Gilles J. Lavigne
Takafumi Kato
Pierre Mayer
Sleep is the natural process that cuts off conscious appreciation of the environment for a period of 6 to 9 hours (or longer for babies, children, and teenagers).1 Normally, sensory stimuli that are part of the environment, such as background noise or light touch, do not interrupt sleep.2 Rather, it is sudden or meaningful incoming information (such as an alarm clock) that usually triggers an arousal (brief brain, heart, and muscle activation [<10 s], without awareness) or an awakening (longer brain activation, with awareness of the environment).
It is important for clinicians to know that patients with orofacial pain are at risk for having poor sleep (ie, difficulty falling asleep or sleep that is interrupted by sudden onset of pain). Sleep is essential to health, and prolonged sleep deprivation increases the risk of cardiovascular and mental disorders or pain-related complaints.3 Chronic pain patients often wake up unrefreshed4–8 and frequently report long delays in falling asleep; insomnia is a common complaint, as is fatigue.4 The consequences of lack of sleep or poor sleep quality include daytime sleepiness, low productivity, and increased risk of work or motor vehicle accidents.4 This chapter will focus on the relationship between chronic pain and the mechanisms that maintain or disrupt sleep. Tools and methodological issues relevant to this topic can be reviewed in a recent publication from our group.9
Normal Sleep
When passing from wakefulness to sleep, there is a gradual change from full alertness and consciousness to drowsiness and a nearly complete disengagement from the environment. At sleep onset, a surprising sudden body jerk is often experienced. This type of myoclonus, the so-called hypnic jerk, is considered normal unless it recurs frequently during sleep. Scientists divide sleep into several stages that are classified as rapid eye movement (REM) and non-rapid eye movement (NREM) sleep stages. NREM sleep stages are divided into light sleep (stages 1 and 2) and deep sleep (stages 3 and 4, also known as slow-wave sleep or delta sleep). Sleep stages 3 and 4 are believed to be the “restorative sleep”; disruption of these stages seems to be associated with a higher risk of daytime fatigue and pain.4,7,9,10 REM sleep is also known as active sleep or paradoxical sleep. During sleep, we pass from light sleep to deep sleep to REM sleep from three to six times (ultradian cycles) during the night. Each of these cycles lasts approximately 90 minutes (Fig 16-1a). In the first half of the night, stages 3 and 4 are predominant. In the second half, REM sleep dominates.
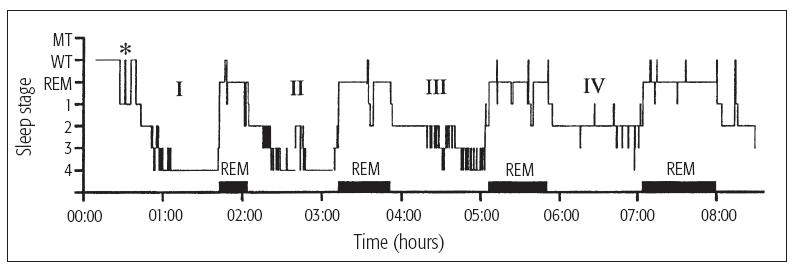
Fig 16-1a Good sleep: Data from a 23-year-old subject who had four full sleep cycles (I to IV). Only 12 sleep awakenings (thin vertical lines extending up to WT) were scored (normal < 30/night); one of the awakenings is depicted here, and in Fig 16-1b, by an asterisk. The duration of the REM periods (corresponding to the black horizontal bars) was longer and the duration of stages 3 and 4 was shorter toward the end of the sleep period. MT = movement time; WT = wake time.
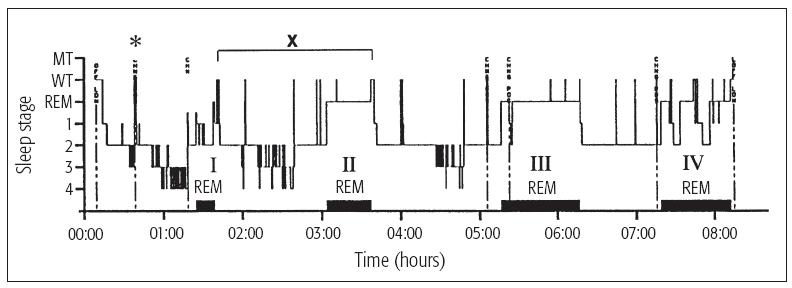
Fig 16-1b Poor sleep: Data from a 28-year-old subject who complained of unrefreshing sleep. Even though he presented four full sleep cycles (I to IV), several sleep awakenings (thin vertical lines extending up to WT) were scored (n = 27) and frequent sleep-stage shifts were noted (X). REM periods correspond to the black horizontal bars. MT = movement time; WT = wake time.
Specific criteria are used to score various sleep stages from polygraphic recordings with dedicated software (Table 16-1 and Fig 16-2). The following recordings are used: brain electric (electroenceph-alographic [EEG]) activity, muscle (electromyographic [EMG]) activity, eye movements (electro-oculogram [EOG]), heart rate (electrocardiogram [ECG]), and respiration (chest and abdominal movements and oronasal airflow).4,9–13 Measurements of rectal temperature and salivary melatonin levels are taken to assess chronobiologic rhythms. Other measurements include esophageal acidity for gastric reflux and blood endocrine levels. Video and sound recordings are also used to identify body movements that occur during sleep, including bruxism, periodic limb movement, somnambulism, snoring, talking, and REM behavior disorder (absence of body paralysis during sleep).9
| Table 16-1 Awake and sleep stage recognition* | ||||||
| Stage | Sleep time (%) | EEG/brain activity | EMG activity | EOG/eye movement | ECG/ heart rate |
Arousal probability |
| Awake | – | Low-amplitude high frequency β (13–30 Hz) and α (8–12 Hz) waves | High | Intens | Variable | – |
| NREM Light sleep Stage 1 | 10 | Low-amplitude high-frequency and mixed-frequency of fast and desynchronized α (10–12 Hz) and θ (4–7.5 Hz) waves | High moderate* | Slow rolling | Slower than awake | Very high |
| Stage 2 | 50 | Mid-amplitude slower α(8–10 Hz) and θ (4–7.5 Hz) waves with presence of K-complexes† and EEG spindles‡ | Moderate* | Slow | Slower than awake | High |
| NREM Deep sleep Stages 3 and 4 | 10–20 | High-amplitude low-frequency δ (0.5–3.5 Hz) waves | Moderate to low | Absent | Slowest and regular | Low |
| REM/active sleep | 20–25 | High-frequency and mixed-frequency desynchronized pattern (absence of δ waves) | Very low/hypotonia |
Stay updated, free dental videos. Join our Telegram channel
VIDEdental - Online dental courses
 Get VIDEdental app for watching clinical videos
Get VIDEdental app for watching clinical videos

| ||
