Management of Persistent Orofacial Pain
Christian S. Stohler
This chapter presents a framework for the management of persistent orofacial pain conditions. Emphasis is placed on the delivery of care. One-size-fits-all “magic-bullet” practice schemes do not take into account the wide range of case complexity (eg, the intensity and extent of pain, mood-related consequences, disability, and comorbid conditions), making it difficult for the inexperienced practitioner to choose a suitable care environment and appropriate level of care for a given patient. Experience has shown that not all patients with a particular diagnosis benefit from being managed the same way. For this reason, this chapter introduces a framework for clinical decision-making to provide a basis for subsequent chapters dealing with specific pain conditions. This outline acknowledges differences in the care needs of individual orofacial pain patients irrespective of whether the origin of their pain is musculoskeletal, neuropathic, or idiopathic.
Professional Care
Disease taxonomies that distinguish disease subsets for which a specific treatment predicts a greater benefit-risk ratio than other types of care are useful. On the other hand, some disease classifications present no evidence that this benefit-risk response varies among subsets for a given intervention; these classifications imply meaningful information when in fact none exists. Any therapeutic intervention should also be based on reasonable certainty that the patient suffers from a condition for which the chosen care is likely to improve the patient’s life. The guiding principles are that treatment benefits outweigh potential risks and that the costs, both monetary and biologic, are justified by the expected benefits.
Defining the Challenge
There is a great deal of subject-to-subject variation in response to treatment, and most patients experience benefits from a range of therapies, especially when treated for the first time. However, the challenge lies with a subset of patients for whom all current treatments leave much to be desired. It is the growing level of dissatisfaction among such patients that is captured in the voice of patient advocates who call for efficacious therapies, care standardization, safety assurances, and professional accountability.
Using a Case-Specific Approach
Lessons learned from the management of persistent pain teaches us key case attributes that have diagnostic and therapeutic implications include the temporal presentation of pain (persistent or not), the presence and nature of comorbid conditions, the impact on the patient’s life, and the history of previous unsatisfactory treatment attempts. In this respect, it seems appropriate to make the assumption that, compared to a patient exhibiting transient pain, patients with persistent pain have greater chance of continuing to be in pain in the future. Similarly, a patient who has experienced multiple unsatisfactory treatments is more likely to encounter another treatment failure than success.
Another problem is that much comorbidity linked to orofacial pain conditions falls beyond the scope of the dental practice act in almost all jurisdictions and, therefore, requires coordination of care with another health care provider (see also chapter 12). Comorbidities include emotional consequences, such as depressive preoccupation, fear, and anxiety. Physical impairment and disability may exceed the range of services offered in a general dentistry setting. The more complex cases are better dealt with in tertiary care pain clinics, where the emphasis shifts from eradicating pain to improving activity tolerance, preventing deconditioning, and maintaining productivity.
Varying Focus in the Treatment of Pain
In contrast to acute pain and pain associated with terminal illness, persistent pain has an element of permanency. In fact, persistent pain implies that all treatments up to this point have not produced acceptable relief. Given the need for continued care, potential health risks due to long-term treatments need to be considered. Unnecessarily high dosages of pain medication should be avoided, and chances of adverse drug interactions increase with the number of concurrent medications consumed (see also chapter 21). When choosing treatments for persistent pain, the primary focus is safety, with secondary importance given to treatment efficacy and cost. This emphasis contrasts sharply with the management of acute pain or pain of the terminally ill, for which treatment efficacy should be the priority.
Sorting Patients According to Care Requirements
Pain severity, extent, and pain/stress-related consequences vary from patient to patient, calling for the decision as to which care intensity and environment best meet the needs of a particular patient. Whereas transient and infrequent orofacial pains represent more of a nuisance than a burden, severe and persistent pains are debilitating and cause significant life disruption. Impact on patients and their families has to be taken into account.
Both patients and health care providers benefit from the customization of therapy. Referrals should be considered based on the experience and skills of providers and the essential services that are at their disposal. The dentist can offer valuable service in combination with other health care providers, even in the most complex case, and particularly in rural settings, where access to specialty clinics is often limited. For the milder, nondebilitating forms of pain, dentists offer treatment alternatives to pharmacotherapy that are often preferred by patients.
Understanding of complex matters can be achieved through a structured approach to simplify the problem. In this approach, a system is introduced that brings order to a patient population with heterogenous care needs. Among the case attributes with both therapeutic and medicolegal implications, two criteria are critical for sorting patients according to care needs and to further define the dentist’s role: (1) pain severity and (2) relevant comorbid conditions. The decision tree, displayed in Fig 19-1, captures the most salient features and suggests the preferred care setting for case-specific reasoning: (1) dentistry as primary setting for cases of minimal complexity; (2) dentistry in collaboration with the primary medical care for cases of intermediate complexity; and (3) dentistry as a secondary resource for the most complex cases managed by specialty clinics.
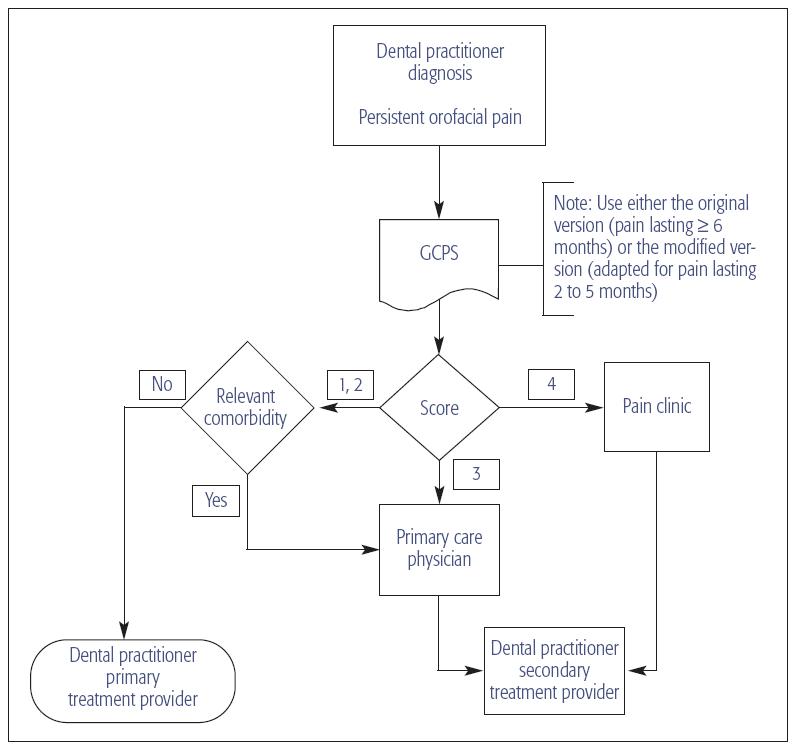
Fig 19-1 Determination of service requirements of patients with musculoskeletal and neuropathic orofacial pains based on assessments of pain severity and impact and the presence or absence of relevant comorbid conditions. Depending on the patient’s response on the original2 or modified Graded Chronic Pain Scale (GCPS), case-specific service requirements are defined. For cases scoring either Grade 1 or 2 on the GCPS, it is further suggested to consider whether the primary care physician should be consulted for comorbid conditions.
The Graded Chronic Pain Scale (GCPS),1,2 which assigns a severity grade to clinical pain lasting 6 months or more (Table 19-1), provides the framework that the inexperienced clinician needs. However, this scale does not cover the complete spectrum of cases because it requires the presence of pain for 6 months minimally. With minor modifications that allow it to acknowledge pain of 2 to 6 months’ duration (see Table 19-1, column 3), the instrument can identify patients not fitting the conservative definition of chronic, but whose care needs are greater than a general dentist can provide. This modification will assist the inexperienced clinician with the sorting of patients according to care-setting needs. Besides the assessment of pain severity and debilitating effects, the dentist must recognize the impact of coexisting illnesses. Pain in parts of the body other than the orofacial complex is not unusual. Often patients do not tell the dentist about conditions outside the orofacial complex because they may think that these are not within the dentist’s scope of practice. These conditions call for coordination of care with the primary care physician.
| Table 19-1 GCPS2 and modified von Korff scale | ||
| Question | GCPS (pain duration > 6 months) |
Modified von Korff Scale |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



