Chapter 21
Surgical endodontics
Introduction
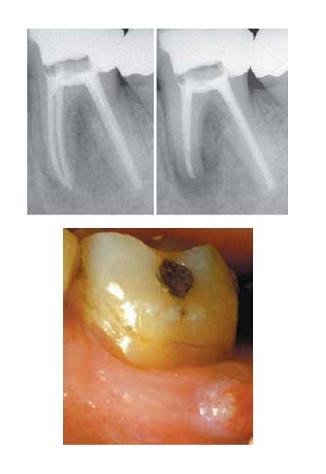
Microorganisms lodging in root filled canals may cause endodontic treatment failure. In order to eradicate the microbes in such cases, the root canal system has to be renegotiated and retreated. If the canals are poorly filled and fairly easy to access, an orthograde route of re-entry is generally to be preferred (Chapter 20). However, in many cases non-surgical retreatment may not be feasible from technical as well as financial aspects. Furthermore, an endodontic treatment failure might be caused by factors located outside the root canal, such as microorganisms colonizing the periapical tissues, cysts and foreign body reactions (Chapter 7). In such cases a surgical approach to retreatment may be considered (Fig. 21.1).
Although extensively debated over the years, there is little evidence to suggest that cysts are unable to heal following conventional endodontic therapy. Nair (42) has drawn attention to the fact that some radicular cyst cavities do not connect directly with the root canal space. These so-called true radicular cysts are therefore thought to be autonomous processes and not likely to respond to conventional therapy. From a clinical point of view, however, there are no means by which the existence of such a pathological condition can be determined. Consequently, all radiolucent lesions associated with non-vital pulps, whether cyst or not, should be seen as treatable by conventional means and be subjected to surgery only if healing by orthograde root canal treatment cannot be attained.
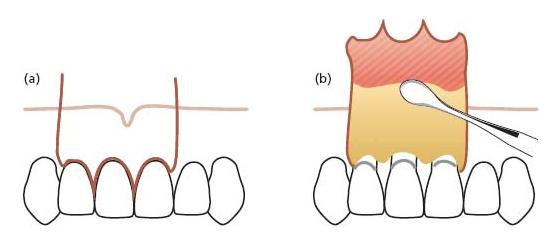
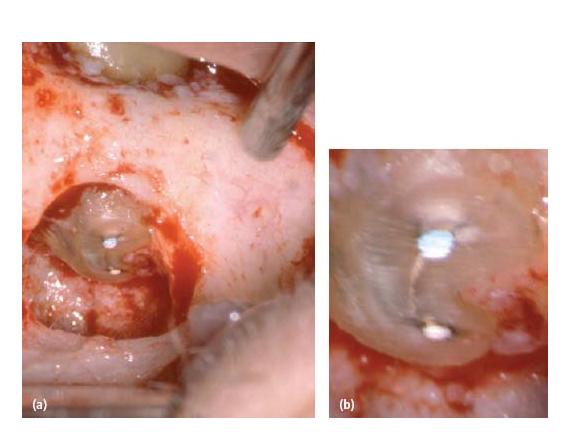
Fig. 21.1 (a) Clinical photograph showing access to the root tips of a lower first molar in an endodontic surgical procedure, at which a root tip resection was carried out. (b) High-power magnification of the resected surface showing the buccal and lingual canal with gutta-percha and isthmus between the canals.
In surgical endodontics the procedural objectives are to expose the root tip and the periapical tissues with the treatment aim to restrain a potential intracanal infection (usually the root tip is cut and the apical part of the canal is instrumented and sealed). Core concept 21.1 summarizes the typical indications for surgical retreatment.
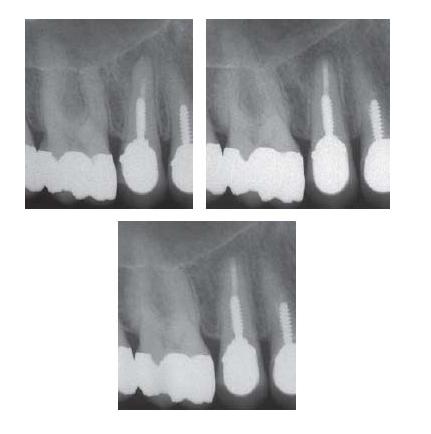
- Blocked root canal in an esthetically satisfactory post-supported crown restoration with a good marginal adaptation that could not be removed. The top-right radiograph was taken immediately postoperatively and the bottom radiograph, taken after 1 year of follow-up, shows apical healing.
- Apical root canals blocked by ledge.

- Grossly overinstrumented and overfilled canal.

- Failed treatment in spite of adequate root filling. Persistence of a fistula.
General outline of the procedure (Core concept 21.2)
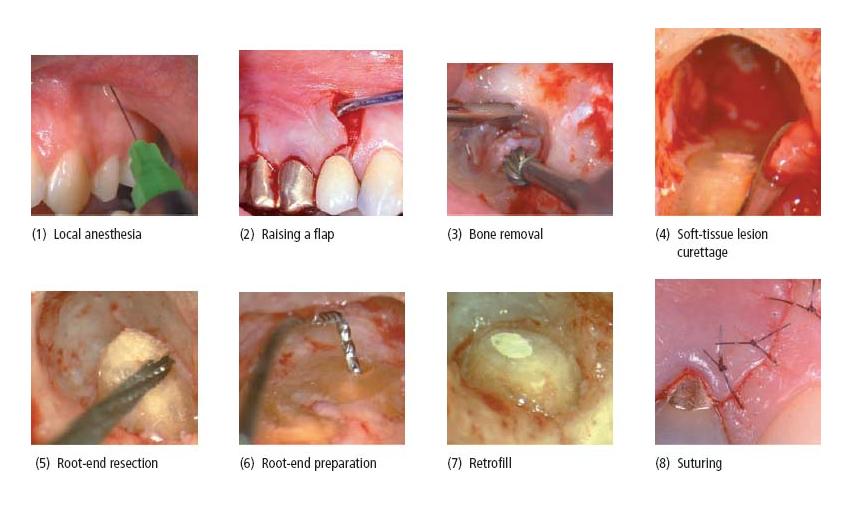
Following local anesthesia (step 1) a mucoperiosteal flap is raised (step 2). If the periapical tissue response has not perforated the cortical bone plate, bone has to be removed (step 3) to provide access to the root tip. The soft-tissue lesion is then curetted (step 4) and the root tip is cut (step 5). A root-end preparation is made (step 6) and a filling (retrofill) is placed (step 7). The surgical procedure is finished with meticulous cleaning of the wound area and repositioning and suturing of the flap (step 8).
Local anesthesia
Proper pain control is required to perform surgical endodontics. Normally the procedure can be conducted under local anesthesia.
Choice of anesthetic agent
Anesthetic agents are most effective in a non-ionized form within a pH range near 7.4. In this state the drug can easily penetrate the nerve membranes and displace the calcium ions at the membrane receptor sites. The sodium channels are then blocked and upon nerve stimulation the membrane will remain in a polarized state. In acutely inflamed tissue the pH is lowered. In such an environment the anesthetic may remain in ionized form. The result can be lesser penetration of the drug, leading to inadequate anesthesia. This is one possible explanation for the deficient pain control sometimes experienced when operating on acutely inflamed tissue. If possible, endodontic surgery should therefore not be performed in such instances. There are several anesthetics suitable for surgical pain control. Because allergic reactions to anesthetic drugs occur mainly to ester-based agents (such as procaine) (23), anesthetics based on amide groups are preferred. Good and profound anesthesia can generally be obtained with articaine, lidocaine and bupivacaine.
Vasoconstrictors
A vasoconstrictor added to local anesthetics reduces the blood flow at the injection site. This serves two important purposes:
- To retain the agent longer in the tissue, thereby extending the time for the anesthetic effect.
- To enhance hemostasis.
The reduced blood flow will also decrease absorption of the anesthetic and minimize systemic toxic effects.
The most widely used vasoconstrictor is epinephrine. This sympathomimetic agent causes vasoconstriction by stimulating specific membrane-bound receptors on the vascular smooth-muscle cells. The pharmacological action of epinephrine depends largely on the type of receptors present in the tissue. There are two types of adrenergic receptors: alpha vasoconstrictive and beta vasodilating receptors. Similar to mucosal and gingival tissues, alphaadrenergic receptors predominate in the apical periodontium. Thus, upon its penetration to these tissue sites, the effect of epinephrine will be contraction of blood vessels. In skeletal muscles, on the other hand, vessels are controlled by beta-adrenergic vasodilating receptors (38). This means that injection of epinephrine to muscle tissue will result in increased blood flow and cause the opposite of the desired hemostatic effect (3). For this reason, the anesthetic should be administered to mucosal tissue only and close to the bone in the area in focus for the operation.
