CHAPTER 2. Disorders of development of the teeth and related tissues
Box 2.1
Requirements for development of an ideal dentition
• Formation of a full complement of teeth
• Normal structural development of the dental tissues
• Eruption of each group of teeth at the appropriate time into an adequate space
• Normal development of jaw size and relationship
• Eruption of teeth into correct relationship to occlude with their opposite numbers
Significant structural defects of teeth are uncommon, but disorders of occlusion due to irregularities of the teeth in the arch or abnormal relationship of the arches to each other are so common that their treatment has become a specialty in its own right. The main groups of disorders affecting development of the dentition are summarised in Box 2.2 and Summary chart 2.1 and Summary chart 2.2.
Box 2.2
Disorders of development of teeth
• Abnormalities in number
Anodontia or hypodontia
Additional teeth (hyperdontia)
• Disorders of eruption
• Defects of structure
Enamel defects
Dentine defects
• Developmental anomalies of several dental tissues
Odontomas
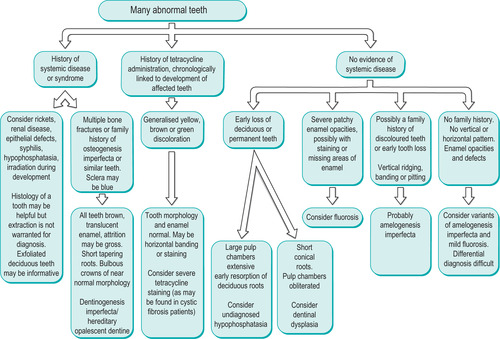 |
| Summary chart 2.1
Differential diagnosis of developmental defects of the teeth.
|
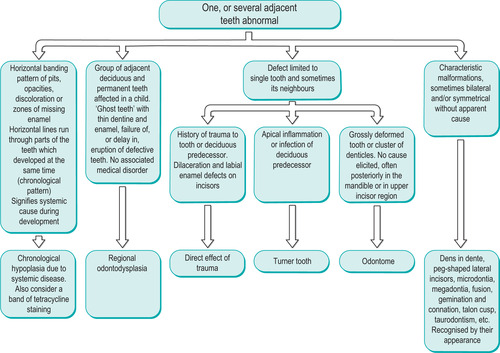 |
| Summary chart 2.2
Differential diagnosis of developmental and acquired abnormalities of one or a group of teeth.
|
ABNORMALITIES IN THE NUMBER OF TEETH
Isolated hypodontia or anodontia
Failure of development of one or two teeth is relatively common and often hereditary. The teeth most frequently missing are third molars, second premolars or maxillary second incisors (Fig. 2.1). Absence of third molars can be a disadvantage if first or second molars, or both, have been lost. The absence of lower premolars worsens malocclusion if there is already disparity between an underdeveloped mandible and a normal upper arch. Otherwise, absence of these teeth may have little or no noticeable effect.
 |
| Fig. 2.1
Congenital absence of lateral incisors with spacing of the anterior teeth.
|
Absence of lateral incisors can sometimes be conspicuous because the large, pointed canines erupt in the front of the mouth beside the central incisors. It is usually impossible to prevent the canine from erupting into this empty space, even if the patient is seen early. It is also very difficult to make room between the centrals and canines by orthodontic means to replace the laterals. An attempt has often therefore to be made to disguise the shape of the canines.
Total failure of development of a complete dentition (anodontia) is exceedingly rare. If the permanent dentition fails to form, the deciduous dentition is retained for many years but, when these deciduous teeth become excessively worn or too much damaged by caries, then they must be replaced by dentures or implants.
Hypodontia or anodontia with systemic defects
Anhidrotic (hereditary) ectodermal dysplasia
The main features are summarised in Box 2.3. In severe cases no teeth form. More often, most of the deciduous teeth form, but there are few or no permanent teeth. The teeth are usually peg-shaped or conical (Fig. 2.2).
 |
| Fig. 2.2
Anhidrotic ectodermal dysplasia showing conical teeth, giving an undesirable, Dracula-like appearance.
|
Box 2.3
Anhidrotic ectodermal dyplasia: major features
• Usually a sex-linked recessive trait
• Hypodontia
• Hypotrichosis (scanty hair)
• Anhidrosis (inability to sweat)
When there is anodontia, the alveolar process, without teeth to support, fails to develop and has too little bone to support implants. The profile then resembles that of an elderly person because of the gross loss of vertical dimension. The hair is fine and sparse (Fig. 2.3), particularly in the tonsural region. The skin is smooth, shiny and dry due to absence of sweat glands. Heat is therefore poorly tolerated. The finger nails are usually also defective. All that can be done to improve the patient’s appearance and mastication is to fit dentures, which are usually well tolerated by children.
 |
| Fig. 2.3
Another case showing typical fine and scanty hair and loss of support for the facial soft tissues.
|
Other conditions associated with hypodontia
There are many rare syndromes where hypodontia is a feature, but the only common one is Down’s syndrome (Ch. 33). One or more third molars are absent in over 90% of these patients, while absence of individual teeth scattered about the arch is also common. Anodontia is rare. Palatal clefts may be associated, though this is also rare.
Additional teeth: hyperdontia
Additional teeth are relatively common. They are usually of simple conical shape (supernumerary teeth) but, less frequently, resemble teeth of the normal series (supplemental teeth). These are the results of excessive but organised growth of the dental lamina of unknown cause.
Supernumerary teeth → Summary p. 157. Conical or more seriously malformed additional teeth most frequently form in the incisor or molar region (Fig. 2.4) and very occasionally, in the midline (mesiodens, Fig. 2.5).
 |
| Fig. 2.4
A paramolar, a buccally placed supernumerary molar tooth.
|
Supplemental teeth. Occasionally an additional maxillary incisor, premolar or, rarely, a fourth molar develops (also seen in Fig. 2.5).
 |
| Fig. 2.5
Maleruption of a midline tuberculate supernumerary and two supplemental premolars.
|
Effects and treatment
Additional teeth usually erupt in abnormal positions, labial or buccal to the arch, creating stagnation areas and greater susceptibility to caries, gingivitis and periodontitis. Alternatively, a supernumerary tooth may prevent a normal tooth from erupting. These additional teeth should usually be extracted.
Syndromes associated with hyperdontia
These syndromes are all rare but probably the best known is cleidocranial dysplasia (Ch. 10) where many additional teeth develop but fail to erupt.
DISORDERS OF ERUPTION
Eighteenth-century parish registers are replete with the names of infants who had died as a result of teething. Nevertheless, the idea that teething, the normal eruption of infants’ teeth, can cause systemic symptoms or serious illness is of course a myth. The time of teething coincides with a period of naturally low resistance to infection and declining maternal passive immunity so that infection during the period of teething is merely coincidental. As might be expected, several studies have shown that teething does not cause systemic disorders. Nevertheless, so resistant is this traditional belief to rational explanation, that yet another study was carried out in 2000, confirming yet again that teething was harmless.
However, an ingenious neuropathologist has suggested that the minute wounds left by the shedding of deciduous teeth could provide a means of entry for the BSE (‘mad cow disease’) prion to cause variant CJD. In view of an incubation period of many years, this suggestion is consistent with the onset of the disease in adolescence. However, this theory is as yet unproven.
Eruption of deciduous teeth starts at about 6 months, usually with the appearance of the lower incisors, and is complete by about 2 years. Mass failure of eruption is very rare. More often eruption of a single tooth is prevented by local obstruction. In the permanent dentition, delay in eruption of a tooth or, more frequently, too early loss of a deciduous predecessor tends to cause irregularities because movement of adjacent teeth closes the available space.
Delayed eruption associated with skeletal disorders
Metabolic diseases, particularly cretinism and rickets, are now uncommon causes of delayed eruption of teeth. Cleidocranial dysplasia, in which there are typically many additional teeth but failure of most of them to erupt, has been mentioned earlier. In severe hereditary gingival fibromatosis, eruption may apparently fail merely because the teeth are buried in the excessive fibrous gingival tissue and only their tips show in the mouth (pseudoanodontia). In cherubism (Ch. 10), several teeth may be displaced by the proliferating connective tissue masses containing giant cells and are prevented from erupting.
Local factors affecting eruption of deciduous teeth
Having no predecessors, deciduous teeth usually erupt unobstructed. Occasionally, an eruption cyst may overlie a tooth but is unlikely to block eruption.
Local factors affecting eruption of permanent teeth
A permanent tooth may be prevented from erupting or misplaced by various causes (Box 2.4).
Box 2.4
Local causes of failure of eruption of permanent teeth
• Loss of space, crowding
• Abnormal position of the crypt
• Supernumerary and supplemental teeth
• Displacement in a dentigerous cyst or by other lesion
• Retention of a deciduous predecessor
Treatment depends on the circumstances, but room may be made for the unerupted tooth by orthodontic means or extractions. A retained deciduous tooth should be extracted if radiographs show a normal permanent successor. If a buried tooth partially erupts and becomes infected, it may have to be removed – mandibular third molars are the main source of this complication.
Changes affecting buried teeth
Teeth may occasionally remain buried in the jaws for many years without complications. The roots of these teeth may undergo varying degrees of hypercementosis or resorption. Alternatively, the teeth may become enveloped in dentigerous cysts, as in cleidocranial dysplasia for example.
DEFECTS OF STRUCTURE: HYPOPLASIA AND HYPOCALCIFICATION
Minor structural defects of the teeth, such as pitting or discoloration or, occasionally, more serious defects, may be markers of past disease, but only rarely is the disease still active. Hypoplasia of the teeth is not an important contributory cause of dental caries; indeed, hypoplasia due to fluorosis is associated with enhanced resistance. The main clinical requirement is usually cosmetic improvement.
Defects of deciduous teeth
Calcification of deciduous teeth begins about the fourth month of intrauterine life. Disturbances of metabolism or infections that affect the fetus at this early stage without causing abortion are rare. Defective structure of the deciduous teeth is therefore uncommon but, in a few places, such as parts of India, where the fluoride content of the water is excessively high, the deciduous teeth may be mottled.
The deciduous teeth may be discoloured by abnormal pigments circulating in the blood. Severe neonatal jaundice may cause the teeth to become yellow, or there may be bands of greenish discoloration. In congenital porphyria, a rare disorder of haemoglobin metabolism, the teeth are red or purple. Tetracycline given during dental development is the main cause of permanent discoloration.
Defects of permanent teeth
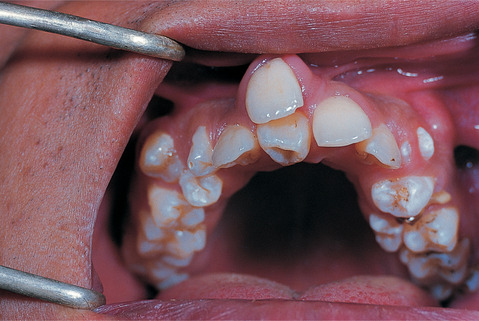
Single permanent teeth may be malformed as a result of local causes such as periapical infection of a predecessor (Turner teeth –Fig. 2.6), damage, for instance by intubation while a preterm neonate (Fig. 2.7) or multiple teeth by systemic diseases as summarised in Box 2.5.
 |
| Fig. 2.6
Turner tooth, a hypoplastic tooth resulting from periapical infection, usually of the deciduous predecessor.
|
 |
| Fig. 2.7
Localised dental disturbance caused by prolonged intubation during tooth development. The upper left central incisor shows enamel pitting incisally and the upper right central incisor is deformed and has failed to erupt.
|
Box 2.5
Multiple malformed permanent teeth: important causes
Genetic
• Amelogenesis imperfecta
Hypoplastic (type 1)
Hypomaturation (type 2)
Hypocalcified (type 3)
• Dentinogenesis imperfecta
Shell teeth
• Dentinal dysplasia
• Regional odontodysplasia
• Multisystem disorders with associated dental defects
• Hypophosphatasia
Infective
• Congenital syphilis
Metabolic
• Childhood infections, rickets, hypoparathyroidism
Drugs
• Tetracycline pigmentation
• Cytotoxic chemotherapy
Fluorosis
Other acquired developmental anomalies
• Fetal alcohol syndrome
Amelogenesis imperfecta → Summary p. 21
Amelogenesis imperfecta is a group of conditions caused by defects in the genes encoding enamel matrix proteins. Classification is complex and based on pattern of inheritance, enamel hypoplasia, hypomineralisation or hypomaturation and appearance; smooth, rough or pitted. At least 16 forms are recognised on clinical grounds but some are accounted for by differing severity and the classification is contentious.
Inheritance can be autosomal dominant, recessive or X-linked. However, the most common types have an autosomal inheritance and are thought to be caused by mutations in the AMEL X gene, which codes for ameloblastin (C4), enamelin (C4) or tuftelin (C1). In the case of the autosomal dominant type of amelogenesis imperfecta, the locus of the defective gene is on chromosome 4q21 to which enamelin maps.
The less common X-linked types are caused by a variety of defects in the amelogenin genes and, confusingly, it seems the same mutation can sometimes cause hypoplasia, hypomineralisation or hypomaturation in different patients.
Genetic factors act throughout the whole duration of amelogenesis. Characteristically therefore, all teeth are affected and defects involve the whole, or are randomly distributed in the enamel. By contrast, exogenous factors affecting enamel formation (with the important exception of fluorosis) tend to act for a relatively brief period and produce defects related to that period of enamel formation.
Hypoplastic amelogenesis imperfecta
The main defect is inadequate formation of the matrix. The enamel is randomly pitted, grooved or very thin, but hard and translucent (Fig. 2.8). The defects tend to become stained, but the teeth are not especially susceptible to caries unless the enamel is scanty and easily damaged.
 |
| Fig. 2.8
Amelogenesis imperfecta, hypoplastic pitted type. Enamel between pits appears normal.
|
The main patterns of inheritance are autosomal dominant and recessive, X-linked and (a genetic rarity) an X-linked dominant type. In the last, there is almost complete failure of enamel formation in affected males, while in females the enamel is vertically ridged (Fig. 2.9, Fig. 2.10 and Fig. 2.11). Occasionally, cases are difficult to classify (Fig. 2.12).
 |
| Fig. 2.9
Close-up of X-linked dominant hypoplastic type amelogenesis imperfecta. These teeth, from an affected female, show the typical vertical ridged pattern of normal and abnormal enamel as a result of Lyonisation.
|
 |
| Fig. 2.10
Amelogenesis imperfecta X-linked dominant hypoplastic form in a male. This premolar has a cap of enamel so thin that the shape of the tooth is virtually that of the dentine core.
|
 |
| Fig. 2.11
Amelogenesis imperfecta X-linked dominant hypoplastic type in a male showing a thin translucent layer of defective enamel on the dentine surface.
|
 |
| Fig. 2.12
Amelogenesis imperfecta, indeterminate type. Some cases, such as this, are difficult to classify but are clearly inherited, as shown by their long family history.
|
Hypomaturation amelogenesis imperfecta
The enamel is normal in form on eruption but opaque, white to brownish-yellow. The teeth appear similar to mottled fluoride effects (Figs 2.13 and 2.14). However, they are soft and vulnerable to attrition, though not as severely as the hypocalcified type.
 |
| Fig. 2.13
Amelogenesis imperfecta, hypomaturation type. Tooth morphology is normal but there are opaque white and discoloured patches.
|
 |
| Fig. 2.14
Amelogenesis imperfecta, one of the several hypomaturation types. In this form there are opaque white flecks and patches affecting the occlusal half of the tooth surface.
|
Hypocalcified amelogenesis imperfecta
Enamel matrix is formed in normal quantity but poorly calcified. When newly erupted, the enamel is normal in thickness and form, but weak and opaque or chalky in appearance.
The teeth tend to become stained and relatively rapidly worn away. The upper incisors may acquire a shouldered form due to the chipping away of the thin, soft enamel of the incisal edge (Fig. 2.15). There are dominant and recessive patterns of inheritance.
 |
| Fig. 2.15
Amelogenesis imperfecta, hypocalcified type. The soft chalky enamel was virtually of normal thickness and form but has chipped away during mastication leaving a characteristic shoulder, seen best on the upper left central incisor.
|
Dentinogenesis (odontogenesis) imperfecta → Summary p. 21
This uncommon defect of collagen formation is transmitted as an autosomal dominant trait. The gene is closely related to that of osteogenesis imperfecta (Ch. 10) particularly type IV. Defects in the genes COL1A1 and COL1A2, for the procollagen alpha helix, prevent polymerisation into normal type 1 collagen.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


