APPROPRIATE ORAL HEALTH CARE
TREATMENT PLANNING
Preoperative assessment
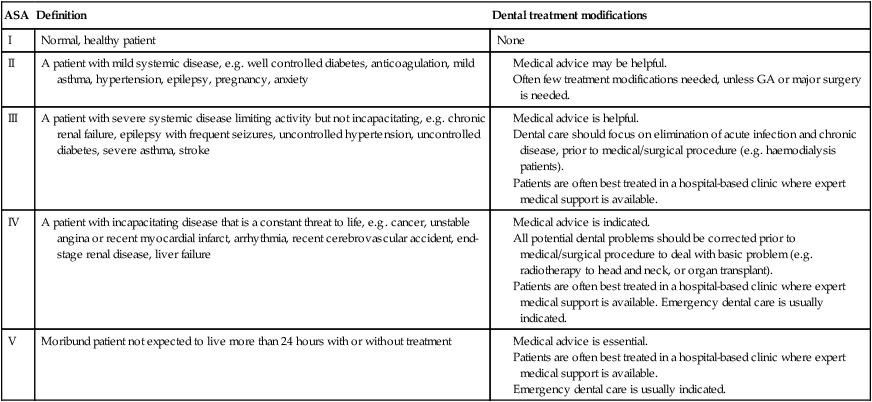
An arbitrary guideline to assist in the selection of appropriate treatment modalities for a patient may be based on the Classification of Physical Status of the American Society of Anesthesiology (ASA) (Table 2.1).
Table 2.1
Classification of Physical Status of the American Society of Anesthesiology (ASA)
| ASA | Definition | Dental treatment modifications |
| I | Normal, healthy patient | None |
| II | A patient with mild systemic disease, e.g. well controlled diabetes, anticoagulation, mild asthma, hypertension, epilepsy, pregnancy, anxiety |
All potential dental problems should be corrected prior to medical/surgical procedure to deal with basic problem (e.g. radiotherapy to head and neck, or organ transplant).
Patients are often best treated in a hospital-based clinic where expert medical support is available. Emergency dental care is usually indicated.
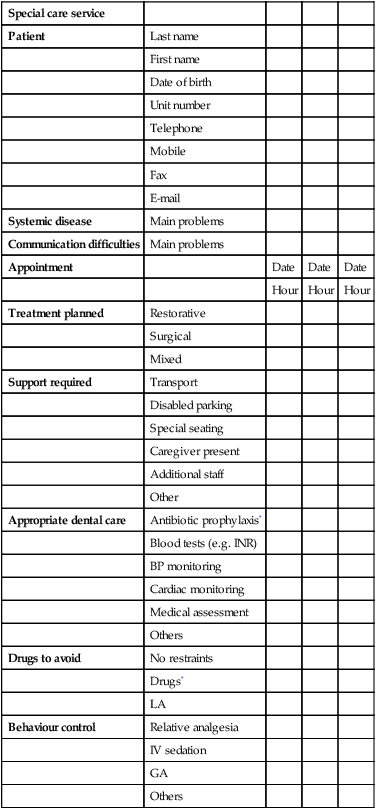
Preoperative planning
Good preoperative assessment and organisation will assist in anticipating potential hazards when providing oral care, and also help to ensure measures are in place to manage emergencies quickly and efficiently. In most situations dentistry is safe, provided that the patient is healthy and the procedure is not dramatically invasive. Risks arise when these conditions do not apply and the dental team attempts anything over-ambitious in terms of their skill, knowledge or available facilities. It is helpful to formulate a checklist to ensure that factors such as transport, disabled parking and the need for accompanying carers are considered prior to the first treatment appointment. It may also be of benefit to devise a treatment plan consisting of a preoperative, operative and postoperative phase, to ensure that other factors (such as the provision of preoperative antibiotics for the prophylaxis of infective endocarditis) are also considered (Table 2.2).
Table 2.2
Example of clinic appointment schedule
| Special care service | ||||
| Patient | Last name | |||
| First name | ||||
| Date of birth | ||||
| Unit number | ||||
| Telephone | ||||
| Mobile | ||||
| Fax | ||||
| Systemic disease | Main problems | |||
| Communication difficulties | Main problems | |||
| Appointment | Date | Date | Date | |
| Hour | Hour | Hour | ||
| Treatment planned | Restorative | |||
| Surgical | ||||
| Mixed | ||||
| Support required | Transport | |||
| Disabled parking | ||||
| Special seating | ||||
| Caregiver present | ||||
| Additional staff | ||||
| Other | ||||
| Appropriate dental care | Antibiotic prophylaxis* | |||
| Blood tests (e.g. INR) | ||||
| BP monitoring | ||||
| Cardiac monitoring | ||||
| Medical assessment | ||||
| Others | ||||
| Drugs to avoid | No restraints | |||
| Drugs* | ||||
| LA | ||||
| Behaviour control | Relative analgesia | |||
| IV sedation | ||||
| GA | ||||
| Others |
CONSENT
 Before you examine, treat or care for competent adult patients you must obtain their consent.
Before you examine, treat or care for competent adult patients you must obtain their consent.
 Adults are always assumed to be competent unless demonstrated otherwise. If you have doubts about their competence, the question to ask is: ‘can this patient understand and weigh up the information needed to make this decision?’ Unexpected decisions do not prove the patient is incompetent, but may indicate a need for further information or explanation.
Adults are always assumed to be competent unless demonstrated otherwise. If you have doubts about their competence, the question to ask is: ‘can this patient understand and weigh up the information needed to make this decision?’ Unexpected decisions do not prove the patient is incompetent, but may indicate a need for further information or explanation.
 Patients may be competent to make some health care decisions, even if they are not competent to make others.
Patients may be competent to make some health care decisions, even if they are not competent to make others.
 Giving and obtaining consent is usually a process, not a one-off event. Patients can change their minds and withdraw consent at any time.
Giving and obtaining consent is usually a process, not a one-off event. Patients can change their minds and withdraw consent at any time.
 The nature, purpose, benefits and risks of the treatment.
The nature, purpose, benefits and risks of the treatment.
 Alternative treatments and their relative benefits and risks.
Alternative treatments and their relative benefits and risks.
In the UK, competent adults, namely a person aged 18 and over who has the capacity to make />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Lack of perceived need
Lack of perceived need  Anxiety or fear, which may be heightened by previous dental or medical encounters
Anxiety or fear, which may be heightened by previous dental or medical encounters  Financial considerations
Financial considerations  Lack of access (e.g.
Lack of access (e.g. 
 Inappropriate manpower resources
Inappropriate manpower resources  Uneven geographical distribution
Uneven geographical distribution  Training inappropriate to changing needs and demands
Training inappropriate to changing needs and demands  Insufficient sensitivity to patient attitudes and needs.
Insufficient sensitivity to patient attitudes and needs. Insufficient public support of attitudes conducive to health
Insufficient public support of attitudes conducive to health  Inadequate oral health care facilities
Inadequate oral health care facilities  Inadequate oral health manpower planning
Inadequate oral health manpower planning  Insufficient support for research.
Insufficient support for research. Lack of political will
Lack of political will  Inadequate resources (e.g.
Inadequate resources (e.g.  Low priority.
Low priority.
 enabling patients to care for their own oral
enabling patients to care for their own oral keeping patients free from pain and acute disease
keeping patients free from pain and acute disease  maintaining effective oral function
maintaining effective oral function  retaining aesthetics causing no harm.
retaining aesthetics causing no harm. parents/carers
parents/carers  social services/social work departments
social services/social work departments  health visitors
health visitors  general medical practitioner
general medical practitioner  paediatric consultant/other hospital specialists
paediatric consultant/other hospital specialists  school teachers and assistants
school teachers and assistants  colleagues in paediatric dentistry, oral surgery, oral medicine, periodontics, endodontics, prosthodontics, orthodontics.
colleagues in paediatric dentistry, oral surgery, oral medicine, periodontics, endodontics, prosthodontics, orthodontics. obtain a careful medical, dental, family and social history
obtain a careful medical, dental, family and social history  determine the oral/dental needs of the patient
determine the oral/dental needs of the patient  obtain informed consent to any investigations that may be needed
obtain informed consent to any investigations that may be needed  obtain informed consent to the resulting treatment plan.
obtain informed consent to the resulting treatment plan. early assessment of oral health
early assessment of oral health  realistic methods of oral hygiene intervention – a dental hygienist can be particularly helpful in delivering advice and support
realistic methods of oral hygiene intervention – a dental hygienist can be particularly helpful in delivering advice and support  dietary advice – liaise with a dietician where appropriate
dietary advice – liaise with a dietician where appropriate  formulation of an oral health care plan – this should include preventative measures to minimise further oral disease
formulation of an oral health care plan – this should include preventative measures to minimise further oral disease  management of current oral disease – this may include the management of dental emergencies, in addition to stabilisation of oral health status
management of current oral disease – this may include the management of dental emergencies, in addition to stabilisation of oral health status  regular oral examination – the frequency of these examinations must be individually assessed in terms of the risk of further oral disease.
regular oral examination – the frequency of these examinations must be individually assessed in terms of the risk of further oral disease. determine any effect on oral health
determine any effect on oral health  assess the fitness of the patient for the procedure
assess the fitness of the patient for the procedure  decide on the type of behaviour and pain control required
decide on the type of behaviour and pain control required  decide how treatment may need to be modified
decide how treatment may need to be modified  warn of any possible emergencies that could arise
warn of any possible emergencies that could arise  determine any possible risk to staff or other patients/visitors.
determine any possible risk to staff or other patients/visitors.

