Box 24.1
Important causes of immunodeficiency
Primary (genetic)
• T or B lymphocyte defects (Swiss-type agammaglobulinaemia, Di George’s syndrome, etc.)
• IgA deficiency
• Complement component deficiencies
• Down’s syndrome (multiple defects)
Secondary (acquired)
• Infections (HIV, other severe viral or bacterial infections, malaria, etc.)
• Drug-induced (immunosuppressive and anticancer treatment)
• Malnutrition (worldwide a major cause)
• Cancer (particularly lymphoreticular)
• Diabetes mellitus
Any patient who develops recurrent infections, particularly if they respond poorly to treatment or are caused by otherwise harmless microbes (opportunistic infections), is likely to be immunodeficient (Fig. 24.1).
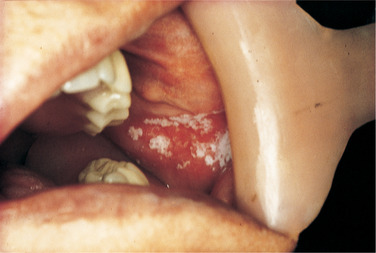 |
| Fig. 24.1
White patches of thrush and erythema in a patient on long-term immunosuppressive treatment.
|
The main causes of severe immunodeficiency are HIV infection and immunosuppressive treatment, particularly for organ transplants. Many cancer patients are also severely immunodeficient as a result of both the neoplasm and cytotoxic drugs used for treatment. The severe primary immunodeficiencies are rare and, unless a marrow transplant can be given, are usually fatal in childhood.
Oral manifestations of immunodeficiencies
The main effect, as mentioned earlier, is abnormal susceptibility to infections, particularly candidosis or viral infections such as herpes zoster as in AIDS (see below). Resistance to treatment or recurrences of such infections strongly suggest immunodeficiency as do opportunistic infections by microbes which rarely affect normal persons. General oral manifestations of immunodeficiencies are summarised in Box 24.2, but there is some variation in presentation between different causes.
Box 24.2
Important oral manifestations of immune deficiency states
Infections (some examples only)
• Herpes simplex, Herpes zoster
• Human herpes-virus 8
• Epstein–Barr virus
• Cytomegalovirus
• Candidosis
• Bacterial infections
Neoplasms
• Kaposi’s sarcoma
• Lymphomas
Other possible manifestations
• Lymphadenopathy
• Hairy leukoplakia
• Thrombocytopenia
• Lupus erythematosus
SELECTIVE IGA DEFICIENCY
Selective IgA deficiency is common and potentially relevant for the mouth, as IgA is the only immunoglobulin secreted in the saliva. Selective IgA deficiency may affect about 1 in 600 of the population and has varied possible effects (Box 24.3).
Box 24.3
Possible effects of selective IgA deficiency
• Normal health
• Enhanced susceptibility, especially to respiratory tract infections
• Atopic disease
• Connective tissue disease, especially lupus erythematosus
Susceptibility to oral infections
Evidence regarding the effect of IgA deficiency on dental caries and periodontal disease is conflicting. Both high and low prevalences of dental caries have been reported. Compensatory secretion of other immunoglobulins into the mouth may explain these variable findings. Gingivitis may be less severe than normal, but even this may be the result of antibiotic treatment for respiratory infections. There is no clear evidence of any significant association between oral mucosal infection and IgA deficiency.
Atopic disease
IgA deficiency may facilitate absorption of allergens. Asthma, eczema or any of the related diseases may be the first sign. However, this has no oral effects unless allergic angio-oedema involves the floor of mouth or lips.
C1 ESTERASE INHIBITOR DEFICIENCY
The familial form of this disease, hereditary angio-oedema, is, pedantically speaking, an immunodeficiency, but there is no abnormal susceptibility to infection. There is also a rare acquired type associated mainly with lymphoproliferative diseases. They are discussed in Chapter 25, together with allergic angio-oedema, which it simulates clinically.
LEUKOPENIA AND AGRANULOCYTOSIS
Immunodeficiency disorders are frequently associated with deficiency of circulating leucocytes. A severe fall in the leucocyte count leads to abnormal susceptibility to infection. In agranulocytosis this is typically shown initially by oropharyngeal ulceration.
IMMUNOSUPPRESSIVE TREATMENT
Bone marrow transplantation
Bone marrow transplantation is used, if suitable donors can be found, for such conditions as some severe primary immunodeficiency diseases, some leukaemias, aplastic anaemia and some lymphomas and other neoplasms. Preoperatively, total immunosuppression by cytotoxic chemotherapy and, sometimes, total body irradiation is required to prevent graft rejection.
Oral sources of infection should be eliminated and the mouth brought to as near perfect health as possible. Elimination of oral infection (particularly periodontal disease) has a significant effect on lessening post-transplant complications and also lessens the need for dental treatment during the difficult post-transplant period.
Possible complications after transplantation are numerous (Box 24.4), particularly during the initial intensive phase of immunosuppression.
Box 24.4
Possible complications of bone marrow transplantation
• Oral complications
Mucositis, mucosal ulceration, infections, haemorrhage, dry mouth, parotitis
Gingival hyperplasia if cyclosporin is used
In children, dental hypoplastic defects may develop
• Graft-versus-host disease
• Systemic infections (sometimes by oral bacteria). These are the chief cause of death
• Tumours such as Kaposi’s sarcoma or lymphomas
Graft-versus-host disease
This results from an attack on an immunosuppressed host by transplanted immunocompetent cells. It is, in effect, a graft rejection reaction in reverse. It most frequently follows bone marrow transplantation, both because of the deep immunosuppression and because of the many immunologically active cells in the implanted marrow.
The oral effects of graft-versus-host disease are lichen planus, a Sjögren-like syndrome with xerostomia, and a condition resembling systemic sclerosis (Ch. 25) with limited oral opening.
Graft-versus-host disease can be acute and self-limiting or responsive to treatment, or chronic. The last is the chief cause of morbidity and mortality.
Post-transplant management
The main considerations are maintenance of meticulous oral hygiene, use of fluorides to control caries and prompt treatment of any infections that develop.
In successful cases, deep immunosuppression is maintained for up to a year post-transplantation. The implanted marrow then takes over normal haematological and immune functions. Any oral surgery should preferably be postponed until this happens.
OTHER ORGAN TRANSPLANTS
Transplantation of other organs, most frequently kidneys, is associated with similar complications to those of bone marrow transplantation. The main differences are that immunosuppression is less complete but has to be maintained indefinitely.
THE ACQUIRED IMMUNE DEFICIENCY SYNDROME (AIDS)
A great variety of oral diseases can be features of the acquired immune deficiency syndrome (see Table 24.3). They sometimes form the first sign of the disease and some of them herald rapid deterioration and, sometimes, early death.
| More common diseases | Less common | |
|---|---|---|
| Infections |
Fungal
Thrush and other forms of candidosis
|
Deep mycoses
Cryptococcosis
Histoplasmosis
Aspergillosis
Geotrichosis
|
|
Viral
Herpes simplex
Varicella-zoster
EB virus, including hairy leukoplakia
|
Viral
Human papillomavirus
Cytomegalovirus
|
|
|
Bacterial
HIV-associated gingivitis and periodontitis
Necrotising gingivitis
|
Bacterial
M. tuberculosis and non- tuberculous (‘atypical’) mycobacterioses
Klebsiella pneumonia
S. enteritidis, E. coli and E. cloacae infections
Sinusitis
Exacerbations of apical periodontitis
Submandibular cellulitis
|
|
| Tumours | Kaposi’s sarcoma | Non-Hodgkin lymphoma (squamous cell carcinoma) |
| Other | Lymphadenopathy |
Neurological disease
Paraesthesiae
Hyperaesthesia
Facial palsy
Dysphagia
|
| Miscellaneous | ||
|
Recurrent aphthae
Progressive necrotising ulceration
Delayed wound healing
Purpura
Pigmentation
|
HIV disease has spread worldwide and is epidemic in parts of the USA and, particularly, Africa. More than 40 million adults, worldwide, are estimated to be infected. Innumerable children, particularly in Africa, have been orphaned by or have acquired the disease. The pandemic is most severe in sub-Saharan Africa where 25 million adults, approximately 9% of the population, are infected. As indicated in Table 24.1, it is estimated that by 2005 there were 2.4 million deaths from AIDS in sub-Saharan Africa alone.
| New infections during 2005 | Total deaths 2005 | |
|---|---|---|
| Sub-Saharan Africa | 3.2 million | 2.4 million |
| North America | 43000 | 18000 |
| Western and Central Europe | 22 000 | 12 000 |
| Eastern Europe and Central Asia | 270 000 | 62 000 |
| South and South-East Asia | 990 000 | 480 000 |
In the former Soviet Union, cases have risen to 700 000, a jump of nearly 70% in one year and it is predicted that one million Russians will have become infected within two or three years. Worldwide, the numbers of persons already infected but who have not yet developed AIDS for some areas is suggested in Table 24.1. Overall, the numbers of children and adults newly infected is estimated to be 4.9 million and the global total of persons living with HIV is estimated to be 40.3 million. The total number of deaths by 2005 is estimated to be 3.1 million.
However, there may be little purpose in quoting such figures as the disease will have claimed many more victims by the time this is read.
AIDS is transmissible to health care personnel, particularly surgeons, dental surgeons and nurses, via needles or other sharp instruments. However, the risk of acquiring HIV infection by such means is considerably smaller than that of hepatitis B.
Aetiology
AIDS is caused by a retrovirus, the human immunodeficiency virus (HIV), mainly HIV-1. HIV-2 is prevalent in West Africa, from where it has spread to central Africa. HIV-2 infection may progress more slowly and cause less deep immunosupression
The chief mode of transmission in many parts of the world is by men who have sex with men. These used to account for over 80% of cases in Britain, but this figure has greatly declined in recent years. In the UK, 28% of cases of HIV infection are in men who have sex with men, 0.01% are in intravenous drug abusers and in 55% there has been heterosexual transmission. Heterosexual transmission is far less common in the Western World than in Africa. Nevertheless, as a result of spread of the virus in the population, heterosexual transmission has become more frequent. The great rise in the frequency of heterosexual transmission in the UK in recent years has been affected by a variety of factors. In most cases, this is the result of migration of individuals who have acquired the infection in high-risk areas. However, an increasing proportion of this heterosexual infection is acquired in the UK. Once infected, pregnant women can transmit the infection to the fetus directly or by breast feeding. Many haemophiliacs have acquired the disease from infected blood products but heat-treatment of clotting factor concentrates should have eliminated this risk and there appear to have been no cases among them or other transfusion recipients in the UK in recent years.
The incubation period of AIDS is highly variable. In men who have sex with men, the average is approximately 5 years, but is sometimes as long as 10 years. Testing of infected persons also shows deterioration of immune function long before clinically apparent disease and it is still not clear whether all those who have become infected will develop the full, lethal syndrome.
In 5–15% of cases, HIV infection shows no clinical progress for periods up to 10 years, possibly because of variations in pathogenicity of HIV strains, or stronger host immune responses.
Immunology
The human immunodeficiency virus directly infects lymphocytes and other cells, such as some macrophages, which carry the CD4 marker. However, the virus appears only to be able to fuse with and enter CD4 cells as a result of interaction between the gp120 envelope proteins and a CD4 binding site by means of a family of co-receptors. The virus kills T-helper (CD4) cells and reverses the ratio of helper to suppressor lymphocytes.
Antibody is produced in response to the virus but is not protective. Antibodies to HIV indicate only that infection has been acquired and all seropositive persons must be assumed to be capable of transmitting it.
The main effect of depletion of T-helper cells is deepening depression of cell-mediated immunity. Thus, there are declining responses of lymphocytes to antigens in vitro and impaired or absent delayed hypersensitivity responses long before any clinical signs of the disease appear. Apparently paradoxically, there is also polyclonal B-lymphocyte activation resulting in hypergammaglobulinaemia and autoantibody production. The main effect of the immunodeficiency and chief cause of death is infection by a great variety of microbes.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