Concentrations of vasoconstrictor among anesthetic solutions vary between 1 : 50 000 and 1 : 200 000. The higher the concentration, the better the hemostatic effect. Most widely used is the concentration 1 : 100 000–200 000. Although this concentration is adequate for non-surgical needs (29), it will not produce sufficient hemostasis for surgical procedures. For this purpose, at least 1 : 80 000 or rather 1 : 50 000 is recommended. It has been found that the use of 1 : 50 000 epinephrine results in good visualization of the surgical site, reduced surgery time and decreased postoperative bleeding and blood loss (3). High concentrations of epinephrine may cause an undesirable increased heart rate, cardiac contractility and peripheral vascular resistance. These systemic effects can be reduced by using several measures (see Core concept 21.3).
It should be realized that sufficient hemostasis can be achieved only if the anesthetic has reached the tissue. Therefore, with inferior alveolar nerve blocks additional anesthetic must be administered to the surgical site to obtain adequate hemostasis, even though blood flow peripheral to such nerve blocks becomes reduced (27).
Raising the flap
The success of any surgical procedure depends largely upon the extent to which adequate access can be obtained. Endodontic surgery first requires exposure of the bone overlying the tip of the root(s) and then the root end(s) per se (Fig. 21.1). To access the bone, a full- thickness flap must be raised. This means a soft-tissue flap, which consists of gingival and mucosal tissue as well as periosteum. To mobilize the flap various modes of incision can be selected, including horizontal incisions (sulcular and submarginal) and vertical releasing incisions.
It is critical that incisions and flap elevations are carried out in a manner such that soft-tissue healing by primary intention is facilitated. This is secured by:
- complete and sharp incision of the tissues;
- avoiding tearing of the tissues during flap elevation;
- preventing drying of the tissue remnants on the root surface during the procedure (see further below).
Proper treatment of the soft tissues with adequate surgical techniques is also a challenge from an esthetic point of view. Incorrect manipulation of soft tissues in areas with restoration margins placed subgingivally for esthetic reasons can, for example, lead to exposure of these margins because of recession following the surgery. Therefore, the presence, type and quality of restorations, especially with regard to the position of the restoration margin in relation to the gingiva, must be carefully assessed prior to surgery, as they are critical to the esthetic outcome of the procedure.
Flap designs
Triangular flap: A horizontal incision extending one tooth distally and one tooth mesially to the involved area, combined with only one vertical releasing incision (Fig. 21.2), forms the triangular flap. The main advantage of this flap design is easy repositioning and minimal disruption of the vascular supply to the flap. It is indicated for correction of marginally located processes such as perforations, cervical root resorptions or resections of very short roots. If it turns out that the access is too limited, the triangular flap can be converted easily to a rectangular flap by placing an additional releasing incision at the distal end of the horizontal incision (see below).
Rectangular flap: The rectangular flap is formed by a horizontal incision with two vertical releasing incisions (Fig. 21.3) and is the most frequently used flap in endodontic surgery. The rectangular flap will give excellent surgical access to the apical area in any region. In esthetically critical areas with prosthetic restorations involving submarginally placed crown margins, a postoperative sequela can result in recession, leading to exposure of the crown margins. Using a proper atraumatic and gentle surgical technique with proper wound management minimizes such esthetic disadvantages.
Fig. 21.2 (a) A triangular flap requires a sulcular incision, usually with mesial placement of the vertical releasing incision. (b) Flap reflected.
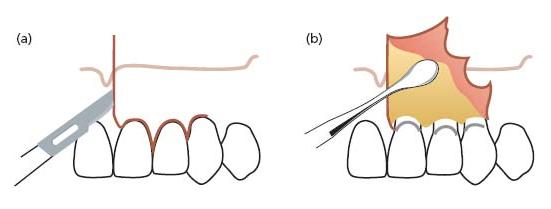
Fig. 21.3 (a) A rectangular flap involves two releasing incisions combined with a marginal sulcular incision. The releasing incisions are placed at least one tooth away from the tooth to be operated on, except in the area of the mental foramen, which should not be subjected to vertical incisions. (b) Flap reflected.
Submarginal flap according to Ochsenbein–Luebke: The submarginal flap is formed by a scalloped horizontal submarginal incision with two vertical releasing incisions (Fig. 21.4). The submarginal flap is only to be used when there is a broad attached gingiva and when the expected apical lesion or surgical bony access will not involve the incision margins. This flap design has the advantage of preserving the marginal gingiva and does not expose the marginal crestal bone.
As well as the risk of massive loss of marginal tissue due to a possible insufficient blood supply to the un reflected gingival tissue (see above), the risk of scarring is another disadvantage of this flap design. Owing to drying out of the tissue the flap tends to shrink during surgery, resulting in tension and difficulty in replacing and securing it by suturing.
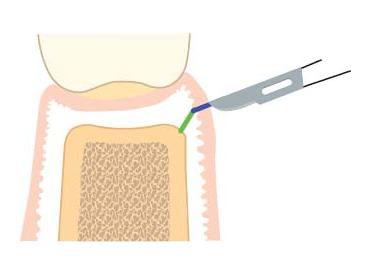
Papilla-base flap: This flap consists of two releasing vertical incisions, connected by the papilla base incision and intrasulcular incision in the cervical area of the tooth. It was designed to prevent recession of the papilla. A microsurgical blade of a size not exceeding 2.5 mm in width should be used. Controlled and minute movement of the surgical blade within the small dimensions of the interproximal space is crucial. The papilla base incision requires two different incisions at the base of the papilla. A first shallow incision severs the epithelium and connective tissue to the depth of 1.5 mm from the surface of the gingiva (Fig. 21.5, blue line). The path is a curved line, connecting one side of the papilla to the other. The incision begins and ends perpendicular to the gingival margin (Fig. 21.6). In the second step, the scalpel retraces the base of the previously created incision while inclined vertically, towards the crestal bone margin. The second incision results in a split-thickness flap in the apical third of the base of the papilla (Fig. 21.5). From this point on apically, a full-thickness mucoperiosteal flap is elevated (Fig. 21.7). Although the papilla base flap achieves predictable healing results, this technique requires a skilled surgeon. Atraumatic handling of the soft tissues is of utmost importance in order to obtain rapid healing through primary intention. The epithelium of the partial-thickness flap has to be supported by underlying connective tissue, otherwise it will break down and lead to scar formation. On the other hand, excessive thickness of the connective tissue layer of the split flap portion can jeopardize the survival of the buccal papilla left in place (59).
Fig. 21.4 An Ochsenbein–Luebke flap is raised by placing a scalloped horizontal incision within the attached gingiva, reflecting the gingival and mucosal tissues (37). For vertical incisions, the same rules apply as for the rectangular flaps.
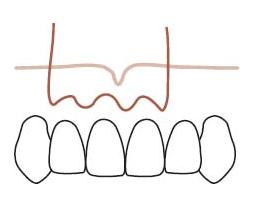
Fig. 21.5 Schematic drawing of incision type for the papilla base flap. The first shallow incision is placed at the lower end of the papilla in a slightly curved line, perpendicular to the gingival margin (blue line). A second incision is placed, directed to the crestal bone margin from the base of the previously created incision (green line). The result is a split-thickness flap on the base of the papilla.
Incisions
Sulcular incision: The scalpel size has to be small enough to allow free movement of the blade within the sulcus and to avoid cutting into the gingiva (Figs 21.8 and 21.9). The scalpel should be kept in constant contact with the tooth. Even so, the incision will sever sulcular epithelium and fibers of the gingival attachment, leaving epithelium and connective tissue at the root surface (Fig. 21.9). These tissue remnants are delicate and easily injured, which can result in impaired healing (16), and should not be allowed to dry out because they facilitate epithelial and gingival reattachment. Interproximally the tissue should be dissected in the middle of the papilla, to preserve its buccal and lingual aspects (Fig. 21.10).
Fig. 21.6 Curved incision placed perpendicular to the gingival margin (lines). (Reprinted with permission from (60).)

Fig. 21.7 Elevated spit-thickness flap showing the papilla base incision with the major part of the papilla unaltered. (Reprinted with permission from (60).)
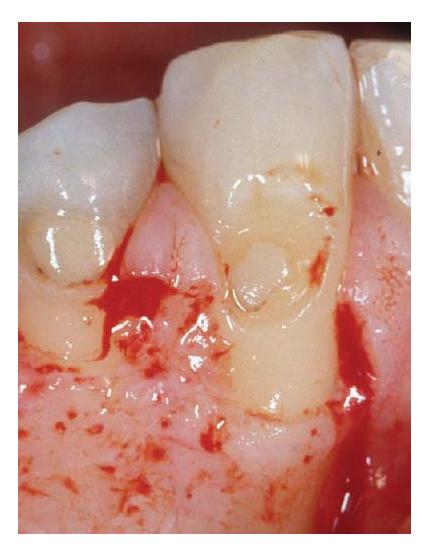
Fig. 21.8 Sulcular incision using a micro-scalpel blade. Note the blade entering the gingival tissue owing to a small root diameter in the cervical area of the root.

Fig. 21.9 Marginal incision leaves small amounts of gingival connective tissue and epithelium on the tooth surface, which should be kept moist and vital for reattachment at the preoperative attachment level.
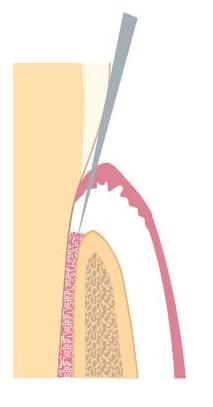
Fig. 21.10 Dissection of the buccal papilla with a micro-scalpel. Note complete separation from the lingual portion of the papilla and the preservation of the tissue in all its dimensions.
