2
Visualization for Minimally Invasive Periodontal Therapy: An Overview
Stephen K. Harrel
The increasing popularity of minimally invasive procedures has been driven in part by advancements in technology that have allowed procedures to be performed through smaller access openings and by the reduced morbidity and improved efficacy seen as a result of these technologies. The most critical advancements in technology are in the area of visualization. The key to performing minimally invasive procedures is the ability to adequately see the site and, therefore, the ability to successfully complete the indicated surgical manipulations. With enhanced visualization, outcomes are improved.
Traditional closed subgingival scaling and root planing is the most frequently used approach for treating inflammatory periodontal diseases. This approach allows no direct visualization of the treatment site. Treatment end points are based on the tactile sense of the operator using various instruments. The operator is forced to determine by palpation alone if the root surface has been debrided of calculus and if root roughness has been removed. Because of a lack of a tactical “feel,” it is impossible for the operator to determine by palpation if any existing biofilm has been completely removed. The process of determining a clinically ideal end point is complicated by factors such as burnished calculus and various root anomalies that give a less-than-smooth feel to the root. While closed root planing has been shown to routinely improve periodontal health, it has also been shown that the end result is often a root surface with some residual calculus. It was found that root surfaces treated with these traditional methods when subsequently viewed either with the endoscope or the videoscope routinely reveal areas of retained calculus and biofilm. Thus, the lack of visualization in traditional closed approaches frequently results in subsequent periodontal breakdown and frequently leads to further treatment often including surgery.
Traditional periodontal surgery was developed to allow for access and visualization of the surgical site. One of the most commonly performed traditional periodontal surgical procedures is open-flap debridement. This approach allows for visualization of the root surface and periodontal defect. The incisions traditionally used to provide visualization often extend over many teeth and often include areas that have little or no periodontal damage. Elevation of these large flaps frequently leads to post-surgical root exposure, areas of food impaction, and thermal sensitivity as well as esthetic deformities.
Minimally invasive periodontal therapy is designed to access and visualize only the areas that require periodontal treatment using the smallest incision possible. This has been made possible by technologic advances for visualization without the necessity of large incisions and flap elevation. This chapter explores the options currently available for visualization. The advantages and disadvantages of each will be discussed.
Visualization for closed root planing procedures
The very nature of closed root planing demands that visualization of the treatment site uses a visualization technology that can be placed into an intact pocket without a surgical incision. To date, there is a single device, the periodontal endoscope which was developed in the 1990s, that will allow for this approach [1] (Figure 2.1). This endoscope consists of glass fibers contained within a plastic disposable sheath with a small stainless steel tube, and a sealed sapphire lens. The stainless steel tube is retained in a handheld dental instrument that allows the fibers and lens to be directed into the periodontal pocket without flap elevation. Some of the glass fibers direct light into the subgingival environment. Other glass fibers capture an image of this space. The image is returned to an external camera that displays it on a monitor. The operator can directly view the treatment area by looking at the monitor that allows them to determine the need for and efficacy of efforts to remove root-bound deposits.

Figure 2.1 The glass fiber endoscope for use in nonsurgical minimally invasive periodontal therapy is shown.
Source: Courtesy of Dr. John Kwan.
The currently available glass fiber endoscope is less than 1 mm in diameter. It contains several thousand individual optical glass fibers. It is considered flexible because some amount of bending and flexing is possible. However, care must be taken to avoid significant bending of the fibers to reduce the probability of fracture. Typically, even with care, some of the individual glass fibers will break with use. As fractures occur, there will be some degradation of the amount of light that reaches the surgical site, and the image returned to the external camera will be degraded. The image will continue to degrade with use until the endoscope fibers have to be replaced. This degradation and the need for replacement can be a significant factor in the expense of using a periodontal endoscope.
