CHAPTER 22
Mandibular Osteotomies
Brian B. Farrell and Myron R. Tucker
Private Practice, Carolinas Center for Oral and Facial Surgery, Charlotte, North Carolina, USA; and Department of Oral and Maxillofacial Surgery, Louisiana State University Health Science Center, New Orleans, Louisiana, USA
Sagittal Ramus Osteotomy (Bilateral Sagittal Split Osteotomy)
A means of surgically repositioning the lower jaw through mandibular osteotomies.
Indications
- The correction of congenital dentofacial deformities, including mandibular deficiency, hyperplasia, asymmetry, and dysgnathia
- The correction of acquired dentofacial deformities resulting from facial trauma, tumor ablative surgery, and tempomandibular joint asymmetries and deformities
Contraindications
- Distorted ramus anatomy (thin or abnormal shape)
- Excessive counterclockwise rotation (greater than 2 cm apertognathia requires two-jaw surgery)
- Mandibular advancements greater than 12 mm
- Neurosensory concerns
- Previous head and neck radiation
Anatomy
- Retrolingual depression: A depression located on the lingual aspect of the mandible between the lingula and the posterior border of the mandible.
- Lingula: Entrance of the neurovascular bundle into the mandibular canal. The sagittal ramus osteotomy is initiated superior to the lingula.
- Antelingula: Prominence along the lateral ramus predicting the position of the lingula on the medial aspect of the ramus.
- Inferior alveolar nerve: Neurovascular bundle which enters the mandibular canal adjacent to the lingual, and exits the mandible anteriorly at the mental foramen.
Sagittal Ramus Osteotomy
Technique
- The patient is nasally intubated, and the tube is secured. A throat pack is positioned at the level of the hypopharynx.
- Local anesthetic containing a vasoconstrictor is injected along the external oblique ridge, retromolar trigone, and posterior buccal vestibule.
- The patient is prepped and draped in the standard sterile fashion to include the oral cavity and maxillofacial skeleton.
- Preplanned enameloplasty is performed, and a posterior bite block is placed.
-
A #15 blade is used to initiate an incision through mucosa only, positioned 2–3 cm lateral to the external oblique ridge (Figure 22.5, Case Report 22.1). The soft tissue is reflected medial over the external oblique ridge exposing the underlying muscle (Figure 22.6, Case Report 22.1). A sharp dissection proceeds to the lateral ramus transecting muscle and periosteum.
- A periosteal elevator is used to dissect within a subperiosteal plane to expose the lateral mandible anteriorly to the Dalpont prominence adjacent to the molars. The dissection continues posteriorly to expose the external oblique ridge and the superior portion of the ascending ramus. A sigmoid notch retractor is positioned to elevate and retract the temporalis attachment from the ascending ramus. Subperiosteal dissection continues on the medial surface of the mandible, creating a subperiosteal pocket superior to the lingula. The inferior alveolar neurovascular bundle is identified. Identification can be accomplished by direct visualization or by palpation of the lingula with a nerve probe.
- A Seldin retractor is placed within the lingual subperiosteal pocket and rotated 45° to protect the inferior alveolar neurovascular bundle and to create a space for the insertion of the reciprocating saw (Figure 22.7, Case Report 22.1).
- A reciprocating saw initiates the horizontal osteotomy of the medial cortex at a 45° angle (the cut may be more vertical if the ramus is thin) (Figure 22.8, Case Report 22.1). The tip of the saw should extend into the retrolingular depression with the blade at full depth to score the osteotomy superior to the neurovascular bundle (Figure 22.1; see also Figure 22.2).
- The osteotomy is extended anteriorly through the cortical bone medial to the external oblique ridge and lateral to the dentition. The osteotomy is extended to the bony prominence located along the buccal aspect of the molar region (Dalpont prominence) (Figure 22.9, Case Report 22.1).
- The bite block is removed. A channel retractor is placed along the inferior border of the mandible along the anterior aspect of the Dalpont prominence. The channel retractor is rotated 45° to expose the inferior border of the mandible, allowing for the insertion of the reciprocating saw.
- The vertical osteotomy is initiated at the anterior aspect of the Dalpont prominence at the inferior border and transects both the buccal and lingual cortical plates inferior to the mandibular canal. The osteotomy continues vertically as a tangential cut through the lateral cortex only to connect the osteotomy along the external oblique ridge (Figure 22.10, Case Report 22.1).
- The bite block is returned to stabilize the mandible during the separation of the mandible into proximal and distal segments. During separation (splitting) of the sagittal ramus osteotomy, the osteotomy should be visualized along its entire length to ensure equal separation throughout.
- Osteotomes are used to facilitate the initial separation of the osteotomy (Figure 22.11, Case Report 22.1). Care is taken to avoid using the osteotomes as a fulcrum posterior to the dentition to prevent the development of a lingual plate fracture within the distal segment.
- After initial separation, larger osteotomes or spreaders are used within the osteotomy to provide equal separation and to complete the split. Care is taken to ensure that the inferior border is associated with the proximal segment (Figure 22.12, Case Report 22.1). The inferior border of the mandible provides structural integrity to the proximal segment, aiding in avoiding unfavorable fractures.
- The neurovascular bundle is identified early to ensure proper positioning and to avoid further iatrogenic injury with instrumentation between the osteotomy.
- The nerve typically will course within the distal segment and require minimal manipulation (Figure 22.13, Case Report 22.1). Occasionally, the nerve will remain encased within the mandibular canal in the proximal segment and requires release by removal of the overlying bone. Elevators and/or osteotomes may be used to free the nerve and allow positioning within the confines of the distal segment.
- The muscular and tendinous attachments of the medial pterygoid muscle are released with a J stripper from the inferior and medial aspect of the distal segment to ensure passive repositioning of the mandible. Mandibular setback surgery will require release of soft tissue from the medial aspect of the proximal segment to create a pocket for the repositioned distal segment.
- Maxillomandibular fixation (MMF) is established using the prefabricated occlusal splint with 24– or 26-gauge stainless steel wires.
- Passive positioning of the proximal and distal segments is confirmed. Bony interferences are removed with saws, burs, and rasps to improve bone contact (Figure 22.14, Case Report 22.1).
- The inferior borders of the mandible are aligned, and the condyles are seated with firm pressure in a posterior-superior vector.
- Fixation can be applied using percutaneous (Figure 22.15, Case Report 22.1) or transoral access. Trocar positioning is determined by passing a local anesthetic needle through the skin followed by a stab incision with a #15 blade. The trocar allows placement of rigid internal fixation perpendicular to the cortex.
Fixation options include positional screws placed in a line at the superior border (Figure 22.15, Case Report 22.1, and Figure 22.24, Case Report 22.2) or in an inverted L pattern (Figure 22.2). Stability of the osteotomy is improved with spacing of the positional screws over the span of the osteotomy. Plates with monocortical fixation may be placed on the lateral border of the mandible. A combination of bicortical positional screw(s) and plates may be used if there is inadequate bone available in the distal segment for isolated screw fixation (concomitant third molar removal) (Figure 22.21, Case Report 22.2) or in cases of long advancements with limited bony overlap (Figure 22.16, Case Report 22.1).
- At the completion of fixation, MMF is released and the occlusion is verified. Deviation of the occlusion to one side may indicate failure to seat the condyle and requires removal of fixation on the affected side with repositioning of the proximal segment.
- The trocar incision is closed with a single interrupted suture. The intraoral incisions are closed with resorbable sutures (Figure 22.17, Case Report 22.1).
- The throat pack is removed, and the surgical splint is removed. Guiding elastics may be utilized to facilitate neuromuscular guidance and reprogramming. A pressure dressing is applied to aid in control of postoperative edema.

Figure 22.1. The Hunsuck modification involves splitting the mandible anterior to the posterior border by placing the reciprocating saw within the retrolingual depression superior to the insertion of the inferior alveolar nerve and lingula.
