Disease Transmission and Infection Prevention
Learning Outcomes
On completion of this chapter, the student will be able to achieve the following objectives:
• Pronounce, define, and spell the Key Terms.
• Describe the roles of the CDC and OSHA in infection control.
• Explain the difference between Universal Precautions and Standard Precautions.
• Describe the differences between a chronic infection and an acute infection.
• Describe the types of immunity, and give examples of each.
• Give an example of a latent infection.
• Identify links in the chain of infection.
• Describe the methods of disease transmission in a dental office.
• Describe the components of an OSHA exposure control plan.
• Describe the infection control considerations when using high-tech equipment.
• Identify the OSHA categories of risk for occupational exposure.
• Describe the first aid necessary after an exposure incident.
• Discuss the rationale for hepatitis B vaccination for dental assistants.
• Explain the importance of hand care for dental assistants.
• Explain proper hand hygiene for dental assistants.
• Explain the advantages of alcohol-based hand rubs.
• Discuss the types of PPE needed for dental assistants.
• Demonstrate the proper sequence for donning and removing personal protective equipment.
• Identify the various types of gloves used in a dental office.
• Explain the types and symptoms of latex reactions.
• Describe the proper handling and disposal methods for each type of waste generated in dentistry.
• Explain the CDC recommendations regarding the use of a saliva ejector.
• Describe the rationale of CDC recommendations regarding laser plumes.
• Explain the precautions necessary when a patient with active tuberculosis is treated.
Performance Outcomes
On completion of this chapter, the student will be able to meet competency standards in the following skills:
• To perform appropriate first aid after an exposure incident
• To wash hands properly before gloving
• To apply an alcohol-based hand rub
• To properly put on and remove personal protective equipment
Electronic Resources
![]() Additional information related to content in Chapter 19 can be found on the companion Evolve Web site.
Additional information related to content in Chapter 19 can be found on the companion Evolve Web site.
• Labeling Exercise: Areas of the Hand Missed During Handwashing
• Procedure Sequencing Exercises
• WebLinks
![]() and the Multimedia Procedures DVD
and the Multimedia Procedures DVD
Key Terms
Acquired immunity Immunity that is developed during a person’s lifetime.
Acute infection An infection of short duration that is often severe.
Anaphylaxis (an-uh-fi-LAK-sis) Extreme hypersensitivity to a substance that can lead to shock and life-threatening respiratory collapse.
Artificially acquired immunity Immunity that results from a vaccination.
Blood-borne disease Disease such as HBV, HCV, or HIV infection that is caused by microorganisms such as viruses or bacteria that are carried in blood.
Blood-borne pathogens Disease-causing organisms transferred through contact with blood or other body fluids.
Chain of infection Conditions that all must be present for infection to occur.
Chronic infection An infection of long duration.
Communicable disease Condition caused by an infection that can be spread from person to person or through contact with body fluids.
Contaminated waste Items such as gloves and patient napkins that may contain potentially infectious body fluids of patients.
Direct contact Touching or contact with a patient’s blood or saliva.
Droplet infection An infection that occurs through mucosal surfaces of the eyes, nose, or mouth.
Epidemiologic (ep-i-dee-mee-oe-LOJ-ic) studies Studies of the patterns and causes of diseases.
Hazardous waste Waste that poses a danger to humans or to the environment.
Immunity (i-MYOO-ni-tee) Ability of the body to resist disease.
Indirect contact Touching or contact with a contaminated surface or instrument.
Infection control Policies and practices designed to prevent the spread of infectious agents.
Infection prevention Ultimate goal of all infection control procedures and policies.
Infectious disease Disease that is communicable.
Infectious waste Waste that is capable of transmitting an infectious disease.
Inherited immunity Immunity that is present at birth.
Latent (LAY-tent) infection Persistent infection with recurrent symptoms that “come and go.”
Naturally acquired immunity Immunity that occurs when a person has contracted and is recovering from a disease.
Occupational exposure Any reasonably anticipated skin, eye, or mucous membrane contact or percutaneous injury involving blood or any other potentially infectious materials.
OSHA Blood-Borne Pathogens (BBP) Standard Guidelines designed to protect employees against occupational exposure to blood-borne pathogens.
Pathogen (PA-thuh-jen) Disease-causing organism.
Percutaneous (pur-kyoo-TAY-nee-us) Through the skin, such as with a needle stick, cut, or human bite.
Permucosal (per-myoo-KOE-sul) Contact with mucous membranes, such as the eyes or mouth.
Personal protective equipment (PPE) Items such as protective clothing, masks, gloves, and eyewear used to protect employees.
Universal Precautions Guidelines based on treating all human blood and body fluids (including saliva) as potentially infectious.
Virulence (VIR-yoo-luhns) Strength of a pathogen’s ability to cause disease; also known as pathogenicity.
The dental assistant is at risk of exposure to disease agents through contact with blood or other potentially infectious body fluids. In this chapter, you will learn how to break the chain of infection, identify methods of disease transmission, and explain how the immune system provides the body with resistance to infection.
This chapter discusses the Centers for Disease Control and Prevention (CDC) Infection Control Guidelines and the requirements of the Occupational Safety and Health Administration (OSHA) Blood-Borne Pathogens (BBP) Standard. By carefully following the infection control recommendations and safety information provided in this chapter, you can minimize the risks of disease transmission to yourself, your patients, and other members of the dental team.
The Chain of Infection
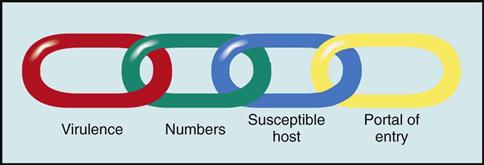
To understand how infection can occur, imagine a chain that has four links. Each link is a condition that must be present for infection or disease to occur. The links in the chain of infection include (1) virulence, (2) number of microorganisms, (3) susceptible host, and (4) portal of entry (Fig. 19-1). Infection control strategies are intended to break a link in the imaginary chain of infection. Break any link in the chain, and you break the infectious process.
Virulence
The virulence of an organism refers to the degree of pathogenicity, or the strength of that organism in its ability to produce disease. If an organism is not very virulent, it may be incapable of causing disease. On the other hand, if an organism is very virulent, it can cause a serious disease. Because the body cannot change the virulence of microorganisms, this task is left to the body defenses and to specific immunizations, such as the vaccine for hepatitis B virus (HBV). Another defense is to avoid coming in contact with microorganisms by always following the infection control techniques described in this chapter.
Number of Microorganisms
To cause disease, a high enough number of pathogenic microorganisms must be present to overwhelm the body’s defenses. The number of pathogens may be directly related to the amount of bioburden present. Bioburden refers to organic materials such as blood and saliva. The use of the dental dam and high-volume evacuation helps to minimize bioburden on surfaces, thereby reducing the number of microorganisms in the aerosol.
Susceptible Host
A susceptible host is a person who is unable to resist infection by a particular pathogen. An individual who is in poor health, is chronically fatigued and under extreme stress, or has a weakened immune system is more likely to become infected. Therefore, staying healthy, washing the hands frequently, and keeping immunizations up-to-date will help members of the dental team to resist infection and stay healthy.
Portal of Entry
To cause infection, pathogens must have a portal of entry, or a means of entering the body. The portals of entry for airborne pathogens are the mouth and the nose. Blood-borne pathogens must have access to the blood supply as a means of entry into the body. This can occur through a break in the skin caused by a needle stick, a cut, or even a human bite. It can also occur through the mucous membranes of the nose and oral cavity.
Types of Infections
Acute Infection
In acute infection, symptoms often are severe and usually appear soon after the initial infection occurs. Acute infections are of short duration. For example, with a viral infection such as the common cold, the body’s defense mechanisms usually eliminate the virus within two to three weeks.
Chronic Infection
Chronic infections are those in which the microorganism is present for a long duration; some may persist for life. The person may be asymptomatic (not showing symptoms of the disease) but may still be a carrier of the disease, as with hepatitis C virus (HCV) or human immunodeficiency virus (HIV) infection.
Latent Infection
A latent infection is a persistent infection in which the symptoms “come and go.” Cold sores (oral herpes simplex) and genital herpes are latent viral infections.
The virus first enters the body and causes the original lesion. It then lies dormant, away from the surface, within a nerve cell, until certain conditions (such as illness with fever, sunburn, and stress) cause the virus to leave the nerve cell and seek the surface again. Once the virus reaches the surface, it becomes detectable for a short time and causes another outbreak at that site.
Another herpesvirus, herpes zoster, causes chickenpox. This virus may lie dormant and later may erupt as the painful disease shingles.
Opportunistic Infection
Opportunistic infections, which are caused by normally nonpathogenic organisms, occur in individuals whose resistance is decreased or compromised. For example, in an individual who is recovering from influenza, pneumonia or an ear infection may develop. Opportunistic infections are common in patients with autoimmune disease or diabetes and in elderly persons.
Modes of Disease Transmission
Before you can prevent disease transmission in the dental office, you must first understand how infectious diseases are spread.
An infectious disease is one that is communicable or contagious. These terms mean that the disease can be transmitted (spread) in some way from one host to another (Fig. 19-2).
Direct Transmission
Direct transmission of pathogens occurs through person-to-person contact. An example would be droplets that are spread through sneezing or coughing, or even by spatter produced during dental treatment. Direct transmission also can occur through unprotected contact with an infectious lesion or infected body fluids, such as blood, saliva, semen, and vaginal secretions. Diseases such as hepatitis, herpes infection, HIV infection, and tuberculosis are spread through direct contact.
Exposure to blood and saliva is a matter of particular concern for dental workers during dental treatment. Although blood may not be visible in the saliva, it often is present.
Indirect Transmission
Indirect transmission occurs when microorganisms first are transmitted to an object or surface, and then are transferred to another person who touches those objects or surfaces. An example would be a dental chart that is handled by a dental assistant while wearing contaminated gloves that is then handled by the receptionist with bare hands. It is important to wash your hands frequently and to carefully disinfect or cover surfaces that can become contaminated to prevent indirect transmission of microorganisms.
Airborne Transmission
Airborne transmission, also known as droplet infection, refers to the spread of disease through droplets of moisture that contain bacteria or viruses. Most of the contagious respiratory diseases are caused by pathogens that are carried in droplets of moisture. Some of these pathogens are carried long distances through the air and through ventilation systems. Airborne transmission also can occur when someone coughs or sneezes.
Aerosol, Spray, or Spatter
Aerosols, sprays, and spatter that are generated during dental treatment can contain blood, saliva, and nasopharyngeal (nasal) secretions. The difference between aerosols, sprays, and spatter is simply the size of the particles. These terms are often used interchangeably to describe droplets of potentially infectious materials.
The finest are the mistlike aerosols. Aerosols can remain airborne for extended periods and can be inhaled. They are not typically visible to the naked eye. Aerosols are created by the use of the high-speed handpiece and the ultrasonic scaler during dental procedures (Fig. 19-3). Inhaling the bacteria in the aerosol (without the protection of a face mask) is comparable to having someone sneeze in your face twice a minute, at a distance of 1 foot. Aerosols can transmit respiratory infections, but they do not transmit HBV or HIV despite the fact that they are inhaled.
Sprays and spatter are also created by the use of the handpiece and the ultrasonic scaler, as well as the air-water syringe, during dental procedures. Spatter consists of larger droplet particles that are contaminated by blood, saliva, and other debris (e.g., calculus, tooth particles).
Spray and spatter droplets travel farther than aerosol mist does and tend to land on the upper surfaces of the wrist and forearms, upper arms, and chest. Droplets also may reach the necktie/collar area of the dentist, assistant, or hygienist.
Intact skin, which is not broken in any way, acts as a natural protective barrier. Nonintact skin, in which a cut, a scrape, or a needle stick injury has occurred, provides a means of entrance for pathogens into the body.
Good work practices such as the use of dental dams and high-velocity air evacuation will help minimize splashes, spatter, and aerosols. In addition, wearing of gloves, masks, eyewear, and protective clothing will reduce the risk of exposure to pathogens.
Parenteral Transmission
Parenteral means through the skin, as with cuts or punctures. Parenteral transmission of blood-borne pathogens (i.e., disease-causing organisms transferred through contact with blood or other body fluids) can occur through needle stick injuries, human bites, cuts, abrasions, or any break in the skin.
Blood-Borne Transmission
Certain pathogens, referred to as blood-borne, are carried in the blood and body fluids of infected individuals and can be transmitted to others. Blood-borne transmission occurs through direct or indirect contact with blood and other body fluids. Saliva is of particular concern during dental treatment because it frequently is contaminated with blood. Remember, although blood may not be visible in the saliva, it still may be present.
Improperly sterilized instruments and equipment can transfer all blood-borne diseases. Individuals who share needles while using illegal drugs easily transmit these diseases to each other. Unprotected sex is another common method of transmission of blood-borne disease.
Common blood-borne microorganisms of concern in dentistry include HCV, HBV, and HIV. Because dental treatment often involves contact with blood and always with saliva, blood-borne diseases are of major concern in the dental office.