A sheath to cover the glass fibers is necessary because the fibers cannot be sterilized. The sheath comes sterilized and the endoscope is fully contained within the sterile sheath (Figure 2.2). The sheath also acts as a conduit for liquid that flows into the sulcus to keep the treatment site clear of blood and debris. Without a constant flow of liquid, the optics of the endoscope would rapidly become fouled and impossible to use. The surgical sheath is a one-time use item that adds a moderate amount of expense to its use.
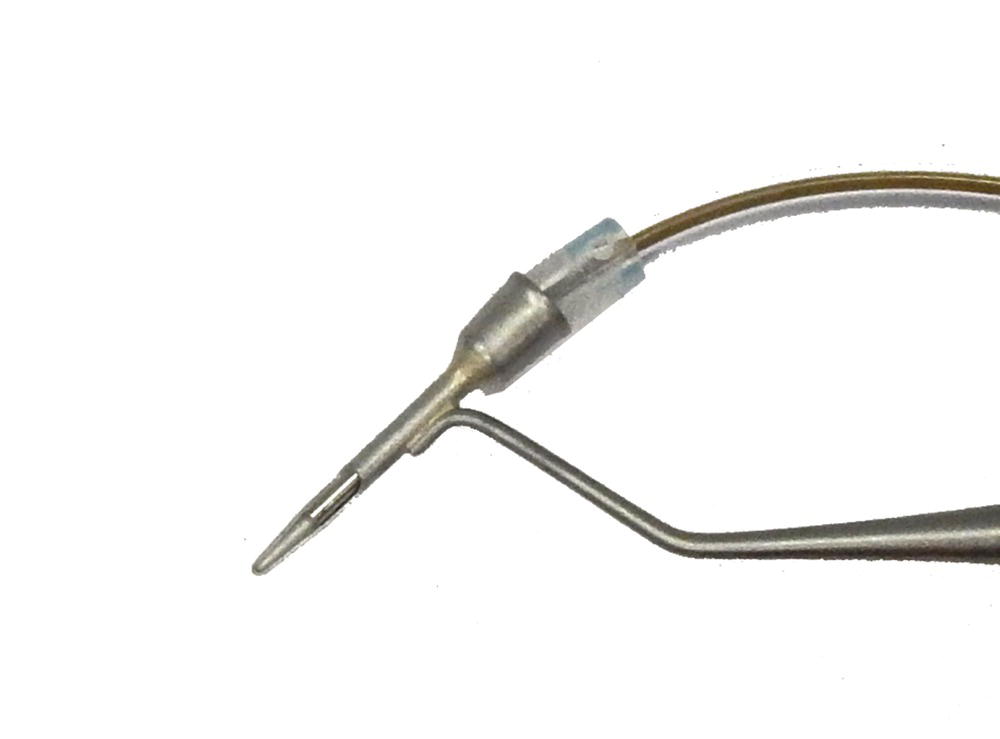
Figure 2.2 The single-use sterile disposable sheath for the glass fiber endoscope is shown.
Source: Courtesy of Dr. John Kwan.
The currently available glass fiber endoscope is the only device that allows visualization of the root surface without the necessity of surgical access. As such, this instrument is unique, and there is no other available alternative for visualization during closed root planing. There are concerns about the endoscope that have limited its acceptance for routine periodontal treatments. Among these is the lack of clarity of the image delivered to the monitor. Most of the lack of clarity is because of the limited number of glass fibers available to transmit the picture. More fibers would increase the diameter of the device and limit its use without flap elevation. Another contributor to the lack of clarity is the amount of debris suspended in the irrigating liquid. The image can be enhanced by moving the instrument over the root surface and causing the debris in the sulcus to be flushed by the flow of irrigant. In addition, the learning curve for this instrument can be quite steep.
Potential improvements for nonsurgical visualization are numerous. The first goal would be to improve the picture quality. This might be accomplished by an increase in the number of optical fibers. This would allow a greater number of fibers to bring light to the sulcus as well as provide more fibers to transmit the />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


