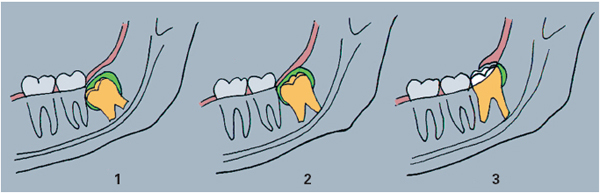
Anomalies of dentition are caused by retained teeth. This term includes impacted and partially erupted teeth and applies to any tooth that is not in its correct functional position after its normal eruption time, taking into account the age of the patient (Fig 2-1).
• A retained tooth is considered to be impacted if the pericoronal follicle does not connect with the oral cavity.
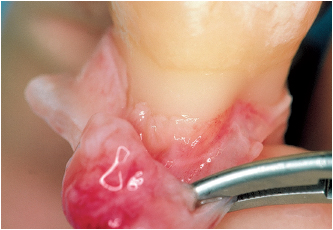
• A retained tooth is considered to have partially erupted if the follicle membrane opens partially or totally into the oral cavity (Figs 2-2a and 2-2b).
Thus, an impacted tooth may either still be totally enclosed inside its bone crypt or the roof of the bone crypt may already be perforated. The crown and its follicular membrane then come into contact with the inner aspect of the fibromucosa, which completely covers the cortical bone; at this stage of eruption the tooth is in a submucosal position. The tooth, however, remains impacted as long as its follicular membrane is not perforated.
The emergence of the tooth occurs when the reduced epithelium and the gingival epithelium fuse together; the crown then breaks through this epithelial layer to erupt into the oral cavity. If emergence cannot occur normally and the crown is retained, the tooth is considered to be submerged or partially retained rather than partially impacted.
The precision of these definitions is important because it enables a distinction to be made between the two types of pathology:
• A follicular cyst (dentigerous cyst) appears when the tooth bud is dystopic or indeed ectopic and the eruption of the tooth is obstructed. The bone crypt is distorted and its walls are pushed back due to the thickening of the follicular tissue.
• Conversely, pericoronitis occurs after the emergence of the tooth, when the pericoronal space opens up into the oral cavity.
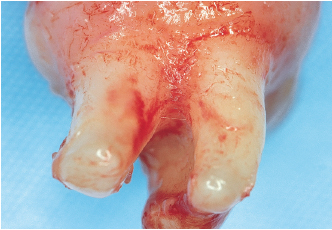
The apex of the dental follicle produces the tissues that support the tooth: the cementum, the periodontal ligament, and the alveolar bone wall (Cahill and Marks). This means that part of the dental follicle disappears as root formation occurs. On the other hand, the coronal portion of the follicle remains until the tooth emerges. At this stage, osteoclasts form to ensure sufficient bone resorption for the tooth to erupt (Marks and Cahill). This occluded portion of the follicle, which completely surrounds the crown, is in close contact with the reduced epithelium. Note that the follicular tissue is not inserted into the anatomic collar, but remains attached to the roots away from the enamel (Figs 2-3 to 2-6). The supracrestal ligament, which develops only after the tooth has emerged, is then inserted into the exposed root area (Korbendau and Guyomard).
The development of a cyst or tumor in the follicle occurs when the tooth is retained. This type of odontogenic cyst occurs quite frequently. About 50% of such cysts are associated with the mandibular third molars. Like the maxillary canine or the mandibular premolars, the eruption of a mandibular third molar is often impeded by a lack of space in the dental arch (Korbendau and Guyomard). The pathogenesis of the development of this type of cyst is still unknown, although the buildup of cystic fluid between the enamel and the follicular tissue is a characteristic of cyst development.
The presence of a follicular cyst in its latent phase cannot be detected by clinical examination because the lesions are generally asymptomatic. Lesions may be discovered in the second decade of life, in the mixed-dentition adolescent, or in the young adult, sometimes following inflammatory events, but are most often detected during routine radiographic examinations:
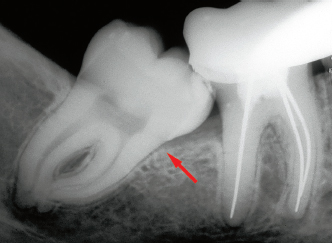
• Small-sized cysts accompany the teeth, which are impacted in the retromolar triangle area (Fig 2-7).
• Voluminous cysts develop in the follicle of the ectopic teeth, which are generally distal to the dental arch (Main) (Figs 2-8a and 2-8b).

2-4 The occlusal end of the follicle completely surrounds the crown. Cell degeneration and thickening of this wall lead to osteolysis and to the enlargement of the bone crypt in the case of cyst formation.
2-5 The follicular membrane has been pushed back, possibly beyond the boundary of the enamel.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses