Chapter 18
Temporomandibular joint arthritis: implications, diagnosis, and management
18.1 The Normal Temporomandibular Joint
18.1.A General Considerations
The temporomandibular joint (TMJ) is a complex synovial joint. It is the only joint in the human body where the condyle slides completely out of its socket and yet is not considered dislocated. This unique joint contains a disk composed of dense fibrous connective tissue, and the temporal and condylar articular surfaces are also covered with the fibrocartilage rather than the more typical hyaline cartilage seen in other joints.1,2 Synovial fluid lubricates the joint, and loading of the articular fibrocartilage and subchondral bone causes chondrocytes in the articular cartilage to synthesize and secrete collagen and proteoglycans and other proteins necessary for cartilage and subchondral bone repair.3–7 Proteoglycan molecules consist of a protein core with negatively charged glycoaminoglycan side chains composed of keratin sulfate and chondroitin sulfate. Aggregates of proteoglycans are linked to a core hyaluronic acid. The twisted structure of this molecule is such that it creates space where water molecules can be bound inside this complex molecule, and compression of the cartilage releases this fluid. It is recaptured as compression is removed. This fluid movement allows cartilage to undergo reversible deformations.
18.1.B Synovial Fluids and the Temporomandibular Joint
Like all synovial joints, the fibrocartilage and TMJ disk are largely acellular and are maintained in health and repaired and lubricated by the synovial fluid in the joint. With either excessive loading or loading without adequate lubrication there is a surface breakdown, leading to microfracture of the cartilage and osteoarthritis. In synovial joints, it has been reported that aging induces articular cartilage thinning and the cartilage actually has a color change (white to a dull yellow). In addition, the fluid that lubricates and protects the joint surface changes with age. With aging, there is reduced accumulation of this synovial fluid and smaller proteoglycans are synthesized, which therefore hold less water and have less compressive ability, and there is more breakdown in the surface of the joint. This produces an increase in keratin sulfate and reduces chondroitin sulfate content in the synovial fluid. These changes are partly caused by the decrease in water content that accompanies aging and a change in cartilage proteoglycan. These changes are considered one of the earliest signs of articular cartilage loss in osteoarthritis. This was clearly demonstrated by a 2002 study8 which examined normal synovial fluid and measured the concentrations of chondroitin 6-sulfate (C6S), chondroitin 4-sulfate (C4S), and hyaluronic acid (HA) in healthy subjects of different ages. The subjects were 82 healthy volunteers ranging in age from 20 to 79 years. They found that the concentrations of CS and HA varied with age. Their values were highest between 20 and 30 years of age, and thereafter they showed a tendency to decrease. The ratio of C6S to C4S was significantly lower in the group aged 60–70 years compared with the group aged 20–30 years. In fact, multiple regression analysis demonstrated that age was, strongly, negatively correlated with the C6S concentration and the C6S:C4S ratio.
18.1.C Age Profiling of TMJ Disease
Arthralgia, arthritis, and arthrosis are among the most common conditions that affect the TMJ. With trauma and time, starting in the early 30s, the cartilaginous surfaces of the TMJ start to show wear-and-tear deterioration, which is then called osteoarthritis. When this wear-and-tear process starts to affect more than one or two joints, this is described as a polyjoint arthritic disease process and it is more common in patients over the age of 50. As might be expected considering this high prevalence, the social and economic impact of rheumatic diseases taxes our healthcare systems. Adults over the age of 65 have more patient visits for these diseases than any other age group.9 In addition to clear-cut rheumatologic disease, there are more than 100 medical conditions that affect the muscles and tendons and joints that are classified as musculoskeletal related diseases. It is postulated that approximately nearly 1 in 5 adults of the US population is also demonstrating signs and symptoms of musculoskeletal disease.10 Moreover, $118.5 billion per year was spent by US citizens on the care of musculoskeletal diseases. Over $86.2 billion is spent annually on rheumatic diseases. The percentage cost of the US gross national product used to treat musculoskeletal disease has increased each decade since the 1960s. When these diseases are severe, mobility and functional limitations cause increased work loss, disability, nursing care, and premature retirement. Musculoskeletal disorders are second only to heart diseases as a cause of work disability. Work-loss costs associated with rheumatic diseases account for 50–76.5% of all indirect costs. Therefore, it is important to understand the disease process and to develop new therapeutic strategies.
18.2 Arthritic Disease of the TMJ
18.2.A Description and Prevalence
Osteoarthritis is considered a disease of the bone, cartilage, and supporting tissues and is the result of both mechanical and biologic events that destabilize the normal coupling of degradation and synthesis of articular cartilage and subchondral bone.11 It is characterized by degeneration of joint cartilage with osseous erosion and sclerosis and sometimes osteophyte formation occurring at the joint margins.12 Age is considered to be the primary risk factor for osteoarthritis and the increase in prevalence with age that is observed in patients with osteoarthritis is likely a consequence of biological changes that occur with aging.13,14 When an elderly patient attends a dentist’s office with a complaint of jaw pain, the most likely diagnosis is localized arthritis (assuming they do not exhibit polyjoint arthritic disease). This can usually be discovered with palpation, auscultation, and radiographic examination of the joint. Occasionally the reason for the jaw joint pain is related to a disk derangement of the jaw (clicking, locking, and/or dislocation), but osteoarthritis is the more prevalent problem in the elderly. In a study based on a European population, it was reported that the prevalence of osteoarthritis is approximately 12% for subjects between 25 and 50 years of age, but in the subset of patients over 60 years this prevalence reaches as high as 95%.15 Fortunately, osteoarthritic changes in the TMJs of an elderly population are much less prevalent than the above data might suggest for all body sites. In a random sample (n = 88) of elderly subjects (between the ages of 76 and 86 years) living in Helsinki the most frequent radiographic finding in the TMJ was flattening of the articular surface, indicating osteoarthritis. This was found to occur in 17% of the population.16
Still, 17% of the population over 65 with TMJ osteoarthritic change is a large group of patients. It is likely that as many as 50% of those with radiographic change have a mild to moderate (or worse) level of pain and dysfunction in their jaw. Aging in-and-of-itself is not thought to cause osteoarthritis, but if a combination of several age-related changes occurs in the same individual, then osteoarthritis will result. Specifically, forceful repetitive function (e.g., bruxism) and/or disk displacement along with synovial fluid alterations of the TMJ will predispose an individual develop osteoarthritis. Localized osteoarthritis is usually thought to be traumatic (either macrotrauma or repetitive microtrauma) in nature but could also be due to a rare infective arthritic disease. Chondrocytes in human articular cartilage collected from patients whose age ranged from 1 to 87 years showed that there is an age-related increase in the accumulation of senescent chondrocytes in the articular cartilage. Furthermore, in vitro studies have demonstrated that chondrocytes subjected to repetitive exposure to peroxide or that have grown under superphysiologic oxygen tension undergo premature aging and that excessive mechanical stress applied to cartilage results in significant increased production of oxidants.17
18.2.B Pathophysiology of Osteoarthritis
Susceptibility to develop osteoarthritis increases and is determined when local factors, such as joint deformity and previous damage to important protective structures in the joint, which leave the joint vulnerable to normal activities, are combined with systemic vulnerabilities.18 Nonetheless, despite the nature of the initiating factors of osteoarthritis, the pathological progression follows a typical pattern.19 The onset of osteoarthritis tends to be insidious and the progression of the disease tends to take a chronic course. Loss of articular cartilage is the hallmark event in osteoarthritis, therefore is the structure that has attracted most attention in relation to the pathogenesis of this condition. However, the pathophysiology of osteoarthritis involves the whole joint, and other associated structures can also be affected, such as the subchondral bone, the soft-tissue structures in and around the joint, such as ligaments, capsule, and muscles. Besides progressive cartilage loss, the structural changes observed include increased subchondral plate thickness, formation of new bone at the joint margins (osteophytes), and development of subchondral bone cysts.20 In the earliest phases of osteoarthritis there is chondrocyte clustering as a result of increased cell proliferation and a general upregulation of synthetic activity leading to a hypertrophic repair of the joint tissue, which results in a thicker than normal cartilage appearance, a phase which can last for decades. As the disease progresses there is a decrease in proteoglycans.21 The loss of proteoglycans causes the softening and reduction in the thickness of the joint cartilage. The ultimate result is the appearance of vertical defects or gaps, a process called fibrillation. At this stage, the underlying bone is exposed due to the disappearance of the cartilage. Subsequently the exposed bone remodels and hypertrophies, leading to sclerosis, new bone formation at the joint margins (osteophytes), and subchondral cyst formation.22
Osteoarthritis traditionally has been regarded as a noninflammatory process, but recent studies using improved detection methods have shown the involvement of altered inflammatory pathways. These observations provide strong evidence for inflammation as one of key mechanisms in the pathogenesis of osteoarthritis, at least in some patients and some phases of the disease process. In a recent study significantly lower levels of the inflammatory mediator peroxisome proliferator-activated receptor gamma (PPARγ) were found in the cartilage of patients with osteoarthritis in comparison with cartilage from healthy individuals.23 This study also demonstrated that interleukin 1(IL-1), tumor necrosis factor alpha (TNF-α), interleukin 17 (IL-17), and prostaglandin E2 (PGE2) induce downregulation of PPARγ, suggesting that downregulation of this chondroprotective molecule might be one of the mechanisms involved in cartilage degeneration. Moreover, it has been suggested that inflammation and cartilage destruction may be two separate pathogenic events: IL-1 has been shown to be responsible for the infiltration of inflammatory cells into the joint and the loss of proteoglycans from cartilage. On the other hand TNF-α, which has many of the properties of IL-1, also induces the infiltration of inflammatory cells into the joint; however, it fails to cause significant cartilage destruction. Since TNF-α, has effects on chondrocytes similar to the effects of IL-1, in combination these two cytokines yield a strong synergistic effect.24,25 In fact, IL-17, TNF-α, and IL-1 have been considered potential targets in arthritis therapy.26 Furthermore, previous studies have demonstrated that there is a correlation between increased synovial fluid levels of TNF-α in patients with chronic inflammatory disease of the TMJ and pain levels on the TMJ during mandibular movement and upon palpation of the posterior aspect of the TMJ capsule.27,28
18.2.C Signs and Symptoms
Common symptoms experienced by patients early in the course of arthritis include joint pain that worsens with activity but is relieved at rest. However, if the disease has reached an advanced, severe stage the patients might experience pain even at rest. Additionally, another sign of advanced disease is internal derangement which might lead to “locking” of the joint. Another common symptom is morning stiffness or following inactivity which, unlike other types of arthritis, rarely exceeds 30 minutes. Characteristic signs of clinically evident osteoarthritis are decreased range of motion, bony enlargement, occasional effusion, variable degrees of inflammation, and crepitation which is considered to be a late manifestation of the disease. The usual presenting symptom is pain, which can involve one or only a few joints. Tenderness on palpation at the joint line and pain on passive motion are also common, although not unique to osteoarthritis. The presence of osteophytes is not only the most specific radiographic marker of osteoarthritis but is also indicative of advanced disease. Additionally, other radiographic findings found in osteoarthritis include decreased joint space, subchondral sclerosis, and subchondral cysts.29
The most common form of arthritis that affects the TMJ is osteoarthritis. The spectrum of clinical signs and symptoms found in osteoarthritis are equal in all the joints including the TMJ. Therefore, the affected patients present with pain, crepitus, joint space narrowing—symptoms which may only be evident at late stages of the disease (Figs. 18.1 and 18.2).30 Martinez et al. studied the clinical and radiological features of patients with osteoarthritis of the TMJ. They identified crepitation as the most relevant clinical finding (93% of cases), along with limited mandibular movement range. Furthermore, the most relevant finding on radiographic examination was alteration of joint surface morphology (62–68% of cases). The most frequent radiographic finding in the TMJ was flattening of the articular surface, which occurred in 17% of the population.31 Another study investigated the prevalence of jaw pain in patients that presented with rheumatoid arthritis (RA) and osteoarthritis. After analyzing 4,011 patients with osteoarthritis they found that 18.6% of the patients presented with pain. They concluded that patients who experienced jaw pain may have decreased functional ability, as well as decreased quality of life.32
Figure 18.1 Osteoarthritis affecting the temporomandibular joint (TMJ). Computed tomographic scan of left TMJ (A) and right TMJ (B); panoramic radiograph (C) of the same patient, showing erosive and irregular cortical outline of the surface of the condylar head characteristic of degenerative changes secondary to osteoarthritis in both TMJs.
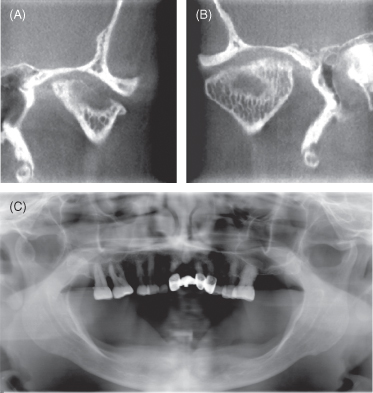
Figure 18.2 Another case of TMJ osteoarthritis. Panoramic radiograph showing a left TMJ with extensive degenerative changes on the left condyle with loss of structure, loss of articular joint space, and involvement of the articulating surface.

18.2.D Treatment of TMJ Osteoarthritis
When management of joint pain symptoms is required, the principles governing treatment of the TMJ are no different than those used with any other body joints with painful osteoarthritis. A table listing the all common treatment of TMJ osteoarthritis is provided (Table 18.1).
Table 18.1 Treatment methods for TMJ arthritis
| Nonpharmacological | |
| Education |
|
| Physical therapy |
|
| Occlusal appliance |
|
| Pharmacological | |
| Nonopioid analgesics and NSAIDs |
|
| Corticosteroid injection (triamcinolone) |
|
| Intra-articular hyaluronic acid injection (Synvisic and Hyalgan) |
|
GERD, gastro-esophageal reflux disorder; NSAIDs, nonsteroidal anti-inflammatory drugs; TMJ, temporomandibular joint.
Nonpharmacologic Treatments
The elements of the nonpharmacologic treatment approach are education, avoidance of harmful behaviors, and in-office physical therapy including daily exercise and use of an occlusal appliance (when tooth clenching or an unstable bite is evident).
Education
One consistent feature of TMJ arthritic disease management is that the patient must be taught about the chronic nature of the disease. It is sometimes difficult for the patient to accept that the damaged joint tissues cannot be repaired or replaced. For instance, it has been shown that patients that have a high degree of jaw function inference show a poorer prognosis when treated with self-directed physical therapy and over-the-counter nonsteroidal anti-inflammatory drugs.33 Depending on what medical information the patient has been exposed to they might have unrealistic treatment expectations that can lead to frustration and depression.
Avoidance of Harmful Behaviors
The patient must be taught to identify and avoid stressful jaw function (e.g., chewing hard foods) and reducing or eliminating aggravating factors such as teeth clenching, opening wide, and gum chewing.
In-Office Physical Therapy
A combined systematic guided musculoskeletal therapy program including exercises, how to properly apply heat and/or ice packs to the jaw, and cognitive self-management skills has been shown to reduce self-reports of pain in a population of patients with chronic myofascial pain.34 The most important exercises are the “N”-position exercise, which involves placing the jaw and tongue in the position achieved when the letter “N” is said and holding it for a count of 10. The patient is instructed to perform this exercise every 2 hours each day (or 6 times a day). The goal is to put and hold the jaw in the most relaxed jaw position where the teeth are apart and the lips not touching. Once the patient’s initial pain symptoms are shown to be reducing, the next exercise is called the jaw hinge exercise. This involves instructing the patient (using mirror feedback) to carefully move the jaw in a strict hinge motion to a point about 15 mm open and then back closed again. This movement promotes synovial fluid movement without any translation of the condyle. The motion is usually performed done 15 times on a 2–3 hour schedule or 6 times a day. When the N-position and hinge exercises help reduce strain on the joint, it is also advisable to use 20 minutes of heat therapy (hot towels, or a moist heating pad) applied to the sorest muscles. Heat helps to reduce pain and stiffness by relaxing aching muscles and increasing circulation to the area. Finally, nonopioid analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs) can be used.
NSAID Treatments
Indications
When and how to use NSAIDs for inflammation and pain control is discussed in detail in Chapter 3 and is not covered here.
Dosage and Adverse Effects
This is information is provided in Chapter 3.
Efficacy
Pharmacologic treatment of arthritis (of all types) aims to decrease pain and inflammation and includes non-narcotic oral analgesics, such as acetaminophen, in those with pain complaints. With regard to selection of an NSAID versus a nonopioid analgesic medication for osteroarthritis, the American College of Rheumatology (ACR) guidelines emphasize that acetaminophen should be the first-line treatment for osteoarthritis of the hip and knee.35–37 We also suggest this is the case for TMJ osteoarthritis, but the dose of acetaminophen that has been used in the studies on which this recommendation is based is 4000 mg per day—a dose that is closer to the toxicity level than many practitioners and patients are comfortable with. Moreover, the magnitude of the pain reduction this dose of acetaminophen induces in osteoarthritis is only minimal. In cases where the patient cannot or will not take this much acetaminophen or where the pain is not effectively controlled, an alternative is to use NSAIDs. Several medications in this drug class are reasonable options (e.g., ibuprofen, naproxen sodium, and nabumetone) and if the patient has a gastric sensitivity making it more logical to use cyclooxygenase-2 (COX-2) selective medications, they have three options here also (celecoxib, meloxicam, etodolac). These medications are reviewed in detail in Chapter 3 and they have reasonable efficacy for arthritic disease, although they must be used with caution.
Nutritional Supplements
Indication
A method of treatment that patients experiment with is the use of “nutraceutical” supplements such as glucosamine and chondroitin sulfate. Chondroitin sulfate is a major component of aggrecan, and glucosamine sulfate is a normal constituent of glycoaminoglycans; both are believed to be involved in restoring the balance in cartilage metabolism.
Dosage and Adverse Effects
It is commonly recommended that a patient consume 1500 mg of glucosamine and 1200 mg of chondroitin sulfate daily. There are very few adverse events associated with this supplement.
Efficacy
The Glucosamine/chondroitin Arthritis Intervention Trial (GAIT), a 24-week, randomized, double-blind, placebo- and celecoxib-controlled, multicenter trial, evaluated the effect of these two supplements, given as 1500 mg of glucosamine and 1200 mg of chondroitin sulfate daily.38 The results showed that treatment with glucosamine and chondroitin sulfate in combination may be effective in the subgroup of patients with moderate-to-severe knee pain; however, their effect failed to be superior to celecoxib. Studies evaluating the efficacy of glucosamine and chondroitin in osteoarthritis of the TMJ remain lacking. A recent (2009) study suggested that these two agents are better when combined versus monotherapy, but noted that research is lacking on this issue.39
Corticosteroid Injections
Indications
Corticosteroid injections are clearly helpful with any inflammatory-based TMJ pain problem when it is unresponsive to the usual treatments and in those patients with gastritis or gastro-esophageal reflux disorder (GERD). In such a situation, the corticosteriod agent is injected directly into the TMJ.
Dosage
When a corticosteroid intra-articular injection is indicated, several different corticosteroids can be used; a common one is triamcinalone.40,41 The usual dose of medication injected in a single jaw joint is 10–20 mg. The injection is targeted to the superior joint space and usually the corticosteroid is mixed with an equal amount of local anesthetic to make the joint injection more comfortable. After the injection, it is wise to recommend ice packs as needed and a completely soft diet for 48 hours until the injection has an effect on the inflammation. The general guideline suggested is that the TMJ should not be injected more than twice in a 12-month period.
Adverse Effects
The issue of whether there are any long-term adverse effects of repeated corticosteroid injections on the TMJ has been examined in several studies. In a study using computed tomography (CT) examination of 36 patients before and after TMJ injection of either corticosteroid or hyaluronate, there were found no changes of osteoarthritic abnormalities in the treated joint after 6 months post-treatment.42 Additionally, in a long-term (12 years) follow-up of 21 patients with rheumatoid arthritis (RA) and symptomatic TMJs who received either an intra-articular injection of a steroid (n = 11) or a local anesthetic agent (n = 10), 14 patients reported no pain arising from the TMJ. Radiographic follow-up examination was performed on 12 of these patients and all but 4 of the 24 joints had structural bone changes. Interestingly the magnitude and prevalence of change was no different for the two groups. They concluded that the odds of long-term progression of joint destruction for the steroid and the nonsteroid injected joints were equivalent in this patient group with RA.43 Presumably these results would be generalizable to osteoarthritic disease in the TMJ also. Moreover, a more recent retrospective chart review of 25 patients with juvenile idiopathic arthritis affecting the TMJ who had received one or more intra-articular joint injections showed that these patients tend to have only minimal adverse events.44 Another study, on effects of CT-guided injections of corticosteroids, no adverse effects were reported after 1 year of the corticosteroid injections and the only side effect reported was a short-term facial swelling in 2 of the 13 patients studied.45 Conversely, other clinicians have reported adverse effects on the TMJ as a result of chronic corticosteroid administration, although the generalizability of such isolated data is highly suspect.46,47
Efficacy
In a 4-week study of three treatment groups totaling 41 patients with temporomandibular d/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


