Chapter 19
The root filled tooth in prosthodontic reconstruction
Introduction
After endodontic therapy a tooth must be restored to functional and esthetic demands. Teeth which are to be used as abutments in prosthodontic reconstructions must be judged especially carefully regarding their ability to withstand a higher load than a single tooth normally is exposed to (Core concept 19.1). An important consideration is that in most cases the remaining tooth structure will often be substantially less than that in intact teeth because of caries or other causes. Additionally, further loss of tooth structure takes place during the preparation of the access cavity and the root canal. The amount of coronal tooth structure that remains is the most important factor in the decision for the kind of reconstruction to be made as it affects the retention of the restoration and the fracture susceptibility of the tooth. When the remaining tooth structure does not provide enough retention for a core build-up, the root canal can provide enhanced retention by the use of a post. Thus, in a singlerooted tooth with substantial loss of coronal tooth structure, a post and core are often needed.
There is experimental evidence that there are changes in receptor properties in teeth with non-vital pulps leading to higher bite forces than in teeth with vital pulps (Key literature 19.1) (49). This must be considered at the planning stage by estimating the fracture susceptibility of a root filled tooth, especially in a prosthodontic reconstruction substituting more than one tooth.
Problems associated with root filled teeth as abutments
In order to achieve long-term clinical success with prosthodontic restoration of root filled teeth it is essential to know the reasons for clinical failures. Some of these reasons, such as recurrent caries or periodontal breakdown, are the same as in non-root filled teeth. A major difference is the absence of a vital pulp with its potential to respond with specific pain symptoms that may act as an alarm for the patient. To minimize the development of new caries and periodontal disease, an individually adapted regimen of preventive care has to be established including an appropriate recall schedule.
The loss of retention of a crown is possible in non-vital as well as in vital abutment teeth, but in the latter case early symptoms warn the patient. The specific issues associated with prosthodontic reconstruction of root filled teeth are now discussed.
Loss of retention
Retention loss is a failure of the connection between two parts of the restoration or between the restoration and the tooth. A fracture within one of the materials may also result clinically in a loss of retention, but the cause must be differentiated.
When the retention is lost in one abutment, either the complete prosthodontic reconstruction will feel loose, causing only minor symptoms in a tooth with non-vital pulp, like malodor, or it will still be functioning satisfactorily and the failure may remain undetected by the patient. In these cases the diagnosis is difficult but nevertheless important. The continuous gap between crown and tooth gives access to bacteria, possibly causing caries, gingival inflammation, pulpal complications and apical periodontitis, depending on the location of the gap and the seal of the remaining barrier between the gap and the apex. Furthermore, the forces acting on the remaining reconstruction are higher, with an increased risk of fracture or subsequent loss of retention of the other abutments. Therefore, at each recall examination, it is of supreme importance to check the fit of every single abutment in a prosthodontic reconstruction.
The marginal fit is checked visually using loupes and with a suitable fine explorer by trying to penetrate between the tooth and the restoration margin from an apical direction. If a gap cannot be felt, a rocking and a push–pull motion with the fingers may disclose movement of the restoration. In the case of a loose restoration, passage of saliva along the cavosurface margin may be observed.
Factors influencing retention
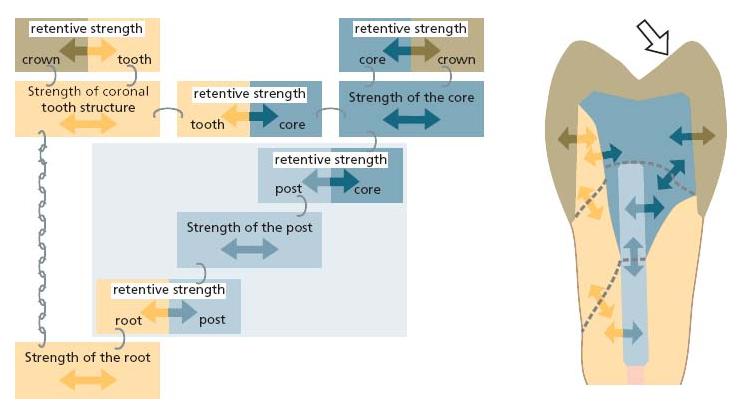
Retention of a core build-up
Assuming that the retention for the crown is sufficient and appropriate to the prosthodontic reconstruction, the retention of the core build-up is the next link in the chain of retention. The more the retention of the crown relies on the build-up, the more important is the retention at the tooth structure. The build-up is attached to the tooth mechanically and may also be adhesively (micromechanically) attached, depending on the material used. A plastic filling material can be condensed or syringed into undercuts, retention grooves or the canal orifices. Additionally, it can be fixed by means of intradentinal pins or a post.
Retention of a post
The retention of a post depends on:
- its design (tapered, parallel, individual);
- insertion depth;
- macroretentions (thread, serrations);
- surface characteristics (composition, roughness, surface energy);
- cementing agent in combination with pretreatment of the dentin surface.
Fractures
Cohesive failure within a material occurs as a fracture.
Fractures of the superstructure
A fracture within the superstructure of a prosthesis does not depend on the endodontic treatment per se and can happen in a vital abutment tooth as well. The only difference is that the reflex control of bite forces is reduced (49) owing to the loss of receptors in the pulp or a change in the mechanoreceptor function in the periodontal membrane.
Core/post fractures
Core: The fracture susceptibility of a core build-up depends mostly on its dimensions, the material’s strength and the forces acting upon it. Regarding these forces, there are major differences between anterior and posterior teeth in the amount and direction of force, the ratio between length and diameter and the area of the bonded surface. When a post is used, its coronal end can weaken the core build-up and exert stress, depending on its size and shape.
Post: A post often is the most retentive link in the chain of retention. In the case of overload either it breaks or it fractures the root, depending on which is the strongest component. The fracture susceptibility of a post depends on its diameter and the material from which it is fabricated.
Tooth fractures – factors influencing fracture risk
- Mechanical characteristics of non-vital dentin: For a long time endodontically treated teeth were thought to be more brittle owing to a loss of moisture content. Several studies have investigated the mechanical properties of dentin in vital versus non-vital teeth (Key literature 19.2) (see also overview in Ref. 32). Although the moisture content did vary significantly, the compression strength and tensile strength did not show any significant difference (28). Thus, factors other than dentin characteristics may be more important in the increased fracture susceptibility of endodontically treated teeth.
- Amount of remaining tooth structure: The loss of tooth structure in an endodontically treated tooth is much more responsible for its higher susceptibility to fracture than changes in its mechanical properties. Posterior teeth with intact marginal ridges and only a small access preparation are most resistant to fracture and are not significantly weaker than intact teeth without any preparation (51, 64). From a prostho dontic point of view, a maximum of internal tooth structure should be preserved to minimize the fracture risk. Thus, ideally, the access would be minimal, i.e. just large enough to gain access to the canal. From this point of view the preparation of the canal, especially in the cervical area, should be as small as possible. This prosthodontic desire is in conflict with modern concepts for root canal preparation in endodontic therapy where direct straight-line access to the canal with a wide access opening for good overview is a general requirement (see Chapter 11). Good cervical flaring is furthermore recommended to ensure an optimal apical preparation, especially in curved canals. In more demanding root canal treatments it might be necessary to sacrifice sound tooth structure, while in nearly straight canals the preservation of tooth structure can be the primary goal.
The prosthodontic reconstruction determines the forces acting on the tooth. The amount of tooth structure left after preparation determines its ability to carry loads. Which type of reconstruction is best suited for the remaining tooth structure needs to be judged at the very beginning of treatment.
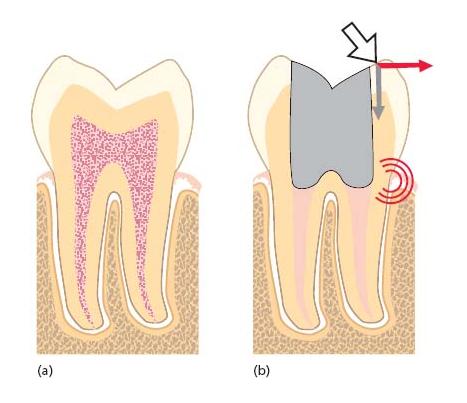
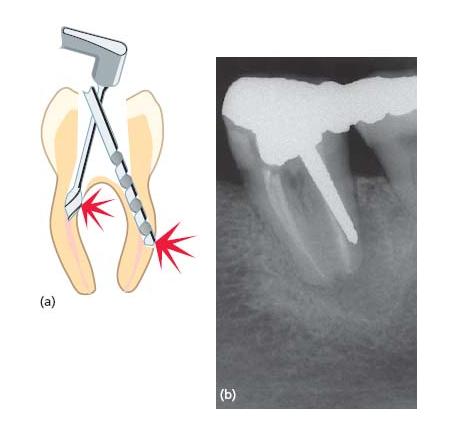
When one or both of the proximal walls are lost, the tooth is substantially weakened as the support of the circumferential marginal ridges (and the roof of the pulp chamber) is lost and a horizontal force on a cusp acts over a long lever-arm on the weakest part in the cervical area, normally just above the alveolar crest. When a force acts on the oblique inner slopes of the cusps it will be divided into a vertical and a horizontal component, the latter exerting high stresses in the weak cervical portion (Fig. 19.1). Therefore an effective bonding or cuspal coverage is necessary whenever a proximal wall is lost and the cusps are not flat owing to abrasion or anatomical form.
Fig. 19.1 (a) Intact tooth. (b) Forces acting on a root filled tooth and resulting stress peak.
The (tensile) bond strength of any material to dentin is always weaker than the (tensile) strength of dentin. Therefore, the preservation of a maximum amount of dentinal bulk should be the aim in endodontic therapy of an abutment tooth.
- Type of post: A stiff material with a high modulus of elasticity may concentrate the forces onto a small area at the end of the post, exerting more stress onto the root; a post material with a similar behavior to dentin could spread the forces, so they decrease towards the post’s tip (Fig. 19.2). This seems to be more favorable with respect to fracture mode (2, 37). A stiff post may induce more damaging types of fractures (Fig. 19.3).
Tapered posts meet the shape of a canal prepared for root filling better than parallel posts which may need additional removal of tooth structure at the apical end. This leads to significant weakening of the root on a level where the thickness of the root is already decreasing naturally (36). - Length of post: The longer a stiff post, the better the distribution of stresses, resulting in reduced stress at the apical end of the post because of leverage (63). Extending the length to two-thirds of the root length results in a superior fracture resistance compared with short posts (29, 55). The length of the post is not so significant for adhesively luted fiber posts (55).
There is a lack of clinical data regarding the length of posts in relation to the level of alveolar bone, but in the case of a metal post it seems more favorable to extend the post below the alveolar crest. - Post diameter: The thicker a post, the thinner and weaker will the remaining tooth structure be, leading to increased risk of fracture. On the other hand, a post must be thick and stiff enough to transmit lateral forces to the root uniformly. Normally, depending on the diameter of the root, the post diameter should not exceed 1.5 mm at the cervical level and in small or fragile roots this is less. The removal of sound tooth structure for placing a post should be considered very carefully.
Fig. 19.2 Distribution of forces by posts with different stiffness.
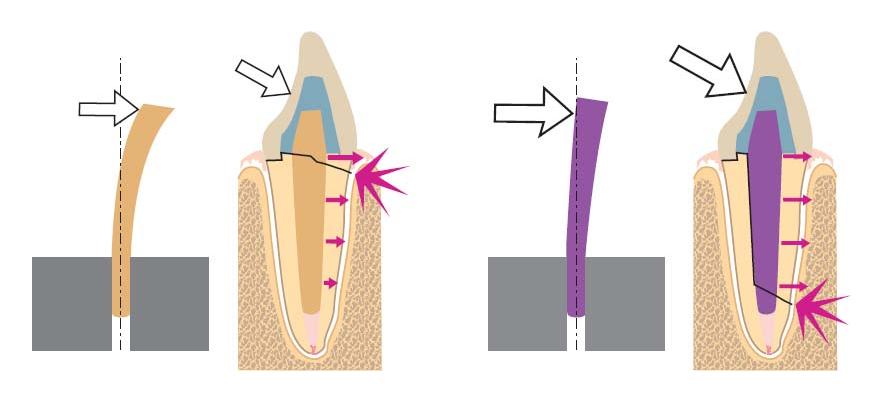
Fig. 19.3 Fracture of root filled tooth 15, probably due to forces from the metallic post. (Courtesy of Dr I.P. Sewerin.)

Fig. 19.4 Correct and incorrect placement of post in distal root of lower molar.
Perforations
Invaginations of the external root surface – stripping perforations
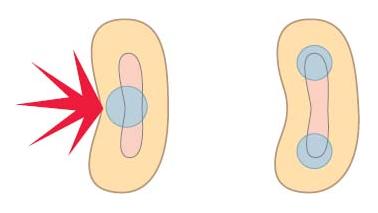
Roots are seldom round and often have curves, invaginations, flutes or other varieties in shape. The distal root of a mandibular molar is kidney-shaped in its cross-section, so care must be taken not to place the post preparation in the middle of the canal but in the bulkiest part of the root, i.e. the buccal or lingual edge (Fig. 19.4).
The mesial root of a lower molar and the mesiobuccal root of an upper molar are often curved in a distal direction. The most cervical parts of the canals go mostly in the mesial direction, so when this initial curve is not removed during the access preparation there is great danger of stripping perforation into the interradicular space or in the mesial direction (Fig. 19.5). Proper flaring and, especially, anticurvature filing are important not only to gain a straight-line access for the apical preparation of the canal but also for safe preparation of the post space (34).
Curvatures not perceptible in the radiograph
Even if the cervical part of the canal is straight, a more apical curvature may limit the length of a post. The most dangerous curvatures are in the plane not perceptible on the radiograph. Only knowledge of the anatomy of the root prevents perforation during preparation of a post space, e.g. the palatal roots of upper bicuspids and molars (75).
Fig. 19.5 (a) Danger of perforation in curved canals. (b) Perforation of the distal root by a post. (Courtesy of Dr I.P. Sewerin.)
Deviation of the prepared canal
Gates–Glidden drills as well as Peeso reamers and some specific drills for post systems have a non-cutting self-centering tip, which ensures that the preparation of the post space will not deviate from a guiding canal being enlarged concentrically. In the case of a root filled tooth, the center of the root filling is the guiding structure. When the root filling deviates from the original canal, the center of the root filling is no longer the center of the root. Enlarging a deviated canal preparation concentrically can therefore cause a lateral perforation, depending on the amounts of deviation, enlargement and dentinal bulk in that direction (24, 34).
Use of end-cutting drills
Special care must be taken when using the end-cutting drills provided with many post systems. Even when driven by hand, they can easily deviate from the canal (Fig. 19.5b). Therefore, removal of the root filling and preparation of the canal space should be done using drills with a non-cutting tip prior to use of the drills for these post systems (24).
Excessive length/diameter
When a post is longer than the straight portion of the canal, a perforation is likely to occur (Fig. 19.5). With increasing diameter of the post, not only the fracture risk but also the risk of perforation increases significantly, therefore a post should always be as thin as possible, i.e. just thick enough to gain some guidance and retention within the canal.
Reinfection/bacterial leakage
Microleakage of cemented posts
A major aim of the root filling is to seal the canal as tightly as possible to hinder bacterial leakage from the oral environment to the periapical tissues. Preparing the canal for receiving a post removes a substantial amount of the root filling and may disturb the seal of the remaining filling. The subsequent cementation of posts may again seal the canal and reduce the risk of infection. Adhesively luted posts leak less than conventionally cemented ones (4) but leakage increases after fatigue loading (53). However, leakage may occur during post space preparation. Immediate post space preparation is less likely to cause leakage than preparation after complete setting of the sealer (1); a root filling without a tight seal of the access cavity allows leakage of bacteria within a few weeks (5), so the post space preparation and the subsequent luting of the post should be established immediately. Aseptic conditions are imperative during post space preparation, so a rubber dam should be used. If this is not possible, there must be adequate moisture control and the post space should be irrigated with antiseptic solutions such as sodium hypochlorite, chlorhexidine or alcohol.
There is clinical evidence that leaving at least 3 mm of apical root filling under posts decreases the probability of occurrence of periapical lesions (35). In vitro studies have shown that a remaining apical root filling of 5 or 7 mm prevents leakage better than one of 3 mm (41), therefore a residual root filling of 3 mm should be the absolute minimum.
Core build-ups
Core build-up without a post
If enough coronal tooth structure remains to yield retention to a core build-up, a post will not be necessary. The build-up will fill the access cavity and any substance loss from caries or other causes, and may increase the height of the abutment. It must be taken into account that during crown preparation the outside walls of the remaining tooth structure will be reduced in thickness or removed completely and so will not contribute to the final buildup retention. The retention of the build-up must be achieved with the tooth structure that will remain after the final preparation.
Modern dentin adhesives are able to retain composite fillings in cavities without any retentive form but they may be overrated in successfully bonding build-up and prosthodontic reconstruction alone. For build-ups, a mechanical retention in addition to dentin bonding should always be used to gain a maximum overall retention.
The possibilities for achieving mechanical retention are different between single- and multirooted teeth. The size of the pulp chamber (in width and depth) in multi-rooted teeth is of considerable advantage for achieving mechanical retention. Undercuts are a natural property of multirooted teeth, with divergent canal orifices providing excellent mechanical retention.
Because forces acting on all teeth are different and depend on the degree of destruction, further mechanical retention may be necessary via grooves (67) or posts. In anterior teeth the forces act in a more horizontal direction and their cross-sectional area is smaller than in posterior teeth. These unfavorable lever-arm relations necessitate the insertion of posts.
Whenever the remaining tooth structure and the pulpal space support sufficient retention for the buildup, a post will not be needed and should be avoided because the risks associated with the use of posts do not exceed the advantages in most cases (Core concept 19.2). Restorations without posts in premolar teeth with their clinical crowns removed resisted similar loads to those resisted by post-restored samples in vitro (10, 22, 65). In substantially decayed incisors, crowns without posts failed at significantly lower forces than teeth with post-retained build-ups did (70). Prospective clinical studies comparing root canal-treated teeth with or without insertion of posts found failure rates of the same level for both types of restorations in single crowns (19, 21/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