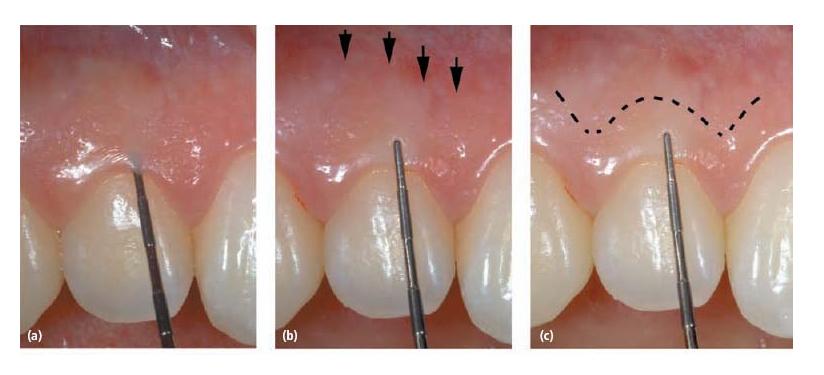
Submarginal incision: The submarginal incision to raise an Ochsenbein–Luebke flap is performed within the attached gingiva and should be at a level where the incision cuts well into the crestal bone (36). The cutting action is a continuous firm stroke with the blade, which separates the tissue all the way to the bone. For easy and precise repositioning of the flap, the incision should not be in a straight line, but scalloped and extending slightly in the interproximal direction. Thus, the contour of the incision should reflect the contour of the marginal gingiva (Fig. 21.11c). The submarginal incision should be at a level that is 2 mm apical to the base of the sulcus in order to avoid the risk of subsequent necrosis and recession of the unreflected marginal portion. To size up the width of the attached gingiva, the pocket probing depth has to be determined (Fig. 21.11a). The width of the attached gingiva is then calculated on the basis of the distance from the base of the sulcus to the linea girlandiformis (Fig. 21.11b).
In general, healing after this mode of incision is favorable because there is sufficient blood supply from vessels exiting at the crestal bone level and from anastomosing vessels deriving from the papilla.
Where there are deep periodontal pockets, this type of incision is contraindicated and a marginal incision should be performed instead. The incision also should not be used when there is danger of having the incision over the bone defect, which increases the risk of postoperative infection. Therefore, the selection of this type of incision requires thorough treatment planning. The main advantage is that the original level of the epithelial attachment can be maintained, which may not always be the case following sulcular incision. This is certainly an important esthetic consideration especially with full crowns, where healing after a sulcular incision can result in gingival recession to such an extent that the crown margins become visible.
Vertical incisions: At least one and usually two vertical incisions are needed in an endodontic surgical procedure to allow sufficient exposure of the root tip area. The incision should extend apically enough to prevent tension on the flap during retraction. When cutting in the apical area the blade often does not reach the bone owing to the thickness of the mucosa, therefore a second stroke has to be taken to completely separate the tissue through the periosteum.
Fig. 21.11 (a) Measuring the pocket probing depth is necessary for calculation of the width of the attached gingiva in a submarginal incision procedure. (b) The probe is held on the buccal surface of the gingiva to visualize the base of the probing depth. The attached gingiva represents the distance from the tip of the probe to the linea girlandiformis (arrows). (c) The line represents the location for a submarginal incision.
The vertical releasing incision is placed usually one tooth laterally to the tooth to be operated on (Fig. 21.3). An exception to this rule is the lower premolar region, where a vertical cut can interfere with the nerve bundles exiting from the mental foramen and cause temporary or permanent paresthesia. In such cases the vertical incision is placed one tooth mesial to the mental foramen. In any case, it is important to determine radiographically the position of the foramen prior to surgery if it is going to be exposed by the flap.
The placement of the vertical incision should be such that the integrity of the papilla is maintained. Figure 21.12 illustrates the correct paramedian releasing incision to be used. Incisions mid-crown and incisions that split the papilla should be avoided because they may lead to necrosis of a large portion of the tissue and recessions.
Flap elevation and retraction
After the incision, lifting the tissue from the underlying bone should raise the flap. In the process, the periosteum should not be perforated or torn. To optimize the healing conditions, maintenance of an intact periosteum is essential because it will protect the surgical cavity from being in direct contact with the mucosal tissue, which otherwise can enter the cavity and prevent complete bone fill.
Flap elevation should begin from the releasing incision in />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses