2 Developmental and Congenital Conditions
Diffuse White Lesions
White Sponge Nevus (Cannon White Sponge Nevus)
Clinical Findings
Etiopathogenesis and Histopathologic Features
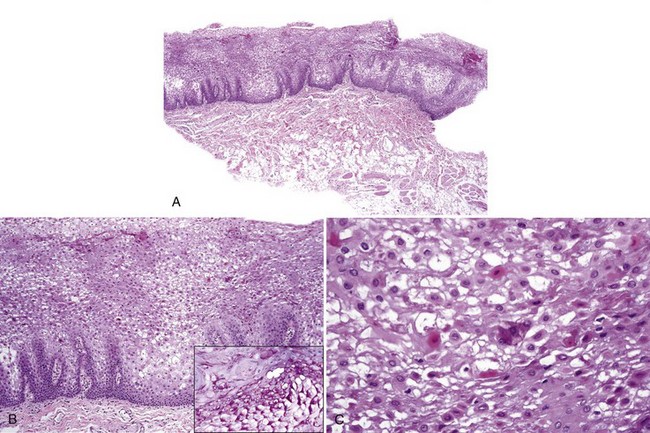
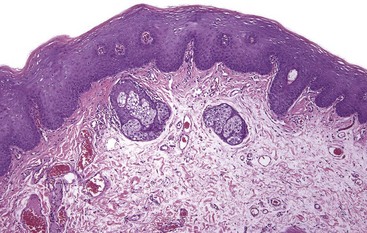
• Variable parakeratosis, benign epithelial hyperplasia with “spongy appearance” caused by cytoplasmic vacuolation (from glycogen) and not true spongiosis; minimal to no inflammation (Fig. 2-2, A and B)
• Perinuclear eosinophilic condensations of keratin and dyskeratotic cells sine qua non for diagnosis (see Fig. 2-2, C); rare cases with epidermolytic hyperkeratosis
Aloi FG, Molinero A. White sponge nevus with epidermolytic changes. Dermatologica. 1988;177:323-326.
Atkinson JC, Harvey KE, Domingo DL, et al. Oral and dental phenotype of dyskeratosis congenita. Oral Dis. 2008;14:419-427.
Boralevi F, Haftek M, Vabres P, et al. Hereditary mucoepithelial dysplasia: clinical, ultrastructural and genetic study of eight patients and literature review. Br J Dermatol. 2005;153:310-318.
Lourenco SV, Boggio PA, Fezzi FA, et al. Dyskeratosis congenita—report of a case with emphasis on gingival aspects. Pediatr Dermatol. 2009;26:176-179.
Morris R, Gansler TS, Rudisil MT, Neville B. White sponge nevus. Diagnosis by light microscopic and ultrastructural cytology. Acta Cytologica. 1988;32:357-361.
Otobe IF, de Sousa SO, Matthews RW, Migliari DA. White sponge naevus: improvement with tetracycline mouth rinse: report of four cases. Clin Exp Dermatol. 2007;32:749-751.
Pradeep AR, Nagaraja C. Pachyonychia congenita with unusual dental findings: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:89-93.
Rugg EL, McLean WH, Allison WE, et al. A mutation in the mucosal keratin K4 is associated with oral white sponge nevus. Nat Genetics. 1995;11:450-452.
Terrinoni A, Candi E, Oddi S, et al. A glutamine insertion in the 1A alpha helical domain of the keratin 4 gene in a familial case of white sponge nevus. J Invest Dermatol. 2000;114:388-391.
Treister N, Lehmann LE, Cherrick I, et al. Dyskeratosis congenita vs. chronic graft versus host disease: report of a case and a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:566-571.
Witkop CJJr, White JG, King RA, et al. Hereditary mucoepithelial dysplasia: a disease apparently of desmosome and gap junction formation. Am J Hum Genet. 1979;31:414-427.
Hereditary Benign Intraepithelial Dyskeratosis
Clinical Findings
• Associated with Haliwa Indians in North Carolina and their descendants (usually on East Coast of the United States); diagnosed in first 2 decades of life
• Oral mucosa with thickened painless, diffuse, folded spongy white plaques similar to white sponge nevus
• Eye lesions present as gelatinous plaques on bulbar conjunctiva in perilimbic location
Etiopathogenesis and Histopathologic Features
Allingham RR, Seo B, Rampersaud E, et al. Duplication in chromosome 4q35 is associated with hereditary benign intraepithelial dyskeratosis. Am J Hum Genet. 2001;68:491-494.
Cummings TJ, Dodd LG, Eedes CR, Klintworth GK. Hereditary benign intraepithelial dyskeratosis: an evaluation of diagnostic cytology. Arch Pathol Lab Med. 2008;132:1325-1328.
Haisley-Royster CA, Allingham RR, Klintworth GK, Prose NS. Hereditary benign intraepithelial dyskeratosis: report of two cases with prominent oral lesions. J Am Acad Dermatol. 2001;45:634-636.
Jham BC, Mesquita RA, Aguiar MC, Carmo MA. Hereditary benign intraepithelial dyskeratosis: a new case? J Oral Pathol Med. 2007;36:55-57.
Darier Disease (Keratosis Follicularis) and Warty Dyskeratoma
Clinical Findings
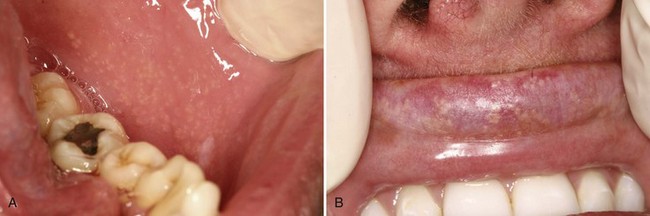
• Darier disease characterized by white, painless, keratotic papules (seen in mild disease) or plaques and cobblestoning of the mucosa (seen in more severe disease) in 10% to 50% of patients with skin disease (Fig. 2-4); onset in first and second decade; lesions on palate, gingiva or tongue; skin findings invariably present; up to one third of cases with parotid or submandibular swelling likely because of strictures and obstruction
• Warty dyskeratoma: isolated white, warty papule usually of the palate or gingiva
Etiopathogenesis and Histopathologic Features
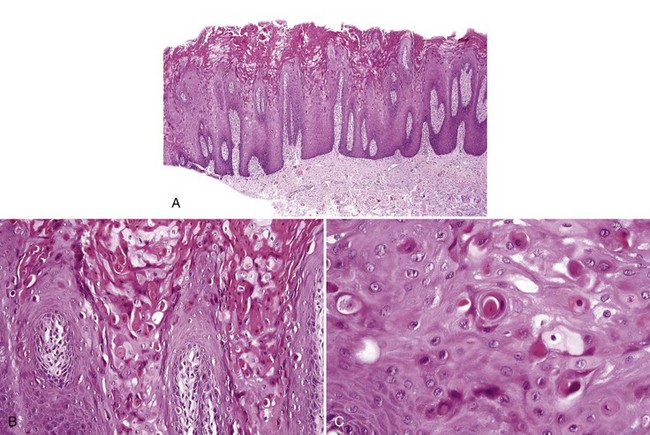
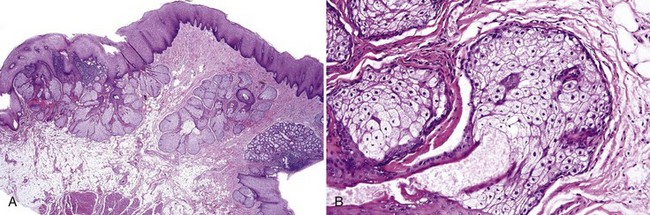
• Often umbilicated/crateriform hyperkeratosis, elongated, slender rete ridges 3 to 8 cells wide, and suprabasilar acantholysis with villous-like projections of connective tissue papillae rimmed by basal cells; dyskeratotic cells with dark nuclei in the form of slender grains (needle-shaped) or corps ronds (round) may not be prominent; variable chronic inflammation (Fig. 2-5)
Adams AM, Macleod RI, Munro CS. Symptomatic and asymptomatic salivary duct abnormalities in Darier’s disease: a sialographic study. Dentomaxillofac Radiol. 1994;23:25-28.
Burge SM, Wilkinson JD. Darier-White disease: a review of the clinical features in 163 patients. J Am Acad Dermatol. 1992;27:40-50.
Frezzini C, Cedro M, Leao JC, Porter S. Darier disease affecting the gingival and oral mucosal surfaces. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:e29-33.
Macleod RI, Munro CS. The incidence and distribution of oral lesions in patients with Darier’s disease. Br Dent J. 1991;171:133-136.
Sakuntabhai A, Ruiz-Perez V, Carter S, et al. Mutations in ATP2A2, encoding a Ca2+ pump, cause Darier disease. Nat Genet. 1999;21:271-277.
Zunt SL, Tomich CE. Oral focal acantholytic dyskeratosis. J Dermatol Surg Oncol. 1990;16:510-515.
Nodular or Tumor-Like Lesions
Fordyce Granules, Sebaceous Hyperplasia, and Adenoma
Clinical Findings
• Fordyce granules: 1 to 3 mm yellowish papules or macules on the posterior buccal mucosa, vermilion of lips, usually bilateral and symmetric, present in 80% of population (Fig. 2-6)
• Sebaceous hyperplasia and adenoma: larger yellowish papules and nodules at same sites as Fordyce granules
• Sebaceous choristoma: usually midline of tongue in area of foramen cecum
Etiopathogenesis and Histopathologic Features
Fordyce granules are considered normal and these can become hyperplastic and adenomatous.
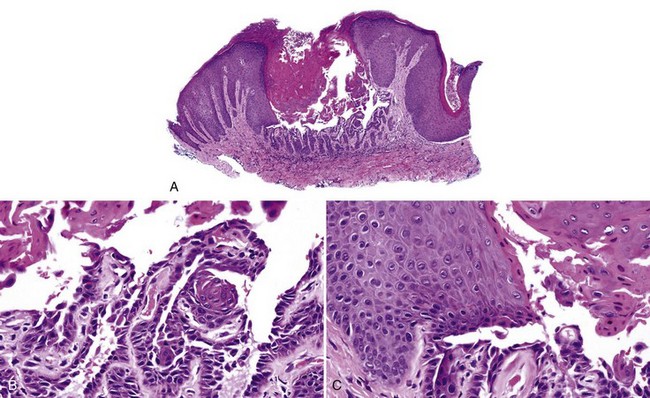
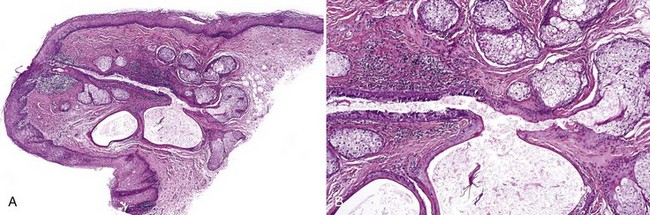
• Fordyce granules: mature sebaceous glands open onto the mucosa via duct; sebocytes have central nuclei and vacuolated cytoplasm; hair and Demodex folliculorum have been reported (Fig. 2-7).
• Hyperplasia: at least 15 lobules (this number is somewhat arbitrary); ducts lined by low cuboidal to columnar epithelium (Figs. 2-8 and 2-9).
• Adenoma: proliferation of germinative cells at the periphery of the lobules
Azevedo RS, Almeida OP, Netto JN, et al. Comparative clinicopathological study of intraoral sebaceous hyperplasia and sebaceous adenoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:100-104.
Daley TD. Intraoral sebaceous hyperplasia. Diagnostic criteria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1993;75:343-347.
Franklin CD, Underwood JC. Demodex infestation of oral mucosal sebaceous glands. Oral Surg Oral Med Oral Pathol. 1986;61:80-82.
Izutsu T, Kumamoto H, Kimizuka S, Ooya K. Sebaceous adenoma in the retromolar region: report of a case with a review of the English literature. Int J Oral Maxillofac Surg. 2003;32:423-426.
Kaminagakura E, Andrade CR, Rangel AL, et al. Sebaceous adenoma of oral cavity: report of case and comparative proliferation study with sebaceous gland hyperplasia and Fordyce’s granules. Oral Dis. 2003;9:323-327.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses