19
Prosthodontic Considerations
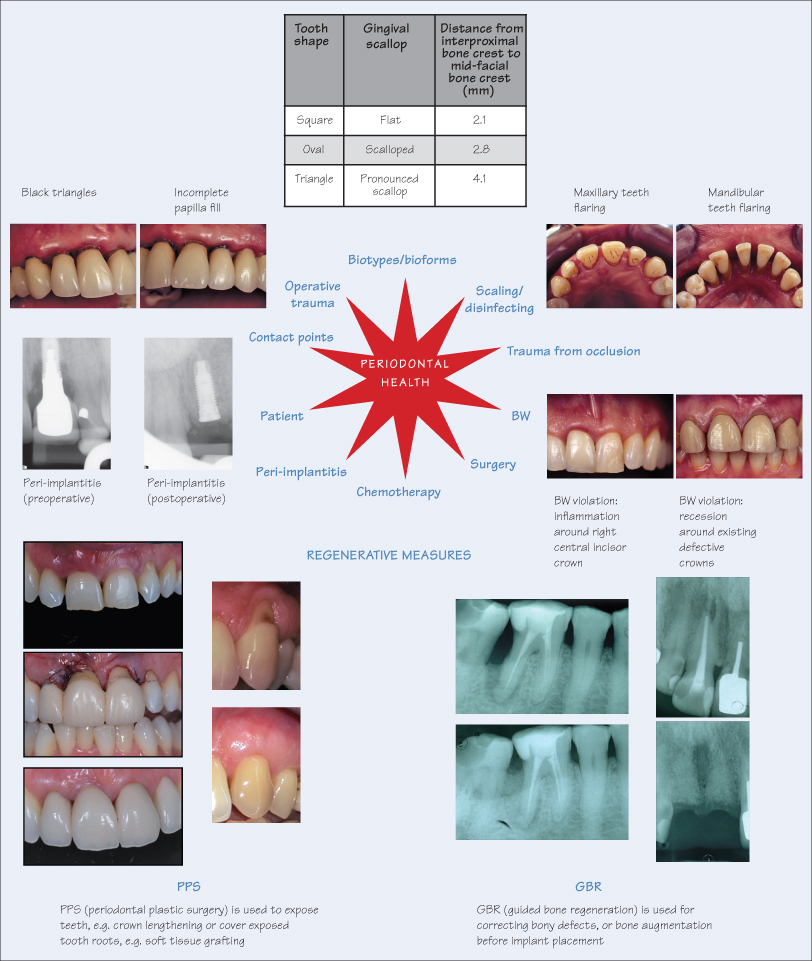
Achieving and maintaining periodontal heath is influenced by numerous factors, including disruption of the biofilm by scaling/root planing, surgery, chemotherapy (local and systemic), patient factors (oral hygiene, constitutional, systemic illness, habits) and degree of operative trauma during clinical procedures. A paradigm shift is also emerging regarding the treatment of periodontal disease. Conventional scaling, root planing and surgery for eliminating pockets is being replaced by a more minimal, non-invasive approach of full-mouth ultrasonic debridement for disrupting the biofilm and thereby achieving disinfection of the root. Periodontal health is essential before starting prosthodontic treatment, and is a constituent of the health, function, aesthetic (HFA) triad.
Periodontal Biotypes and Bioforms
The periodontal biotype plays a significant role when planning prosthodontic and implant therapies. Periodontal biotypes represent gingival texture and architecture around teeth and are classified as:
- Thin-scalloped – delicate, prone to gingival recession, dehiscences and fenestrations;
- Thick-flat – fibrotic, resilient, prone to periodontal pocket formation;
- Medium – intermediate between the above two extremes.
The periodontal bioform describes the degree of gingival scallop around teeth, which is primarily dictated by tooth shape, and can broadly be categorised as square, oval or triangular, corresponding to the flat, scalloped or pronounced scalloped bioforms, respectively.
Contact Points
The relationship of the contact point (either of natural teeth or artificial prostheses) to the interproximal alveolar bone crest determines the amount of interproximal gingival papilla fill. If the distance is 5 mm or less, total papilla fill is evident in the gingival embrasures. If the distance is
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