Food and Water Transmission
Many diseases are transmitted by contaminated food that has not been cooked or refrigerated properly and by water that has been contaminated with human or animal fecal material. For example, tuberculosis, botulism, and staphylococcal and streptococcal infections are spread by contaminated food or water.
Fecal-Oral Transmission
Many pathogens are present in fecal matter. If proper sanitation procedures, such as handwashing after use of the toilet, are not followed, these pathogens may be transmitted directly by touching another person, or they may be transmitted indirectly through contact with contaminated surfaces or food.
Fecal-oral transmission occurs most often among healthcare and daycare workers (who frequently change diapers) and among careless food handlers.
The Immune System
The immune system is responsible for providing resistance to communicable diseases. A communicable disease is a condition that is caused by an infection that can be spread from person to person or through contact with body fluids.
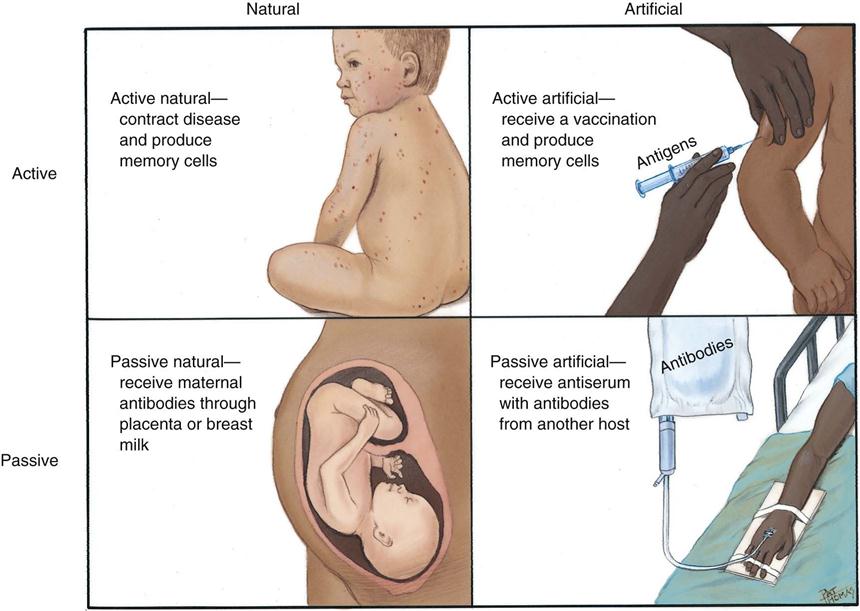
Immunity allows the body to resist disease and prevents foreign bodies from causing infection. When immunity is present at birth, it is called inherited immunity. Immunity that is developed during a person’s lifetime is called acquired immunity. Acquired immunity can occur naturally or artificially (Fig. 19-4).
Naturally Acquired Immunity
Naturally acquired immunity occurs when a person has previously contracted a disease and recovered. When the body was fighting the invading pathogen, it formed antibodies that provide future resistance against that particular pathogen. This form of immunity is called active immunity because the body of the host is actively involved in the process.
Another type, passive immunity, occurs during pregnancy when the fetus receives antibodies from the mother’s placenta. Passive immunity also occurs when the mother breastfeeds the infant. It is called “passive” immunity because the antibodies are acquired from an outside source.
Artificially Acquired Immunity
When the human body has not been exposed to a disease, it has not developed antibodies and is completely defenseless against the disease. However, antibodies can be introduced into the body artificially by immunization or vaccination.
A vaccine that contains weakened disease-causing organisms or genetically engineered organisms is injected into the body. Harmful characteristics of the disease-producing organisms are eliminated from the vaccine to make them less likely to cause disease. The body then forms antibodies in response to the vaccine, resulting in artificially acquired immunity.
Disease Transmission in the Dental Office
Disease transmission in the dental office can occur in a variety of ways, as described below:
Patient to Dental Team
Microorganisms from the patient’s mouth can be passed to the dental team through the following routes:
Infection control measures that help prevent disease transmission from the patient to the dental team member include (1) gloves, (2) handwashing, (3) masks, (4) rubber dams, and (5) patient mouth rinses.
Always remember, a patient may be a carrier of a disease. Carrier-transmitted diseases include certain types of viral hepatitis, herpes, tuberculosis, typhoid fever, and HIV, among others.
Dental Team to Patient
Fortunately, the spread of disease from a member of the dental team to a patient is very unlikely to happen. If proper procedures are not followed, however, disease transmission could occur.
Team-to-patient transmission can result if the dental team member has lesions on the hands, or if the hands are cut while in the patient’s mouth, permitting the transfer of microorganisms. Droplet infection of the patient can occur if the dental team member has a cold, but this can also occur outside the dental office.
Infection control measures that help to prevent team-to-patient transmission include (1) masks, (2) gloves, (3) handwashing, and (4) immunization.
Patient to Patient
Patient-to-patient disease transmission has occurred in the medical field, but only one case of this type of transmission has been documented in dentistry. For this type of transmission to occur, contamination from instruments used on one patient would need to be transferred to another patient.
Infection control measures that can prevent patient-to-patient transmission include (1) instrument sterilization, (2) surface barriers, (3) handwashing, (4) gloves, and (5) use of sterile instruments (Box 19-1).
Dental Office to Community
Microorganisms can leave the dental office and enter the community in a variety of ways. For example, contaminated impressions may be sent to the dental laboratory, or contaminated equipment may be sent out for repair. Office-to-community transmission also can occur if members of the dental team transport microorganisms out of the office on their clothing or in their hair.
Infection control measures that help prevent organisms from leaving the dental office include (1) handwashing, (2) changing clothes before leaving the office, and (3) disinfecting impressions and contaminated equipment before such items leave the office.
Community to Dental Office to Patient
In this type of disease transmission, microorganisms enter the dental office through the municipal water that supplies the dental unit. Waterborne organisms colonize the inside of dental unit waterlines and form biofilm. As water flows through the handpiece, air-water syringe, and ultrasonic scaler, a patient can swallow contaminated water (see Chapter 24).
Roles and Responsibilities of the CDC and OSHA in Infection Control
The CDC and the OSHA are federal agencies that play very important roles in infection control for dentistry (see Chapter 22).
The CDC is not a regulatory agency. Its role is to issue specific recommendations that are based on sound scientific evidence for health-related matters. In 1986, the CDC issued the first recommendations for the dental profession to prevent the transmission of blood-borne disease. OSHA is a regulatory agency. Its role is to issue specific standards designed to protect the health of employees in the United States. In 1991, on the basis of CDC guidelines, OSHA issued the BBP Standard. Failure to comply with OSHA requirements can result in serious consequences, including heavy fines.
As a dental assistant, it is important to follow all of these guidelines and recommendations.
Guidelines for Infection Control in Dental Healthcare Settings (CDC)
In December 2003, the CDC released its Guidelines for Infection Control in Dental Healthcare Settings—2003. Earlier guidelines issued in 1993 had primarily addressed the prevention of blood-borne diseases such as HIV, HBV, and HCV (Fig. 19-5).
The 2003 guidelines expanded upon the existing OSHA BBP Standard and added information on some topics that were not already covered in the 1993 guidelines. In some cases, only a word or two has been added. In others, a significant amount of new information has been added. The guidelines were developed in collaboration with experts on infection control from the CDC and other public agencies; input was also sought from private and professional organizations. These guidelines are based on scientific evidence and are categorized on the basis of existing scientific data, theoretical rationale, and applicability.
The guidelines apply to all paid and unpaid dental health professionals who might be occupationally exposed to blood and body fluids by direct contact or through contact with contaminated environmental surfaces, water, or air.
Although it is not law, the CDC Guidelines for Infection Control in Dental Healthcare Settings now represents the standard of care.
OSHA Blood-Borne Pathogens Standard
OSHA’s BBP Standard is the most important infection control law in dentistry. It is designed to protect employees against occupational exposure to blood-borne, disease-causing organisms, such as HBV, HCV, and HIV.
The BBP requires employers to protect their employees from exposure to blood and other potentially infectious material (OPIM) in the workplace and to provide proper care to the employee if an exposure should occur. This standard applies to any type of facility in which employees might be exposed to blood and other body fluids, including dental and medical offices, hospitals, funeral homes, emergency medical services, and nursing homes.
OSHA requires that a copy of the BBP Standard be present in every dental office and clinic. A copy of the OSHA BBP Standard is available at http://www.osha.gov/SLTC/bloodbornepathogens/index/html.
Exposure Control Plan
Each dental office must have a written exposure control plan that clearly describes how that office complies with the BBP Standard. This exposure control plan must be reviewed and updated at least annually. A copy must be made available to all employees.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses