Infection Control Systems
LEARNING OUTCOMES
The administrative assistant generally has no direct patient contact. Nevertheless, he or she must understand both the risks and management of occupational exposures to blood-borne pathogens. Although his or her primary duties are in the business office, the administrative assistant may be called upon to perform some clinical task that could cause exposure to such a risk. The assigned job, therefore, does not make it impossible to contract a communicable disease. The role of the administrative assistant in infection control is vital, because it involves the following responsibilities:
• Acquiring a thorough understanding of the routes of disease transmission
• Verifying employee compliance with OSHA
• Maintaining employee records
• Scheduling continuing education courses for the staff
• Maintaining all Material Safety Data Sheets (MSDSs)
• Arranging for the disposal of hazardous waste
• Providing infection control training for new employees as designated by the employer
A variety of diseases can be transmitted by means of routine dental care. Fortunately the dental profession, through the American Dental Association (ADA), the Organization for Safety and Asepsis Procedures (OSAP) and the Centers for Disease Control and Prevention (CDC), has worked vigorously to establish infection control and safety procedures for the dental healthcare worker (DHCW) to prevent the transmission of disease.
The CDC report, Guidelines for Infection Control in Dental Health Care Settings, was revised in 2003. Every dental office should have direct access to these guidelines through a link on the ADA’s web site (www.ada.org) or the CDC’s web site (www.cdc.gov). This report consolidates previous recommendations and adds new ones for infection control in dental settings. It provides recommendations on: (1) educating and protecting dental healthcare personnel; (2) preventing the transmission of blood-borne pathogens; (3) hand hygiene; (4) PPE; (5) contact dermatitis and latex hypersensitivity; (6) sterilization and disinfection of patient care items; (7) environmental infection control; (8) dental unit water lines, biofilm, and water quality; and (9) special considerations (e.g., dental handpieces and other devices, radiology, parenteral medications, oral surgical procedures, and dental laboratories). These recommendations were developed in collaboration with and after review by authorities on infection control from the CDC and other public agencies, academia, and private and professional organizations.
DISEASE TRANSMISSION
Dental treatment involves several sources by which infectious diseases can be transmitted, including blood, saliva, nasal discharge, dust, hands, clothing, and hair. Any of these media can transmit a microbial or viral infection. Table 17-1 presents a list of several communicable diseases and their routes of transfer.
TABLE 17-1
Common Communicable Diseases and Routes of Transmission
| Disease | Medium of Transmission | Route of Transmission |
| Acquired immunodeficiency syndrome (AIDS) | Blood, semen, or other body fluids, including breast milk | Inoculation by use of contaminated needles or by direct contact so that infected body fluids can enter the body |
| Gonococcal disease | Lesions, discharge from infected mucous membranes | Direct contact, as in sexual intercourse; towels, bathtubs, toilets; hands of infected individuals soiled with their own discharges; through breaks in hands of attendant |
| Hepatitis B, viral | Blood and serum-derived fluids, including semen and vaginal fluids | Contact with blood and body fluids |
| Herpes | Cold sore; genital sores | Direct skin-to-skin contact as through kissing or sexual intercourse |
| Measles (rubella) | Discharges from nose and throat | Direct contact, hands of healthcare worker, articles used by and about patient |
| Mumps | Discharges from infected glands and throat | Direct contact with affected person |
| Pneumonia | Sputum and discharges from nose and throat | Direct contact, hands of health care worker, articles used by and about the patient |
| Rubeola | Secretions from nose and throat | Through mouth and nose |
| Streptococcal sore throat | Discharges from nose and throat, skin lesions | Through mouth and nose |
| Syphilis | Infected tissues, lesions, blood, transfer though placenta to fetus | Direct contact, kissing or sexual intercourse, contaminated needles and syringes |
| Tuberculosis | Saliva, lesions, feces | Direct contact, droplet infection from a person coughing with mouth uncovered, saliva transferred from mouth to fingers and then to food and other articles |
Types of Infections
Infections common to dental treatment generally can be divided into two categories, autogenous infections and cross infections. Autogenous infections are infections for which the patient is the source. For example, a patient who undergoes dental treatment, such as an extensive scaling procedure, may subsequently develop endocarditis; this condition can result from the introduction of virulent organisms (e.g., staphylococci or pneumococci) that live in the mouth and can be introduced into the bloodstream during the scaling procedure.
Cross infections are transferred from one patient or person to another. For example, when a child has an infection and coughs or sneezes, the caregiver may contract the infection through airborne or droplet transmission.
Routes of Infection Transmission
Microbial transmission through dental-related secretions and exudates occurs by three general routes: (1) direct contact with a lesion, organisms, or debris during intraoral procedures; (2) indirect contact through contaminated dental instruments, equipment, or records; and (3) inhalation of microorganisms aerosolized from a patient’s blood or saliva during the use of high-speed or ultrasonic equipment, such as a high-speed handpiece or an ultrasonic scaler.
In many dental practices, treatment providers may not realize the dissemination potential of saliva and blood by these routes. Potential dangers often are missed, because much of the spatter from the patient’s mouth is not readily noticeable. For example, bioburden (blood, saliva, exudate) may be transparent and may dry as a clear film on contaminated surfaces. Consequently the administrative assistant must understand the potential risk of handling contaminated surfaces.
INFECTION CONTROL IN THE DENTAL OFFICE
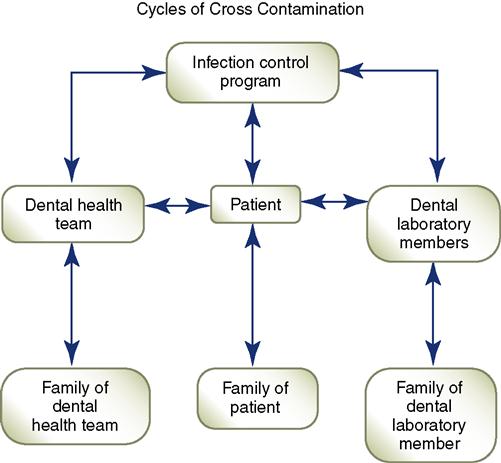
Because patient care actually begins in the business office, it is important to identify the role of the administrative assistant as it relates to infection control in the clinical area. Every dental healthcare worker is responsible for breaking the cycle of disease transmission (Figure 17-1). Safe practice is based on the following principles:
• A complete and accurate patient history must be obtained and screening must be done.
• Aseptic techniques must be observed using personal protective equipment.
• Healthcare workers must strictly adhere to acceptable sterilization procedures.
• Acceptable disinfection procedures must be practiced.
• Equipment asepsis and dental laboratory asepsis must be practiced.
The administrative assistant is responsible for the first step in safe practice, obtaining complete and detailed information about the patient. The records discussed in Chapter 7 must be completed, dated, signed, and reviewed thoroughly by the dentist. During treatment procedures, the administrative assistant must make sure that protocols are followed and the necessary barrier materials are available for use. Finally the administrative assistant ensures that the records used during the treatment procedure are transferred safely from the clinical site to the business office without cross contamination.
Table 17-2 presents several situations that the administrative assistant may encounter in attempting to maintain safe practice in the office. The administrative assistant must be able to distinguish between right actions and wrong actions and must understand the consequences of a wrong action in infection control. Box 17-1 presents a self-assessing list of points the administrative assistant should live by when working in the dental office to make sure that disease transmission is not being promoted.
TABLE 17-2
Recognizing Wrong from Right in Infection Control
| Wrong | Effect | Right |
| Shaking hands while wearing contaminated gloves | Disease transmission may occur during cross-contamination. | Remove gloves and wash hands prior to leaving examination gloves treatment room; nod and speak greetings to the individual. |
| Pulling mask on and off | Contact with the face with contaminated gloves can expose unprotected tissues to disease. If mask is contaminated, contact with gloved or ungloved hands will also allow disease transmission. | Always leave mask in place; if movement for repositioning is necessary, either do it with clean gloves or slight readjustment may be made by using the upper arm or shoulder. |
| Wearing the same mask for more than one patient | Masks become moist field, allowing penetration of particles through the mask. | Always change masks between patients and use more than one mask if treatment procedure is lengthy. |
| Reusing same gloves | Most gloves have microscopic openings allowing penetration of microbes. Washing gloves increases the potential for disease transmission. | Gloves are always changed between patients; gloves may need to be changed during a treatment procedure that is lengthy. |
| Placing patient records in treatment room | Records may become exposed to aerosols or through handling; these records are transferred to the business office after treatment, thus exposing the business personnel to the potential for disease. | Records other than radiographs should be kept outside the treatment room to avoid contamination. If the records must be in the treatment room, they should be kept out of reach of aerosols and handled with clean hands or with overgloves rather than examination gloves. |
| Storing instruments in trays or drawers instead of sealed bags in treatment rooms | Instruments not individually bagged (if not part of a tray set-up) may be exposed to aerosols or other contact during treatment and may become contaminated. | All instruments processed through sterilization should be bagged to ensure their sterility when used. Instruments, even in closed drawers, may not remain sterile. |
| Eating in the laboratory or other contaminated site | Surfaces can become contaminated from instruments or materials exposed to patient aerosols or handling. | A staff lounge or eating area must be available in a site away from potentially contaminated materials. |
| Wearing a V-neck laboratory coat | Garments under lab coat can become contaminated. If wearing a V-neck shirt underneath, skin will be exposed. | Always wear high neck lab coat when working with patients or in the laboratory. These coats should be removed before leaving the workplace. |
| Wearing dangling earrings, piercings, necklaces, bracelets and/or ties | Items can become contaminated. They may hang in the patient’s face or catch on something. | Minimize jewelry to only wearing wedding bands and small post earrings. |
Health Protection Program for the Dental Staff
The administrative assistant plays a role in maintaining the health and safety of the patients and healthcare workers in the office. Although not usually assigned the task of infection control coordinator, he or she should be familiar with the aspects of this process. After all, the administrative assistant is responsible for managing the office, and must be able to access all records.
The office’s personnel policy must include a health service program for the staff that covers the following:
• Exposure prevention and postexposure management
• Medical conditions, work-related illness, and work restrictions
• Allergies or sensitivities to work-related materials, such as latex
• Records maintenance, data management, and confidentiality issue
The administrative assistant and the dentist must work together to maintain the safety of all staff members and patients. Attention to records maintenance and continual education and training can ensure safe practice.
Government Regulations
All dental professionals are expected to comply with current guidelines and regulations governing infection control, hazard communication, and medical waste disposal. Several agencies are responsible for providing the dental professional with the current regulations affecting each of these areas. The employer is primarily responsible for maintaining current copies of all state and federal regulations that relate to the dental office. These guidelines must be reviewed, and their implementation in the office must be documented.
OSHA established guidelines to protect workers from occupational exposure to blood-borne diseases. Regulations now require that employees in direct contact with blood or infectious materials and substances are required to use standard precautions; that is, all patients must be treated as if they are potentially infectious with the human immunodeficiency virus (HIV), the hepatitis B virus (HBV), or other infectious diseases. An overview of the latest required OSHA standards is presented in Box 17-2.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Practice Note
Practice Note Practice Note
Practice Note Practice Note
Practice Note Practice Note
Practice Note Practice Note
Practice Note