CHAPTER 18
Frontal Sinus Fractures
Gabriel C. Tender,1 Arnett Klugh III,2 Min S. Park,2 Robert M. Laughlin,3 and Christopher J. Haggerty4
1Department of Neurosurgery, Louisiana State University Health Sciences Center, New Orleans, Louisiana, USA
2Department of Neurosurgery, Naval Medical Center San Diego, San Diego, California, USA
3Department of Oral and Maxillofacial Surgery, Naval Medical Center San Diego, San Diego, California, USA
4Private Practice, Lakewood Oral and Maxillofacial Surgery Specialists, Lees Summit; and Department of Oral and Maxillofacial Surgery, University of Missouri–Kansas City, Kansas City, Missouri, USA
A method of correcting cosmetic and functional defects of the frontal sinus via obliterating nonfunctional nasofrontal ducts (NFDs) and reconstructing the anatomy of the anterior table. A method of prophylactically minimizing the formation of mucoceles and pyoceles by removing respiratory mucosa from the frontal sinus. A method of removing displaced posterior table segments via craniotomy and cranialization.
Indications to Frontal Sinus Obliteration
- Significant anterior table displacement
- Significant anterior table comminution
- Foreign body within the frontal sinus, contaminated site
- Potential injury to NFDs
- Cosmetic deformity
Indication for Frontal Sinus Cranialization
- Significant posterior table displacement
- Significant posterior table comminution
- Penetrating injury
- Foreign body within the anterior cranial fossa
- Cerebrospinal fluid (CSF) leak with extensive dural tears
- Frontal lobe damage or need for craniotomy access
Contraindications for Surgical Management of Anterior Table Frontal Sinus Fractures
- No evidence of NFD damage on computed tomography (CT) scanning, and minimal cosmetic defect
- Medically unstable
Contraindications for Surgical Management of Posterior Table Frontal Sinus Fractures
- Nondisplaced posterior table fractures
- Medically unstable
Anatomy
The frontal sinus begins to develop at age 6 and is completely developed by age 12–16. The floor of the frontal sinus is formed medially by the ethmoid bones and laterally by the supraorbital roof. The entire frontal sinus is lined with pseudostratified ciliated respiratory epithelium. The cilia beat backward and medial to lateral as they push mucus into the NFDs, which drain below the middle meatus, anterior to the ethmoid infundibulum.
Coronal Incision Layers
- Skin
- Subcutaneous connective tissue
- Galea aponeurotica
- Loose areolar subgaleal connective tissue
- Pericranium
Surgical Management of Anterior Table Frontal Sinus Fractures
- The patient is positioned in 30° reverse Trendelenburg. The head is placed within a Mayfield headrest (with or without three-pin skull fixation), and the head is positioned in 15–20° extension. The scalp is prepped and draped in a sterile fashion.
-
Triple-antibiotic ointment and a comb may be utilized to create a horizontal part within the patient’s hairline approximately 5 cm posterior to the patient’s hairline. Alternatively, a strip of hair may be shaved within the site of the proposed coronal incision. For patients with signs of male pattern baldness, it is acceptable to place the incision more posteriorly in order to minimize the potential for a noticeable scar (Figure 18.4 [all figures cited in this chapter appear in the Case Reports]).
-
Local anesthesia containing epinephrine is injected along the incision line, and tumescent solution is deposited within the loose areolar subgaleal connective tissue in order to further aid in hemostasis and to hydrodissect this layer from the underlying pericranium (Figure 18.6).
- A scalloped coronal incision (Figure 18.4) is created from preauricular region to preauricular region. The inferior extent of the incision is determined by the amount of exposure required. The forehead and supraorbital regions can be accessed by limiting the inferior incision to the level of the auricular helix. Access to the zygomatic arch requires a preauricular extension to the level of the ear lobe (Figure 18.5).
- Scalp bleeding is controlled with either Raney clips or needle-tipped cautery.
-
Elevation of the coronal flap occurs within the subgaleal loose areolar connective tissue just superficial to the pericrainum (Figure 18.7). The temporal and preauricular plane of dissection is superficial to the temporalis fascia (Figure 18.8). Care is taken during coronal flap design and reflection to preserve pericranial attachments for the use of a pedicled, vascularized pericranial flap (Figure 18.18).
-
The anterior table of the frontal sinus is removed in order to allow for wide surgical access of the frontal sinus. The peripheral margins of the frontal sinus can be identified with instrumentation (Figure 18.10) and/or a fiber-optic light source (Figures 18.9, 18.31, and 18.32). The anterior table may be removed with any combination of saws, burs (Figure 18.11), chisels, and/or ronguers. The use of saws and burs will frequently allow for the anatomical repositioning of the removed segments at the completion of the frontal sinus exploration or obliteration.
- Once all bony fragments from the anterior table have been removed, the NFDs are evaluated for trauma and patency. Patency is determined by placing a sterile medium within the frontal sinus (propofol, methylene blue, or sterile water) and observing for drainage from the nasal cavity or posterior oral pharynx. Frontal sinuses with patent NFDs are repaired by anatomically reconstructing the anterior table. If damage to the NFDs is suspected, a curette and/or handpiece is utilized to remove bony septi and mucosa from within the NFDs and from the entire frontal sinus (Figures 18.13, 18.14, 18.15, 18.16, and 18.17).
- The NFDs are obliterated with temporalis muscle and fibrin sealant (Figures 18.20 and 18.21). A pedicled pericranial flap is laid within the frontal sinus (Figure 18.22). In cases where the pericranial flap does not completely fill the frontal sinus defect, either abdominal fat (Figure 18.23) or a synthetic filler may be utilized to obliterate the frontal sinus defect.
- Depending on the comminution of the anterior table, the original segments of the anterior table are anatomically repositioned (Figure 18.24) and secured with rigid fixation (Figure 18.25), or a titanium mesh is placed.
- The coronal incision is closed in a three-layered fashion: 2-0 interrupted Vicryl sutures to reapproximate the galea, 3-0 Vicryl sutures to reapproximate the subcutaneous tissue, and 3-0 nylon sutures or skin staples to close the skin. If a pre-auricular extension was required, the subcutaneous tissues are closed with 4-0 Monocryl sutures, and 5-0 plain gut sutures are used to close the skin (Figure 18.26).
- A thin layer of triple-antibiotic ointment, an overlying telfa dressing, and a light pressure dressing are placed over the incisions. Drains are typically not required with adequate closure.
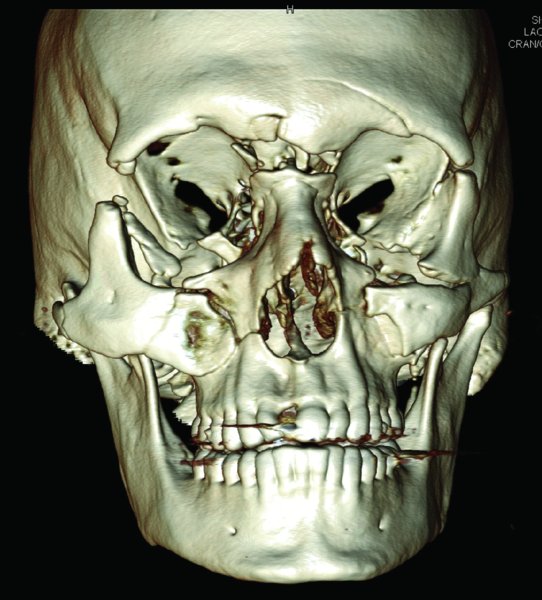
Figure 18.1. 3D reconstruction demonstrating frontal sinus fractures with associated facial fractures.
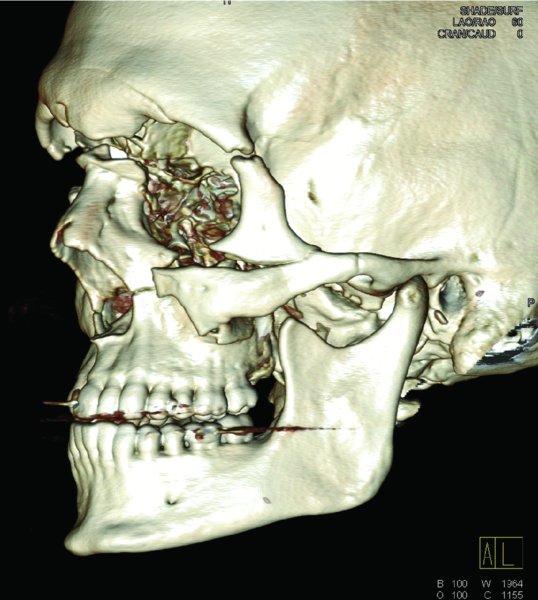
Figure 18.2. Lateral 3D reconstruction demonstrating displaced fractures of the frontal sinus and gross comminution of the bones comprising the nasofrontal ducts.
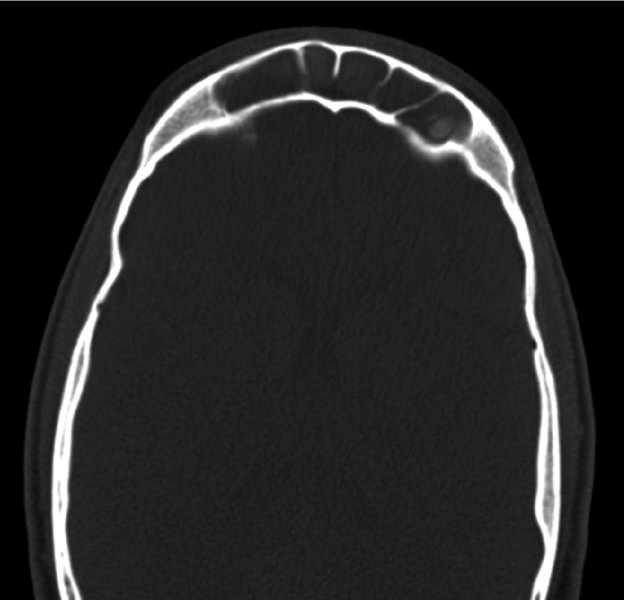
Figure 18.3. Axial computed tomography scan demonstrating an intact posterior table with no evidence of intracranial injuries, fluid within the frontal sinus, and multiple frontal sinus septi.

Figure 18.4. A scalloped marking is made posterior to the hairline at the site of the proposed coronal incision.

Figure 18.5. The lateral extent of the coronal incision will be extended to the level of the ear lobe to allow for exposure of the frontal sinus and other associated facial fractures.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