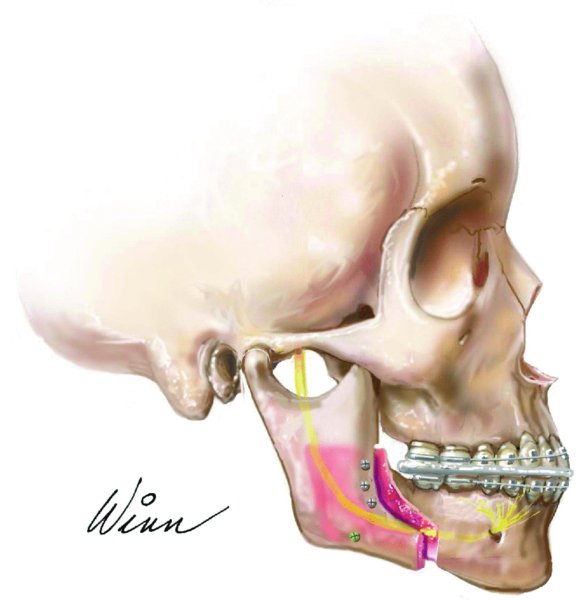
Figure 22.2. Illustration depicting a favorable sagittal ramus osteotomy split (Hunsuck modification), mandibular advancement, and fixation with positional screws.
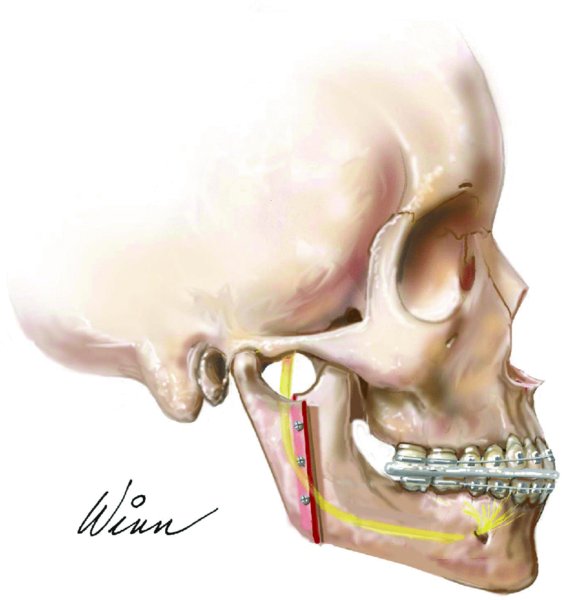
Figure 22.3. Illustration depicting a favorable vertical ramus osteotomy split, mandibular setback, and fixation with vertically oriented positional screws.

Figure 22.4. Preoperative image depicting a class II deep bite malocclusion and mandibular retrognathia.

Figure 22.5. Incision initiated through mucosa only positioned 2–3 cm lateral to the external oblique ridge.
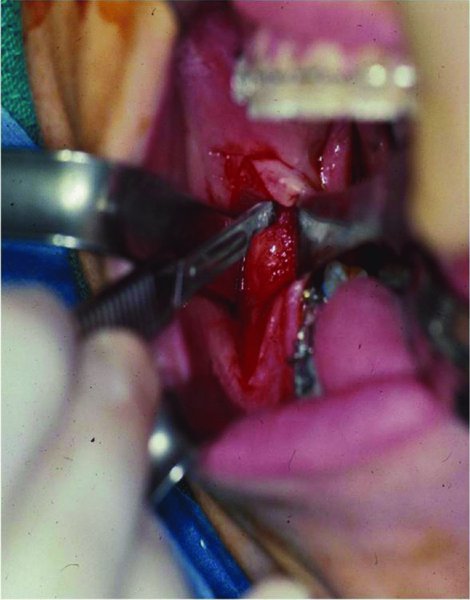
Figure 22.6. The soft tissue is reflected medially over the external oblique ridge exposing the underlying muscle. A #15 blade is used to transect the overlying muscle and periosteum to expose the lateral ramus.

Figure 22.7. A subperiosteal tissue pocket is created along the retrolingual depression to visualize the inferior alveolar nerve and />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


