Preventive Care
Learning Objectives
1 Pronounce, define, and spell the Key Terms.
2 Describe the goal of preventive dentistry.
3 Name the components of a comprehensive preventive program.
4 Explain the uses of systemic and topical fluoride in preventive dentistry.
5 Identify the recommended concentration of fluoride in community water.
6 Describe the role of plaque in dental caries and periodontal disease.
7 Describe the purpose of a disclosing agent.
8 Demonstrate providing personal oral hygiene instruction to a patient.
9 Teach a patient to brush and floss his or her teeth.
10 Describe the MyPlate concept.
11 Name the key nutrients and describe their primary functions.
12 Discuss the role of cariogenic foods in causing dental caries.
13 Explain the process of demineralization and remineralization of the teeth.
Key Terms
Active Learning
Calculus
Demineralization
Dental Decay
Disclosing Agent
Fluoride
Fluoride Varnish
Interdental Aids
MyPlate
Plaque
Plaque Control
Preventive Dentistry
Remineralization
Sodium Fluoride
Stannous Fluoride
Systemic Fluorides
Topical Fluorides
White spot
The goal of preventive dentistry is to achieve and maintain optimum oral health for a lifetime. Through a comprehensive oral health program and a partnership between the patient and dental professionals, optimum oral health can become a reality for everyone.
This chapter discusses the components of a comprehensive preventive dentistry program (Table 17-1).
TABLE 17-1
A Comprehensive Preventive Dentistry Program
| Preventive Measure | Description |
| Nutrition | Dietary counseling extends beyond the narrow scope of limiting sugar consumption and may include a discussion of nutrition from the standpoint of oral health and general health. |
| Patient education | Education motivates patients, provides them with information, and assists them in developing the skills necessary to practice good oral hygiene. |
| Plaque control | Daily removal of bacterial plaque from the teeth and adjacent oral tissue is the goal. |
| Fluoride therapy | Therapy includes professionally applied fluorides, at-home fluoride therapy, and consumption of fluoridated community water. |
| Sealants | Sealants are most frequently applied to difficult-to-clean occlusal surfaces of the teeth. Decay-causing bacteria are then prevented from reaching into occlusal pits and fissures. Chapter 18 discusses sealants. |
Process of Dental Disease
To effectively educate patients, you first must understand how dental diseases occur and how preventive dentistry is effective in reducing these occurrences.
Bacterial Dental Plaque
Bacterial dental plaque (often referred to as plaque) is a sticky, soft deposit of bacterial colonies that adhere to the teeth. Plaque forms on both supragingival and subgingival surfaces. The formation of plaque involves three basic steps (Table 17-2). (Supragingival plaque is above the gingival margin and subgingival plaque is below the gingival margin.) The bacteria found in plaque are the primary cause of dental caries and periodontal disease.
TABLE 17-2
Stages in the Formation of Plaque
| Stage | Description |
| Pellicle formation | The pellicle is a thin layer made up of glycoproteins from the saliva that forms over tooth surfaces and restorations. It re-forms on the teeth within minutes after brushing and/or polishing. It serves to keep the tooth surfaces moist and may even provide a barrier against acids in plaque. |
| Bacteria attach to the pellicle | Bacteria colonize within the pellicle and begin to grow and multiply and produce acids. Organisms in the first few hours are gram-positive cocci and rods (see Chapter 5). |
| Bacteria multiply and mature | The longer the plaque remains on the teeth, the greater the numbers and types of bacteria. Eventually Streptococcus mutans and Streptococcus sanguis dominate the colonies. These bacteria are primarily responsible for dental caries and periodontal disease. |
Dental Calculus
Dental calculus is mineralized bacterial plaque that forms a hard mass on the surface of the natural teeth, and on dentures and other dental prostheses. Calculus occurs at every age and on both permanent and primary teeth. Calculus plays an important role in periodontal disease. The rough surface of the subgingival calculus holds the disease-causing bacterial plaque close to the gingival tissue, continuing the inflamed state of the tissue.
It is important for the patient to understand the interrelationship between the removal of plaque, calculus, and good oral health.
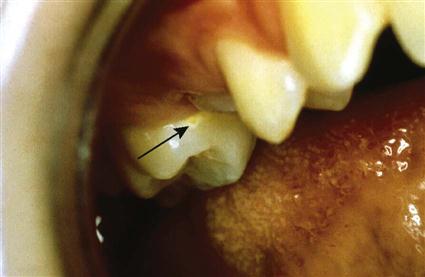
Dental Caries
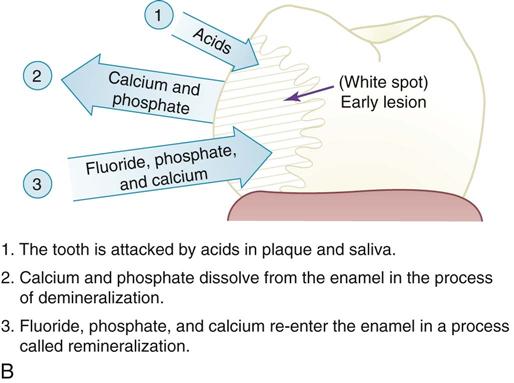
Dental caries, also known as dental decay, occurs when the bacteria in the plaque convert sugar from the foods we eat into acid. After a period of time, the acid attacks the tooth and causes demineralization (loss of calcium and phosphate) of the enamel. The earliest sign of demineralization appears as a white spot on the tooth (Figure 17-1, A). As plaque continues to attack the tooth, the areas of demineralization can turn into areas of caries (decay) (see Figure 17-1, B).
Periodontal Disease
Periodontal disease can range from gingivitis (inflammation of the gingivae) to extensive bone loss around the teeth (periodontitis). Dental plaque is the primary cause of periodontal diseases (Figure 17-2). Periodontal diseases are discussed in Chapter 24.
Tooth Brushing
Many different toothbrushes and brushing methods are in use today. The dental professional will assess the patient’s needs and recommend the toothbrush and brushing method best suited to the individual patient.
How Often to Brush
There is not a single answer when patients ask, “How often should I brush?” The answer is based on complete plaque removal rather than on the number of brushings.
To control bacterial plaque and to prevent halitosis (mouth odor), at least two brushings and flossings are recommended each day. Bacteria thrive in warm, moist, dark environments; therefore the mouth should be cleaned before going to bed at night. The longer the bacteria remain undisturbed, the more damaging the plaque becomes.
Toothbrush Selection
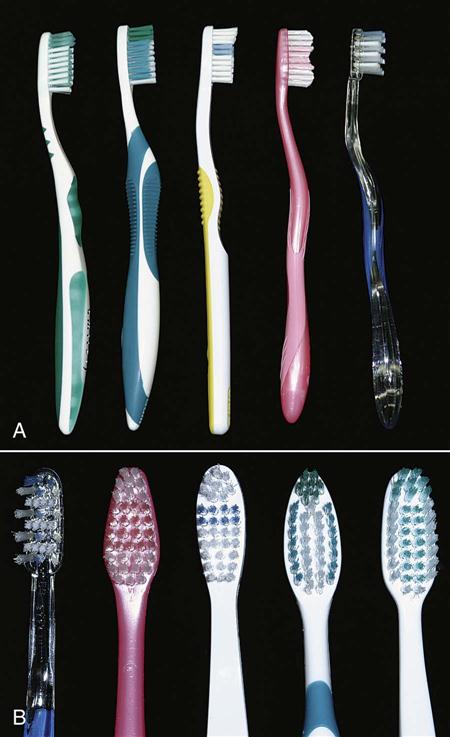
The size and style of the toothbrush are highly personal decisions. Many styles of head size, tuft shape, and handle angle and shape are available (Figure 17-3). It is generally recommended to use soft-bristled brushes. Soft bristles are less likely to cause damage to the soft tissue or any exposed cementum or dentin. Soft bristles also adapt to the contours of the tooth better. Toothbrushes should be replaced as soon as the bristles show signs of wear. Generally, this is every 8 to 12 weeks.
A powered toothbrush may be substituted for a manual toothbrush if the plaque is not removed with the manual brush. Suggest that the patient use a timer to ensure that adequate time is spent brushing. Powered toothbrushes are also useful for physically handicapped individuals who are unable to clean their teeth with a manual brush. They may be useful for a patient with orthodontic bands and brackets, and for some patients with periodontal problems.
Tooth Brushing Precaution
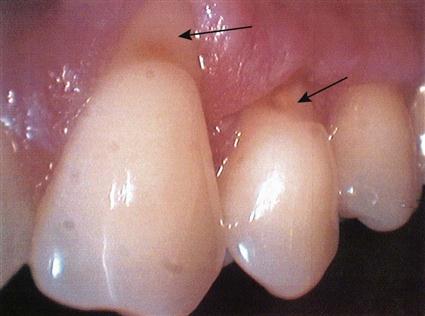
The patient should be cautioned about damage that may be caused by vigorously scrubbing the teeth. Over time, this may cause abnormal abrasion (wear) of the tooth structure, gingival recession, and exposure of the root surface (Figure 17-4).
Disclosing Agents
Because plaque is difficult to see, some people find it easier to learn tooth brushing and other plaque removal techniques with the aid of a disclosing agent. Disclosing agents temporarily color the plaque (usually red) to make it visible and therefore easier to remove (Figure 17-5).
Disclosing agents are artificially sweetened and may be candy-like tablets or may be formulated in a solution that is wiped over the teeth using a cotton-tip applicator. All ingredients in the tablet or solution are nontoxic and harmless if swallowed. However, they stain clothing, so be careful with their use (Box 17-1).
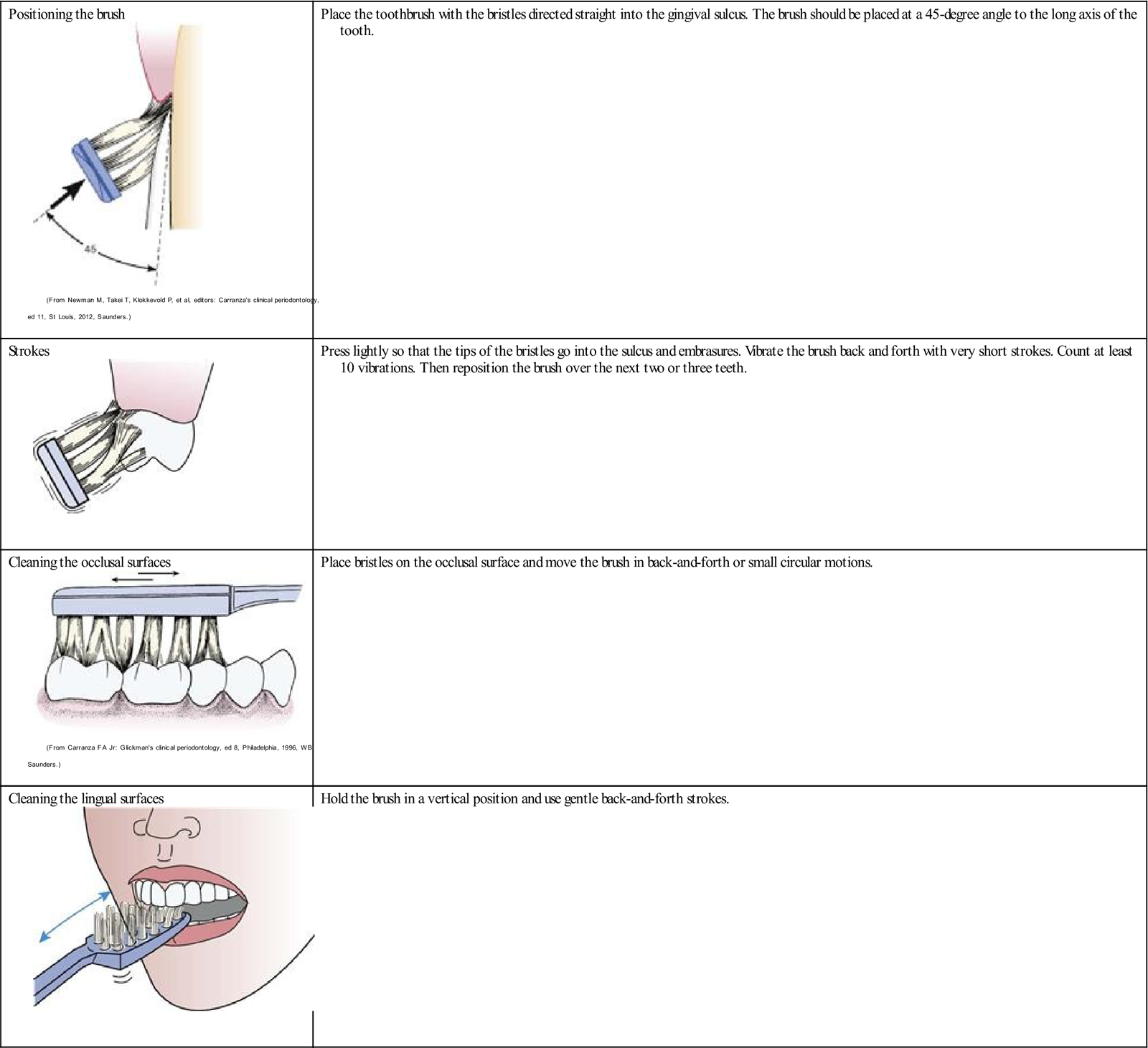
Bass Method of Sulcular Tooth Brushing
Several brushing techniques are commonly used. The Bass method (named after Dr. C. Bass, a pioneer in preventive dentistry) is the most commonly recommended technique (Table 17-3). This method is very effective in removing plaque directly beneath the gingival margin. The gingival margin is most important in controlling gingival inflammation.
TABLE 17-3
Bass Method of Sulcular Brushing
< ?comst?>
Positioning the brush
 |
Place the toothbrush with the bristles directed straight into the gingival sulcus. The brush should be placed at a 45-degree angle to the long axis of the tooth. |
Strokes
 |
Press lightly so that the tips of the bristles go into the sulcus and embrasures. Vibrate the brush back and forth with very short strokes. Count at least 10 vibrations. Then reposition the brush over the next two or three teeth. |
Cleaning the occlusal surfaces
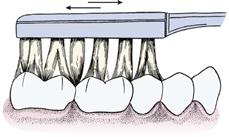 |
Place bristles on the occlusal surface and move the brush in back-and-forth or small circular motions. |
Cleaning the lingual surfaces
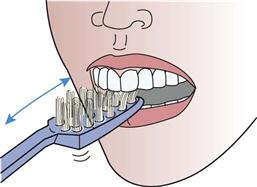 |
Hold the brush in a vertical position and use gentle back-and-forth strokes. |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Figure of positioning the toothbrush from Newman MG, et al: Carranza’s clinical periodontology, ed 11, St Louis, 2012, Saunders. Figures of cleaning occlusal and lingual surfaces from Carranza FA Jr: Glickman’s clinical periodontology, ed 8, Philadelphia, 1996, WB Saunders.
Note: Adding a rolling stroke after sulcular brushing modifies the Bass technique.
Brushing the Tongue
Bacteria on the tongue and tooth surfaces must also be removed by brushing. The easiest method is to place the toothbrush at the back of the tongue and sweep forward several times across the dorsum (top) of the tongue.
Care of the Toothbrush
When brushing is completed, the toothbrush should be thoroughly rinsed to remove excess water. The toothbrush should then be placed in a position with good air circulation to permit air-drying.
Flossing
Removing plaque from between the teeth is a critical part of good oral health. Dental floss is the most effective tool for most people to use in removing plaque from between the proximal surfaces of the teeth and in reducing interproximal bleeding.
Dental floss comes in several different types: waxed or unwaxed, thick or extra fine, or even in a tufted texture that change shape when tightened. Research has shown no difference in the effectiveness of waxed or unwaxed floss for removing plaque. It depends on how well the dental floss is used.
Dental floss is even available in various colors and flavors. However, colored and flavored dental flosses are no more effective in removing plaque, although they may motivate patients to floss more routinely (Figure 17-6).
The choice of dental floss is based on the patient’s manual skills, needs, and preferences (see Procedure 17-1).
Home Care Techniques
Once the patient is motivated to want to learn and use plaque control skills, he or she must learn how to do them correctly. The dental professional will work with the patient to develop a program of oral hygiene that the patient will follow routinely at home. The goal of the program is to thoroughly remove plaque at least once daily. After plaque has been thoroughly removed, it takes about 24 hours to form again. Many home care techniques are used for plaque removal; the technique selected must be based on the needs and abilities of the individual patient.
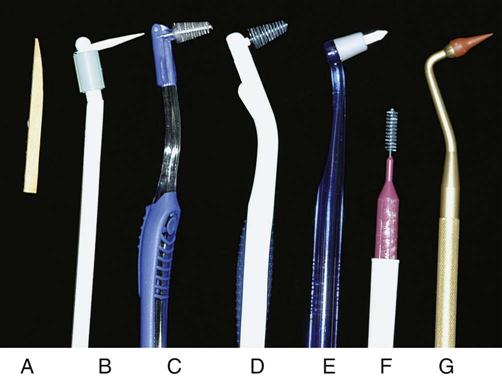
Special interdental aids are recommended for cleaning between teeth with large or open interdental spaces. These devices may be used in addition to dental floss but are not a substitute (Table 17-4 and Figure 17-7).
TABLE 17-4
Types of Self-Applied Fluorides
| Type | Form | Comments |
| Sodium fluoride (NaF) 0.24% | Dentifrices (gel or paste) | Approved by the American Dental Association (ADA) |
| Sodium monofluorophosphate (Na2PO3F) 0.76% | Dentifrices (gel or paste) | Approved by the ADA |
| Neutral sodium fluoride 0.025% | Mouth rinse | Sold over-the-counter without prescription |
| Neutral sodium fluoride 0.20% | Mouth rinse | Prescription required |
| Sodium fluoride (NaF) 1.1% | Brush-on gel | Not intended for use as a dentifrice; teeth must be brushed first, then gel used |
| Stannous fluoride (SnF2) 0.4% in glycerine base | Brush-on gel | Not intended for use as a dentifrice; teeth must be brushed first, then gel used |
Fluoride
Fluoride is a naturally occurring mineral that is found in many forms. It may be present in the water from wells; in the food we eat, which has absorbed fluoride from the soil; and as additives in many different products we use.
Fluorides are effective in strengthening the enamel’s resistance to dental decay. However, to achieve the maximum benefits of fluoride, an ongoing supply of both systemic and topical fluoride must be available throughout life (Box 17-2).
Systemic fluorides, also known as dietary fluorides, are those consumed in water, foods, beverages, or supplements.
Topical fluorides are applied directly to the teeth in the form of fluoridated toothpaste, fluoride mouth rinses, and topical applications (see Procedure 17-2).
Fluoride varnish is a concentrated topical fluoride within a resin or synthetic base that is painted on the teeth to prolong fluoride exposure. It can be used instead of a fluoride gel; two to three professional applications a year are effective in preventing decay (see Procedure 17-3).
Demineralization and Remineralization
Demineralization is loss of minerals (calcium, phosphorus, and fluoride), causing a breakdown of the enamel. Demineralization leads to a “white spot,” which is actually the early lesion, which with further demineralization will form caries (Figure 17-8).
When plaque is present, the teeth are exposed to tooth acid formed by bacteria within the plaque. These acid attacks cause demineralization. When fluoride is present in the outer layers of the enamel, the tooth is more resistant to demineralization.
Remineralization is the reverse process. Minerals are restored to the tooth surface that has been demineralized. When early remineralization occurs, the “white spot” hardens, and that area may even be harder than the enamel around it. However, if the carious lesion has progressed too far, remineralizaion cannot halt the process and the tooth must be restored by a dentist, or a toothache and possible loss of the tooth will result. Fluoride itself cannot remineralize tooth structure, but it does act as a catalyst to repair damaged enamel by using calcium, phosphorus, and fluoride from the saliva.
Safe Use of Fluoride
Fluorides added to the public water supply and present in dental products carry little or no risk when used as directed. Fluoride is beneficial in small amounts, but it can be harmful if instructions for use are not followed.
Long-term overexposure to fluoride, even at low concentrations, can result in dental fluorosis in children younger than 6 years with developing teeth. (Fluorosis appears as white spots on the teeth. These spots do not weaken the teeth and are primarily a cosmetic problem.)
Children should always be supervised when brushing or using fluoride rinses and should not be allowed to swallow fluoride toothpaste or fluoride rinses.
It is important for any dental professional responsible for the application of fluoride to know how much fluoride he or she is giving to patients.
Sources of Systemic Fluoride
Fluoridated Water
For over 40 years, fluoride has been safely added to the communal water supply. Most major cities in the United States are fluoridated, and efforts to fluoridate additional communities are ongoing.
In September 2010, the U.S. Department of Health and Human Services (DHHS) convened a panel of scientists from across the U.S. government to review new information related to fluoride intake and to develop new recommendations for community water fluoridation.
These scientists reviewed the best available information on prevalence and trends in dental caries, water intake in children in relation to outdoor air temperature, changes in the percentages of U.S. children and adults with dental fluorosis, and new assessments by the U.S. Environmental Protection Agency (EPA) that have examined cumulative sources of fluoride exposure and risks of children developing severe dental fluorosis.
This new information led DHHS to propose changing the recommended level for community water systems to 0.7 milligrams per liter.
Levels of fluoride in controlled water fluoridation are so low that there is no danger of ingesting an acutely toxic quantity of fluoride from fluoridated water. However, some communities have water that naturally contains more than twice the optimum level of fluoride. Prolonged exposure to these excessive amounts may cause dental fluorosis.
Other Dietary Sources
Foods and Beverages
Because many processed foods and beverages are prepared with fluoridated water, they must be considered as sources of die/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses