Chapter 2
Preventive and community dentistry
Contents
Relevant pages in other chapters Plaque control, p. 198; prevention of secondary caries, p. 226; prevention of trauma to anterior teeth, p. 95.
Principal sources and further reading British Society for Disability and Oral Health guidelines and policy documents  www.bsdh.org.uk. British Society of Paediatric Dentistry guidelines and policy documents
www.bsdh.org.uk. British Society of Paediatric Dentistry guidelines and policy documents  www.bspd.co.uk. DOH 2007 Delivering Better Oral Health – An evidence-based toolkit for prevention
www.bspd.co.uk. DOH 2007 Delivering Better Oral Health – An evidence-based toolkit for prevention  www.dh.gov.uk. J. J. Murray 2003 Prevention of Oral Disease (4e), OUP. Scottish Intercollegiate Guideline Network (SIGN) guidelines 47 and 83 (preventing dental caries)
www.dh.gov.uk. J. J. Murray 2003 Prevention of Oral Disease (4e), OUP. Scottish Intercollegiate Guideline Network (SIGN) guidelines 47 and 83 (preventing dental caries)  www.sign.ac.uk. R.R. Welbury 2005 Paediatric Dentistry (3e) OUP.
www.sign.ac.uk. R.R. Welbury 2005 Paediatric Dentistry (3e) OUP.
Dental caries
Dental caries (Figure 2.1) is a sugar-dependent infectious disease.1 Acid is produced as a by-product of the metabolism of dietary carbohydrate by plaque bacteria, which results in a drop in pH at the tooth surface. In response, calcium and phosphate ions diffuse out of enamel, resulting in demineralization. This process is reversed when the pH rises again. Caries is therefore a dynamic process characterized by episodic demineralization and remineralization occurring over time. If destruction predominates, disintegration of the mineral component will occur, leading to cavitation.
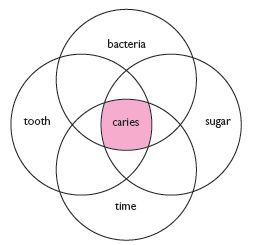
Fig. 2.1 The factors involved in the development of caries.
Enamel caries
The initial lesion is visible as a white spot. This appearance is due to demineralization of the prisms in a sub-surface layer, with the surface enamel remaining more mineralized. With continued acid attack the surface changes from being smooth to rough, and may become stained. As the lesion progresses, pitting and eventually cavitation occur. The carious process favours repair, as remineralized enamel concentrates fluoride and has larger crystals, with a ↓ surface area. Fissure caries often starts as two white spot lesions on opposing walls, which coalesce.
Dentine caries
comprises demineralization followed by bacterial invasion, but differs from enamel caries in the production of secondary dentine and the proximity of the pulp. Once bacteria reach the ADJ, lateral spread occurs, undermining the overlying enamel.
Rate of progression of caries
Although it has been suggested that the mean time that lesions remain confined radiographically to the enamel is 3–4 years,2 there is great individual variation and lesions may even regress.3 The rate of progression through dentine is unknown; however, it is likely to be faster than through enamel. Progression of fissure caries is usually rapid due to the morphology of the area.
Arrested caries
Under favourable conditions a lesion may become inactive and even regress. Clinically, arrested dentine caries has a hard or leathery consistency and is darker in colour than soft, yellow active decay. Arrested enamel caries can be stained dark-brown.
Susceptible sites
The sites on a tooth which are particularly prone to decay are those where plaque accumulation can occur unhindered, e.g. approximal enamel surfaces, cervical margins, and pits and fissures. Host factors, e.g. the volume and composition of the saliva, can also affect susceptibility.
Saliva and caries
Saliva acts as an intra-oral antacid, due to its alkali pH at high flow-rates and buffering capacity. Also:
An appreciation of the importance of saliva can be gained by examining a patient with a dry mouth.
Chewing sugar-free gum regularly after meals does appear to ↓ caries, but the reduction is small.
Root caries
With gingival recession root dentine is exposed to carious attack. Rx requires, first, control of the aetiological factors and for most patients this involves dietary advice and OHI. Topical fluoride may aid remineralization and prevent new lesions developing. However, active lesions will require restoration with GI cement (p. 233).
Caries prevention
Classically three main approaches are possible:
In practice this means dietary advice, fluoride, fissure sealing, and regular toothbrushing (which is also important in the prevention of periodontal disease). The relative value of these varies with the age of the individual.
Of equal importance with the prevention of new lesions is a preventive philosophy on the part of the dentist, so that early carious lesions are given the chance to arrest and a minimalistic approach is taken to the excision of caries where primary prevention has failed.
Caries diagnosis
As caries can be arrested or even reversed, early diagnosis is important.
Aids to diagnosis
Diagnosis and its relevance to management
 Remember: precavitated lesion— prevention
Remember: precavitated lesion— prevention
cavitated lesion— prevention and restoration
 Counsel the patient that if the lesion is not cavitated it has the potential to arrest. This makes the preventive advice very relevant to the patient, increasing the chance of that patient acting on the advice.
Counsel the patient that if the lesion is not cavitated it has the potential to arrest. This makes the preventive advice very relevant to the patient, increasing the chance of that patient acting on the advice.
Smooth surface caries
is relatively straightforward to diagnose. The chances of remineralization are ↑ as it is obvious, and accessible for cleaning. Restoration is indicated if prevention has failed and the lesion is cavitated, or if the tooth is sensitive or aesthetics poor.
Pit and fissure caries
is difficult to diagnose reliably, especially in the early stages. A sharp probe is of limited value as stickiness could be due to the morphology of the fissure. The anatomy of the area also tends to favour spread of the lesion, which often occurs rapidly. As fissure caries is less amenable to fluoride and OH, fissure sealing is preferable to watching and waiting. Occlusal caries evident on b/w radiographs should not always be excised. If the tooth is fissure-sealed or restored, check the margins very carefully, and if intact monitor the lesion radiographically. If marginal integrity not intact, investigate the area with a small round bur. The ‘cavity’ can be aborted if no caries found and the surface sealed.
Approximal caries
Currently accepted practice:
If in doubt whether an approximal lesion has cavitated or not, fit an elastic orthodontic separator for 3–7 days so the surfaces can be visualized.
Recall intervals1
This subject has evoked considerable controversy, some arguing that regular attendance puts a patient more at risk of receiving replacement fillings, while others contend that regular and frequent check-ups are necessary to monitor prevention. In fact, it would appear that only a minority of the British public attend for 6-monthly check-ups. The available evidence suggests that there is no clear benefit for recall intervals of less than 1yr for healthy patients, although the at-risk patient often needs to be seen more frequently.2 In addition, as changing dentist ↑ the likelihood of replacement restorations the profession has to re-examine its criteria for replacement.
In the UK, guidance from the National Institute of Clinical Excellence (NICE) recommends that dental recall intervals (‘oral health review’ intervals) should be determined by the needs of the individual patient based on a risk assessment of existing disease progressing or new disease developing. For adult patients this interval can be between 3 and 24 months and for children 3 and 12 months.1
Fluoride
The history of fluoride is covered well in other texts.1
Mechanisms of the action of fluoride in reducing dental decay
The concentration of fluoride in enamel ↑ with ↑ fluoride content of water supply and ↑ towards the surface of enamel.
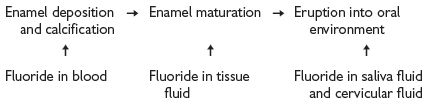
Pre-eruptive effects
Enamel formed in the presence of fluoride has:
Discontinuation of systemic fluoride results in an ↑ in caries, therefore pre-eruptive effects must be limited.
Post-eruptive effects
NB Newly erupted teeth derive the most benefit.
At higher pH fluoride is bound to protein in plaque. A drop in pH results in release of free ionic fluoride, which augments these actions.
NB Fluoride is more effective in ↓ smooth surface than pit and fissure caries.
Safety and toxicity of fluoride
Fluoride is present in all natural waters to some extent. Many simple chemicals are toxic when consumed in excess, and the same is true of fluoride.
Fluoride is absorbed rapidly mainly from the stomach. Peak blood levels occur 1h later. It is excreted via the kidneys, but traces are found in breast milk and saliva. The placenta only allows a small amount of fluoride to cross, therefore pre-natal fluoride is relatively ineffective.
Fluorosis
(or mottling) occurs due to a long-term excessive consumption of fluoride. It is endemic in areas with a high level of fluoride occurring naturally in the water. Clinically, it can vary from faint white opacities to severe pitting and discoloration. Histologically, it is caused by ↑ porosity in the outer third of the enamel.
Toxicity
Safely tolerated dose (STD)
Dose below which symptoms of toxicity are unlikely = 1mg/kg body weight
Potentially lethal dose
(PLD) Lowest dose associated with a fatality. Patient should be hospitalized = 5mg/kg body weight
Certainly lethal dose (CLD)
Survival unlikely = 32–64mg/kg body weight
Fluoride concentration in various products
Standard fluoride toothpastes:
Daily fluoride mouthrinse 0.05% NaF=0.023% F=0.23mg F/ml
APF gel 1.23% F=12.3mg/ml
Fluoride varnish 5% NaF=2.26% F=22.6mg/ml
To reach the 5mg F/kg threshold (requiring hospitalization) a 5yr-old (about 19kg) would have to ingest 95 (1mg F) tablets, 63ml of 1500ppm toothpaste, or 7.6ml of 1.23% of APF gel.
Antidotes:
<5mg F/kg body weight—large volume of milk. >5mg F/kg body weight—refer to hospital quickly for gastric lavage. If any delay give IV calcium gluconate and an emetic.
 Advice about managing fluoride overdose can be sought from the National Poisons Information Service (0870 6006266).
Advice about managing fluoride overdose can be sought from the National Poisons Information Service (0870 6006266).
Health benefits vs risks of fluoride.
A number of detailed systematic reviews have been conducted to investigate the efficacy and safety of fluoride, especially in the context of public water fluoridation schemes1,2,3. These have all essentially come to the same conclusions:
Planning fluoride therapy
Most important action of fluoride is to favour remineralization of the early carious lesion. Although fluoride incorporated within developing enamel results in a high local concentration following acid attack, the maximum benefit appears to be derived from frequent low-concentration topical administration.1
Systemic fluoride
 To minimize the risk of mottling only one systemic measure should be used at a time.
To minimize the risk of mottling only one systemic measure should be used at a time.
Water fluoridation
at 1ppm (1mg F per litre) reduces caries by 50%. Main advantages are systemic and topical effect; no effort is required on the part of the individual; and the low cost. Yet despite this only 10% of the UK population has fluoridated water. In some countries school water has been fluoridated, but a concentration of 5ppm is required to offset the less frequent intake.
Fluoride drops and tablets
Regimen (mg F per day) depends upon drinking water content (see table opposite). This approach can be almost as effective as fluoridated water, but this requires good parental motivation. Unfortunately, compliance is generally poor, so benefit as a public health measure questionable.
Milk
with 2.5–7ppm F has been tried successfully.
Salt
is cheap and effective for rural communities in developing countries where water fluoridation is not feasible.
Topical fluoride
Professionally applied fluorides
Variety of solutions, gels, and application protocols are available. Overall, caries ↓ of 20–40%. If applied in trays without adequate suction the systemic dosage can be high therefore it is better to apply to a few, well-isolated teeth at a time. Fluoride varnish (e.g. Duraphat®) is useful for applying directly to individual lesions to aid arrest, and regular (2-4 times per year) site-specific application has been shown to be effective at ↓ caries incidence in children1. However, it should be applied carefully and sparingly, especially in young children as it contains 23000ppm fluoride.
Rinsing solutions
C/I in children <7yrs. The concentration depends upon the frequency of use: 0.2% fortnightly/weekly or 0.05% daily. Daily use is the most beneficial. Caries reductions of 16–50% have been reported with rinsing alone. The most widely used solution is sodium fluoride.
Toothpastes
aid tooth cleaning, but, most importantly, provide fluoride. In the UK they contain abrasives (to a specified abrasivity standard), detergents, humectants, flavouring, binding agents, preservatives, and active agents, including:
Recommended daily fluoride supplementation (mg F) 1,2,3
For children considered to be at high risk of caries and who live in areas with water supplies containing less than 0.3ppm:
| Age | mg F per day |
| 6 months to 3yrs | 0.25 |
| 3yrs to 6yrs | 0.5 |
| >6yrs | 1.0 |
Toothpaste
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


