Jean-Paul Goulet
Sandro Palla
Patients complaining of acute or chronic orofacial pain often first consult a general dentist, whose task is threefold: (1) to establish the correct diagnosis, (2) to determine the cause of the pain, and (3) to select the treatment plan. A decision to refer to an expert for further evaluation can be made at any stage, but it is mandatory in the case of chronic pain. The aim of this chapter is to describe the diagnostic process and provide a diagnostic framework for the following chapters on pain management.Chapter 27 outlines cases that illustrate this process.
Overview of the Diagnostic Process
The clinical reasoning leading to a final diagnosis follows a hypotheticodeductive process (Fig 17-1). This process includes the practitioner’s memory of clinically relevant knowledge gained by formal training, as well as exposure to different clinical conditions and procedures. To develop clinical expertise, acquired knowledge and cognitive processing need to be reorganized to fit the domain of expertise. The richness of such knowledge contributes to the buildup of meaningful sets of illness scripts that are used in the deductive process to test diagnostic hypotheses by pattern recognition.1
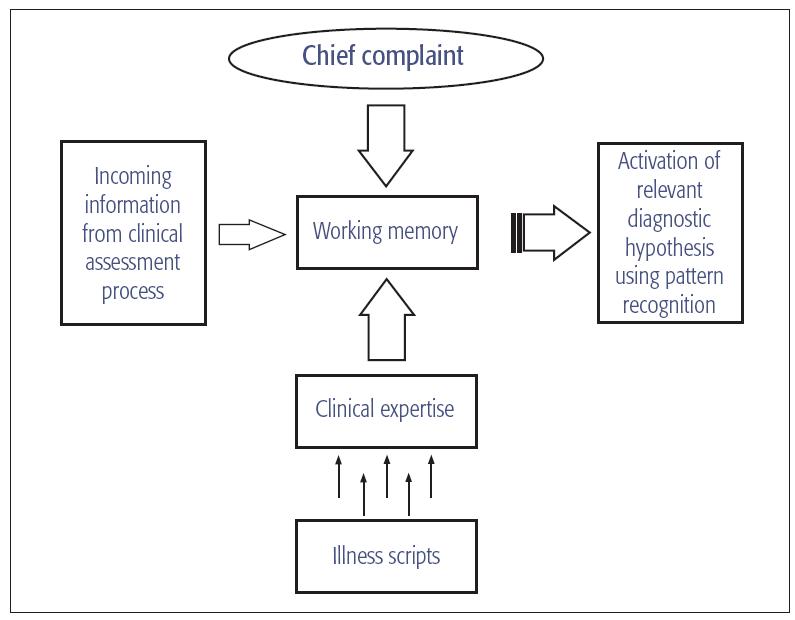
Fig 17-1 Clinical reasoning process that leads to diagnosis.
Gathering all anamnestic information represents the key starting point for creating the patient’s database, which then feeds the clinical reasoning process. While doing this, the clinician’s working memory analyzes, weighs, compares, and reassesses incoming information so as to place it in proper perspective. The next step consists of developing a provisional or differential diagnosis from a list of all possibilities and ranking them from the most to the least probable. Clinicians’ experience and knowledge of signs and symptoms, natural course, distribution, and possible mechanisms, in combination with their familiarity with the diagnostic criteria of the different orofacial pain conditions, are therefore invaluable in the making of meaningful connections with the patient’s database. At this stage, the decision to seek additional clinical information or to refer the patient to a specialist usually takes place. An action plan is then developed based on a working diagnosis.
In many instances, confirming a definitive diagnosis might not be possible due to the lack of disease-specific signs, objective tests, and precise diagnostic criteria. For example, a patient may not have the “textbook” presentation. Confirming a diagnosis based on the effects of treatment is also difficult given that a variety of orofacial pain conditions may respond well to the same treatment and that different treatments may be effective for the same condition (see chapters 18 and 19). When the working diagnosis remains the one with the highest probability, it is ruled as the final diagnosis unless proven otherwise.
The Clinical Assessment Process
The process of gathering evidence implies a reliance on proper strategies and procedures for data collection. As the clinician proceeds, the diagnostic space is likely to change and so will the focus of the assessment process. The assessment of the somatic, psychosocial, and behavioral aspects of the pain problem becomes invaluable when one considers that the site and source of the pain are not always the same, that tissue damage might be unnoticeable or absent, and that any state of pain has a psychologic and psychosocial impact. The clinical assessment process is usually divided into two distinct parts: (1) the appraisal of the chief complaint and the patient’s medical, dental, and psychosocial status (also called the comprehensive history), and (2) the clinical examination.
It is important also to point out that the diagnostic process is different for acute and chronic pain states. For instance, it is only necessary to establish a physical/somatic diagnosis for an acute pain condition such as a pulpitis. In cases of chronic pain, a physical as well as a psychosocial diagnosis is necessary because the pain has rarely any biologic value and is frequently accompanied by significant emotional distress and affective and cognitive disturbances that need to be addressed (see chapter 12).2,3 In that regard, the Graded Chronic Pain Scale4 is a good screening instrument for patients with chronic pain.
Comprehensive history
The comprehensive history constitutes the most important part of the diagnostic process. Taking the history is essential for establishing a good doctor-patient relationship, the prerequisite for successful management of the pain patient. In addition, several orofacial pain conditions lack specific signs, and their diagnosis relies on pain-related inclusion criteria that can be revealed only by the comprehensive history. The history should lead to a provisional or differential diagnosis; the clinical examination and additional tests then are needed to confirm or rule out the provisional diagnosis (Fig 17-2).
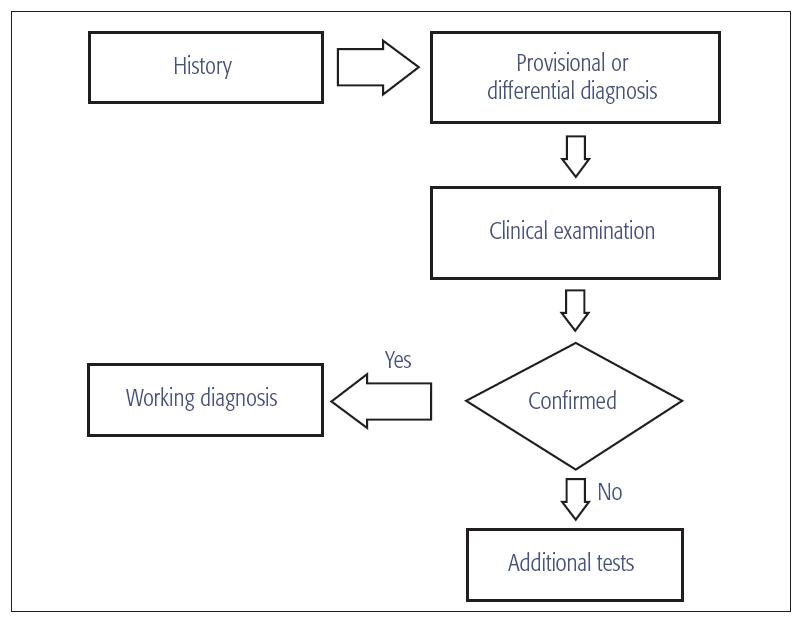
Fig 17-2 The diagnostic process.
Besides appraising the patient’s chief complaint, the comprehensive history helps put symptoms in the appropriate context. This is achieved through a well-organized and structured interview covering the reason the patient is seeking professional assistance, how the problem started, and how it has evolved. The clinician must inquire about localization, quality, duration, time course, triggering, worsening or relieving factors, and accompanying symptoms (Box 17-1). A careful pain description is important since several orofacial and headache conditions are diagnosed only upon specific pain features. The classic example is trigeminal neuralgia with its normal neurologic status, pain-free intervals, and characteristic waves of paroxysmal, brief electric shock–like pain with triggering factors, (see chapter 24). Because pain is a multidimensional experience, the patients must also be asked how the pain influences their emotional behavior (see also chapters 11 and 12).
| Box 17-1 Comprehensive pain description | |
| Intensity | On a 0 to 10 scale, how does your present pain rate? For chronic pain problems, how would you rate your average, minimum, and worst pain over the past month? |
| Location | Is the pain intraoral or extraoral; unilateral or bilateral; localized, regional, or diffuse? Does it involve one or more branches of the trigeminal territory? |
| Referral patterns | Where does the pain irradiate to? |
| Character | What does the pain feel like (eg, throbbing, shooting, stabbing, sharp, cramping, gnawing, hot/burning, aching, heavy, tender, splitting, tiring/exhausting, sickening, fearful, punishing/cruel, unbearable)? |
| Duration | How long does the pain last when it occurs (eg, seconds, minutes, hours, days)? |
| Frequency | How often does the pain occur (eg,/> |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



