CHAPTER 22 Root Form Implant Prosthodontics: Abutments
After second-stage surgery has been completed, and the healing collars have been removed, the final restoration is started. To affix a final prosthesis to the implants, abutments must be used as intermediate devices. In most implant systems (two surgical stages), abutments are the components that extend through the gingival tissues overlying the implants. For implants placed in a single-stage procedure (e.g., implants by Nobel Biocare, BioHorizons, and Park Dental Research), the abutments, when attached, are positioned above the exposed gingival cuffs (see chapters 10 and 11).
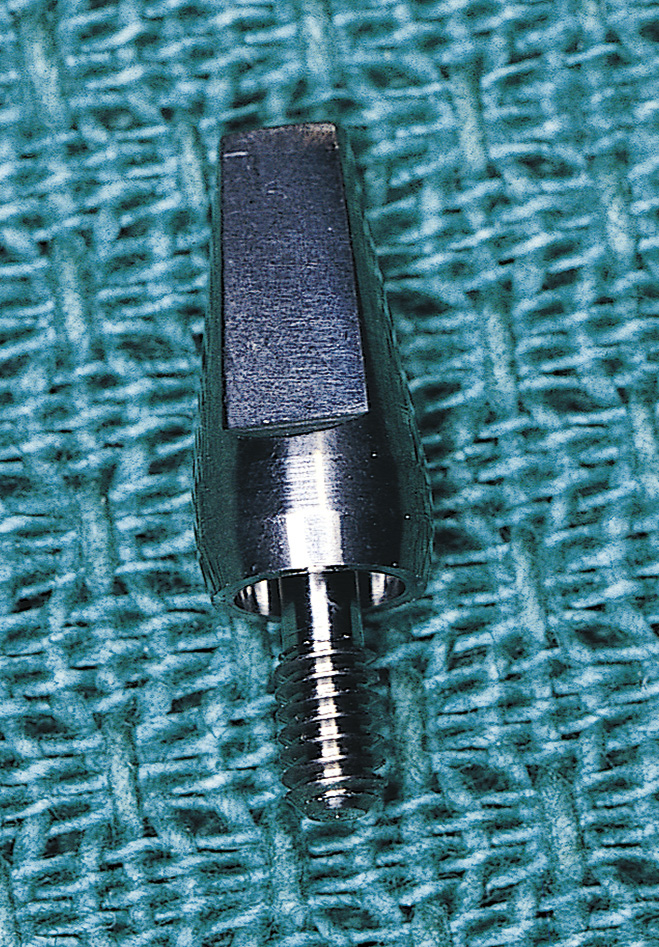
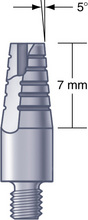
Abutments may consist of a single unit (Fig. 22-1); two pieces (Fig. 22-2); or three pieces. The parts of the three-piece abutment, which may be separate or unified, are the base, which fits into the antirotational component of the implant; the head, which protrudes permucosally and serves as the prosthetic retainer; and the retaining screw, which affixes the other two parts to the implant.
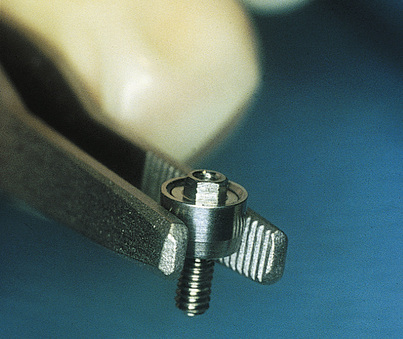
FIGURE 22-2. The Nobel Biocare abutment has a center screw and an outer housing that fits over the external hex of the implant.
Abutments can be obtained from the manufacturer in machined form, or they can be custom cast by a laboratory using manufactured gold or plastic components. Several recently introduced variations include ceramic, zirconium and other wide esthetic abutments. Tables 22-1 and 22-2 list the specific characteristics of each company’s spectrum of available abutments for screw-retained and cementable crowns and copings. In this atlas, implant abutments are referred to as transepithelial abutments (TEAs).
| Name | Straight | Angled | Custom Cast | Esthetic | Other |
|---|---|---|---|---|---|
| Astra Tech | + | + | + | a, b, c, d | |
| Bicon | + | + | + | ||
| BioHorizons | + | + | + | d | |
| Biomet-3i | + | + | + | a | |
| Camlog | + | + | + | a | |
| Implant Direct | + | + | + | ||
| Imtec | + | + | |||
| Innova | + | + | + | a | |
| Lifecore | + | + | + | ||
| MIS | + | + | + | a, b, c, d | |
| Neoss | + | + | + | a, b | |
| Nobel Biocare | + | + | + | c | e |
| Park Dental | + | + | + | ||
| Sargon | + | + | + | ||
| Straumann | + | + | |||
| Zimmer | + | + | + | a |
+, A feature of this implant.
a, Wide emergence profile.
b, Tooth-shaped bioesthetic abutments.
c, Prepable ceramic inverse cone, allows for up to 20-degree angulation.
d, Prepable titanium inverse cone, allows for up to 20-degree angulation.
Table 22-2 Abutment Options for Screw-Retained Prostheses
| Name | Flat Top | Tapered | Tapered Angled | Direct Gold |
|---|---|---|---|---|
| Astra Tech | + | + | ||
| Bicon | ||||
| BioHorizons | + | + | ||
| Biomet-3i | + | + | + | + |
| Camlog | + | + | + | + |
| Implant Direct | + | |||
| Imtec | + | |||
| Innova | + | + | ||
| Lifecore | + | + | + | |
| MIS | + | + | + | |
| Neoss | + | + | + | |
| Nobel Biocare | + | + | + | + |
| Park Dental | + | + | ||
| Sargon | + | |||
| Straumann | + | |||
| Zimmer | + | + |
+, A feature of this implant.
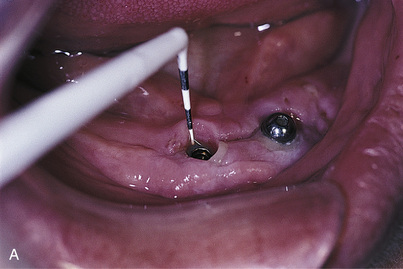
Wherever esthetics allows, the margins of final restorations should be placed 2 mm above the gingival tissues. This provides easier access for oral hygiene and minimizes the risk of gingival inflammation, which can lead to implant pericervical saucerization. In such areas, a TEA is selected that will put the planned crown margin at an optimum location. This location is determined by placing a plastic periodontal probe along the gingival margin adjacent to the healing collar and down to the cervix, or by using the collar itself as a guide. The proper collar height is established by adding 2 mm to that measurement (Fig. 22-3). This can be done by the laboratory technician or the surgeon. (Chapter 24 presents the steps required to transfer an implant to a cast.)
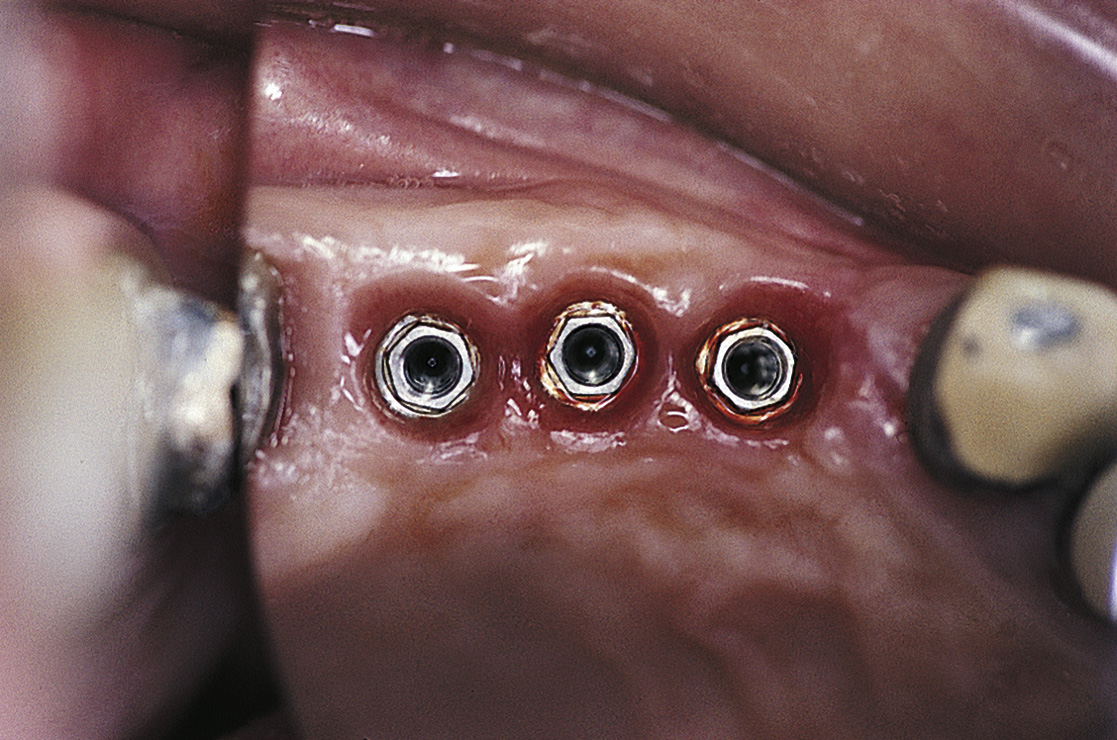
In some cases, the cervix of an implant is already level with the gingival tissues or possibly slightly below them (Fig. 22-4), and no space has been left for a collar. In these cases, an esthetic restoration is made by fabricating a crown directly to the head of the implant. This commonly is done by using a manufactured gold or polymeric coping (described later in the chapter).
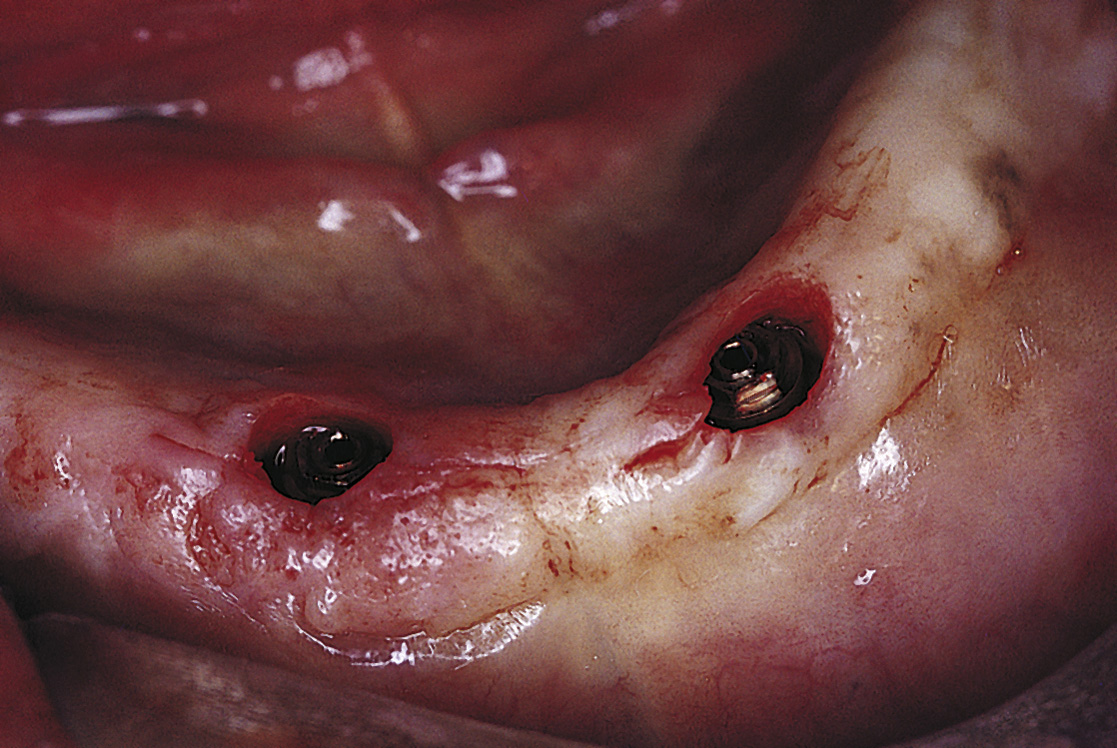
FIGURE 22-4. These implants have cervices at the tissue level and may require custom-cast abutments for an esthetic restoration.
Another alternative, which allows cementation of the prosthesis, is to insert the abutment with a torque wrench and prepare the implant-abutment combination intraorally with a tapered diamond bur and copious irrigation, creating a subgingival margin. Some systems do not have an abutment or attachment designed to satisfy the surgeon’s every requirement. A wide variety of abutments are made with internal thread patterns (Fig. 22-5) and matching antirotational bases that are compatible with implants made by several manufacturers. The abutments of different companies (e.g., Biomet-3i, BioHorizons), therefore, can be substituted if they provide a required angulation, dimension, or emergence profile.
CEMENT VERSUS SCREW RETENTION OF ABUTMENT-BORNE PROSTHESES
Cement Retention
Advantages of Cement Retention
Cement retention offers many benefits, including the following:
Disadvantages of Cement Retention
Cement retention does have some potential shortcomings as well:
Screw Retention
Proponents of screw retention cite retrievability as this method’s major advantage. Screw-retained prostheses also offer other benefits that deserve serious consideration. The primary advantage is greater prosthetic flexibility. Although cementation is used primarily for conventionally designed crown and bridge prostheses (whether single tooth or full arch), they lose efficacy if height is insufficient. In such cases, screw retention allows the use of short or low-profile abutments. In addition, screws provide reliable security when mesostructure bars (see Chapter 26) of limited vertical dimension are made quite close to the mucosa, and screws offer reliable support to hybrid prostheses, which must be removed for hygiene (see Chapter 24) (Fig. 22-6).
ATTACHMENT OF ABUTMENTS TO THEIR IMPLANTS
Abutments for Flat-Surfaced Implants
Abutment-implant interfaces vary, depending on whether antirotational devices are included. Implants that do not have antirotational elements are flat surfaced and usually require attachment of one-piece abutments (Fig. 22-7). Traditionally, these implants are used only when multiple units are to be splinted by connecting their overlying crowns or bars, which generally are cement retained, preventing abutment malrotation. However, flat-surfaced implants should not be used for single-tooth restorations, because the lack of an antirotational feature results in persistent loosening of the abutment and prosthesis.
Abutments for Implants with Antirotational Features
Antirotational Features of Various Implant Systems
Antirotational features on implants prevent unwanted movement of the overlying abutment. Antirotational features currently used include the external hex, the internal hex, the spline-type interface, the Park star, and the Morse taper. Table 22-3 shows the distribution of these features in the various implant systems.
Table 22-3 Antirotational Connection Between Implants and Abutments
| Name | External Hex | Internal Hex | Spline | Morse Taper |
| Astra Tech | + | |||
| Bicon | + | |||
| BioHorizons | + | |||
| Biomet-3i | + | |||
| Camlog | + | + | ||
| Implant Direct | + | |||
| Imtec | + | |||
| Innova | + | |||
| Lifecore | + | |||
| MIS | + | |||
| Neoss | + | |||
| Nobel Biocare | + | |||
| Park Dental | + | + (internal) | ||
| Sargon | + | |||
| Straumann | + | |||
| Zimmer | + | + (external) |
+, A feature of this implant.
External Hex
The external hex (Fig. 22-8) is the second most widely available antirotational feature in implants. This design offers a wide variety of restorative options because of the interchangeability of abutments among manufacturers. For example, the hexagonal geometry atop the Lifecore implant is compatible with the abutments available for Biomet-3i implants.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses