16
Medical disability
M.T. Hosey and R. Welbury
Chapter contents
16.1.2 The general examination
16.2.1 Congenital heart disease
16.2.2 Acquired cardiovascular disease
16.2.3 Dental care for children with cardiovascular disorders
16.3.2 Dental management of bleeding disorders
16.6 Metabolic and endocrine disorders
16.7.1 Dental management of children with cancer
16.8.1 Pre-transplant treatment planning
16.8.2 Immediate post-transplant period
16.8.3 Stable post-transplant period
16.1 Introduction
There are many general medical conditions that can directly affect the provision of dental care and some where the consequences of dental disease, or even dental treatment, can be life-threatening. The increasing number of children who now survive with complex medical problems because of improvements in medical care present difficulties in oral management. Dental disease can have grave consequences and so rigorous prevention is paramount. The decline in childhood mortality has led to increasing emphasis on maintaining and enhancing the quality of the child’s life and ensuring that children reach adult life as physically, intellectually, and emotionally healthy as possible. Dental care can play an important part in enhancing this quality of life. Indeed, management within the primary dental services helps to ‘normalize’ life for these children who appreciate attending along with their family even though sometimes they might still require specialist expertise.
Even though infant mortality rates (deaths under 1 year of age) have declined dramatically in the UK, death rates are still higher in the first year of life than in any other single year below the ages of 55 in males and 60 in females. The rates are highest for the very young. The main causes of death in the neonatal period (the first 4 weeks of life) are associated with prematurity (over 40%) and congenital malformations (30%). However, in the remainder of the first year the main causes of death occur at home and often nothing abnormal or suspicious is found (SUDI (sudden unexpected death in infancy) and SIDS (sudden infant death syndrome)). Although the unexpected death of a child over 1 year of age is rare, a few infants still succumb to respiratory and other infective diseases (e.g. meningitis), congenital malformations, and accidents. (See Key Points 16.1.)
16.1.1 The medical history
All patients should have an accurate medical history taken before any dental treatment is undertaken. This is important for several reasons.
1. To identify any medical problems that might require modification of dental treatment.
2. To prioritize children who require intensive preventive dental care.
3. To identify those requiring prophylactic antibiotic cover for potentially septic dental procedures.
4. To check whether the child is receiving any medication that could result in adverse interaction(s) with drugs or treatment administered by the dentist. This would include past medication that could have had an effect on dental development.
5. To identify systemic disease that could affect other patients or dental personnel. This is usually related to cross-infection potential.
6. To establish good rapport and effective communication with the child and their parents.
7. To determine the family and social circumstances, whether other siblings are affected by the same or similar condition, and the ability of the parents to cope with attendance for dental appointments given the added burden of medical appointments and their wish to ensure adequate continued schooling.
8. To facilitate communication with medical colleagues.
9. To satisfy medico-legal requirements.
Many dental practitioners use standard questionnaires to obtain a medical history. It has been found that one of the most effective methods is to use a questionnaire followed by a pertinent personal interview with the child and their parent or guardian. (See Key Points 16.2.)
16.1.2 The general examination
General observation of the child is invaluable and can provide vital information. The child’s demeanour is important in assessing their potential cooperation for dental treatment, but assessment of general outward appearance can also be helpful in determining their state of health. An impression of height (are they as tall as their peers?) and weight (undernourished or obese?) can give clues about not only nutrition but also somatic growth and dental development. Visually accessible areas, such as skin and nails, can reveal cyanosis, jaundice, and petechiae from bleeding disorders. The hands are particularly worthy of inspection, and can show alterations in the finger-nails such as finger-clubbing from chronic cardiopulmonary disorders as well as infections and splinter haemorrhages. Overall shape and symmetry of the face may be significant, and there may be characteristic faces that are diagnostic of some congenital abnormalities and syndromes.
16.2 Cardiovascular disorders
These can be divided into two main groups: congenital heart disease (existing before or at birth), and those disorders that are acquired after birth. Congenital heart disease occurs in approximately eight children in every 1000 live births. There is a wide spectrum of severity, but two or three of these children will be symptomatic in the first year of life.
16.2.1 Congenital heart disease
The cause is rarely known in individual cases but multifactorial inheritance patterns are mainly responsible. Several chromosomal abnormalities, such as Down syndrome, are associated with severe congenital heart disease, but these represent fewer than 5% of the total. The main types of congenital condition are shown in Table 16.1. In most instances there is a combination of genetic and environmental influences, including infections, during the second month of pregnancy.
Many defects are slight and cause little disability, but a child with more severe defects may present with breathlessness on exertion, tire easily, and suffer from recurrent respiratory infections. Those children with severe defects such as tetralogy of Fallot and valvular defects, including pulmonary atresia and tricuspid atresia, will have cyanosis and finger-clubbing, and may have delayed growth and development (Figs 16.1–16.3). Characteristically, these children will assume a squatting position to relieve their dyspnoea (breathlessness) on exertion.
Heart murmurs
The incidence of congenital heart disease is falling, affecting 7–8 infants per 1000. Many parents will report that their child either has, or had, a ‘heart murmur’. These may only be discovered at a routine examination, although they occur in over 30% of all children. Most of these murmurs are functional or innocent, and are not associated with significant abnormalities but are the result of normal blood turbulence within the heart. Innocent murmurs are heard most frequently from 3 to 7 years of age. In a small minority of cases a heart murmur indicates the presence of a cardiac abnormality causing the turbulence. If the dentist is in any doubt about the significance of a murmur, a cardiological opinion should be sought. Normally, contact with the child’s medical practitioner will clarify the situation. Innocent murmurs do not require any special precautions or treatment.
Table 16.1 Prevalence of congenital cardiac disease
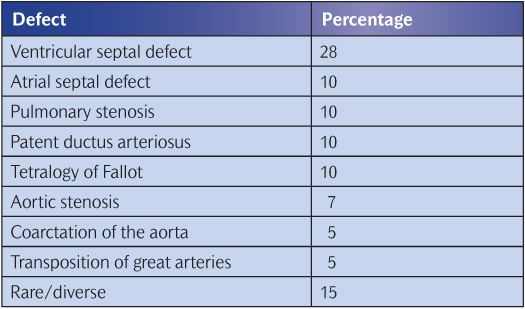
Figure 16.1 The fingers of a boy with Down syndrome and tetralogy of Fallot. The cyanosis and finger-clubbing associated with his severe cardiac disease are obvious.
Figure 16.2 Cyanosis affecting the lips in a boy with tetralogy of Fallot. The mucous membranes appear bluish.
Figure 16.3 Central cyanosis affecting the tongue of the boy shown in Fig. 16.2.
Ventricular septal defects (VSDs)
VSDs are the most common of the cardiac malformations. Small defects are asymptomatic and may be found during a routine physical examination. Large defects with excessive pulmonary blood flow are responsible for symptoms of breathlessness, feeding difficulties, and poor growth. Between 30% and 50% of the small defects close spontaneously, usually within the first year of life. Larger defects are usually closed surgically in the second year of life, but defects involving other cardiac structures may require complex surgery or even transplantation.
Atrial septal defects (ASDs)
ASDs are not as common as VSDs in children, but are proportionately more significant in adults and more frequent in females. An isolated patent foramen ovale is of no clinical significance and is not considered to be an ASD. Even an extremely large ASD rarely produces heart failure in children, but symptoms usually appear in the third decade. Surgery is usually carried out before school age.
Pulmonary stenosis
There are usually no symptoms with mild to moderate stenosis of the pulmonary valve, but exercise intolerance and cyanosis may occur if this is severe. Treatment is required for the moderate to severe forms; in the majority of children relief of this obstruction is now carried out by balloon dilatation rather than surgery.
Patent ductus arteriosus
During fetal life most of the pulmonary arterial blood is shunted through the ductus arteriosus into the aorta, thus bypassing the lungs. Functional closure of the ductus arteriosus usually occurs at birth. Virtually all preterm babies weighing less than 1.75kg have a patent ductus arteriosus in the first 24 hours of life, but this usually closes spontaneously. Ductus arteriosus patency is mediated by pros-taglandins, and the administration of inhibitors of prostaglandin synthesis, such as indometacin, is effective in closing the ductus in a significant number of babies. However, surgical ligation is a safe and effective back-up if indometacin is contraindicated or has not been successful.
Tetralogy of Fallot
This classically consists of a combination of:
• an obstruction of right ventricular outflow (pulmonary stenosis)
• VSD
• dextroposition of the aorta (its origin may be overlying the VSD)
• right ventricular hypertrophy.
Cyanosis is one of the most obvious signs of this condition, but it may not be present at birth. However, as the child grows, the obstruction to blood flow is further exaggerated. The oral mucous membranes and nailbeds are often the first places to show signs of cyanosis. Growth and development may be markedly delayed in severe untreated tetralogy of Fallot, and puberty is delayed. Early medical management involves the use of prostaglandins so that adequate pulmonary blood flow can occur until surgical intervention can be carried out. Initially, a shunt procedure (usually the Blalock–Taussig shunt) is performed to anastomose the subclavian artery to the homolateral branch of the pulmonary artery. Later in childhood, total surgical correction is undertaken, but the mortality rate from this procedure is 5–10%.
16.2.2 Acquired cardiovascular disease
Rheumatic fever
Rheumatic fever follows a group A streptococcal infection of the upper respiratory tract, especially in developing countries, and may occur at all ages but usually between 5 and 15 years. Environmental factors, such as overcrowding, promote the transmission of streptococcal infections, and the incidence of rheumatic fever is higher among lower socio-economic groups. The clinical onset is usually acute and occurs 2–3 weeks after a sore throat. Joint pains are common and of a characteristic migratory polyarthralgia or polyarthritis. Carditis is the most serious manifestation, occurring in 40–50% of initial attacks, especially in young children. Fever is usually present, but in an insidious onset of the condition it may be low grade. Most of the carditis resolves, except the lesions on the cusps of the heart valves which become fibrosed and stenotic. Rheumatic heart disease is the most important manifestation of rheumatic fever and may affect the mitral, aortic, tricuspid, and pulmonary valves.
Diseases of the myocardium and pericardium
Major diseases involving the myocardium and pericardium include bacterial infections such as diphtheria and typhoid, tuberculous, fungal, and parasitic infections, rheumatoid arthritis, systemic lupus erythematosus, uraemia, thalassaemia, hyperthyroidism, neuromuscular diseases such as muscular dystrophy, and glycogen storage diseases. They are relatively rare in children in developed countries.
Other cardiovascular problems
There are several other important conditions that are common in adults but not in children. These include coronary artery disease (ischaemic heart disease), cardiac arrhythmias, and hypertension. In children, secondary hypertension is more common than essential hypertension and is associated with renal abnormalities in 75–80% of those affected.
16.2.3 Dental care for children with cardiovascular disorders
The most important consideration in planning dental care for children with cardiovascular disorders is the prevention of dental disease. As soon as a child is diagnosed as having a significant cardiac problem, they should be referred for dental evaluation and an aggressive preventive regimen, including dietary counselling, fluoride therapy, fissure sealants, and oral hygiene instruction, should be commenced. Regular monitoring, both clinical and radiographic, with reinforcement of the preventive advice is essential. Active dental disease should be treated before cardiac surgery is undertaken.
Antibiotic prophylaxis
Guidance from the National Institute for Health and Clinical Excellence (NICE) in the UK (NICE 2008) has shown that antibiotic prophylaxis is not effective in preventing infective endocarditis and there is no clear association between episodes of infective endocarditis and interventional procedures. Any benefits from prophylaxis need to be weighed against the risks of adverse effects for the patient and the development of antibiotic resistance. As a result, NICE recommends that antibiotic prophylaxis is no longer routinely offered for defined dental interventional procedures.
Adults and children with the following structural cardiac conditions are considered to be at risk of infective endocarditis:
• aquired valvular heart disease with stenosis or regurgitation;
• valve replacement;
• structural congenital heart disease, including surgically corrected or palliated structural conditions, but excluding isolated ASD, fully repaired VSD, or fully repaired ductus arteriosus, and closure devices that are judged to be endothelialized;
• hypertrophic cardiomyopathy;
• previous infective endocarditis.
NICE makes the following recommendations:
Advice
Offer people at risk of infective endocarditis clear and consistent information about prevention, including:
• the benefits and risks of antibiotic prophylaxis, and an explanation of why antibiotic prophylaxis is no longer routinely recommended;
• the importance of maintaining good oral health;
• symptoms that may indicate infective endocarditis and when to seek expert advice;
• the risks of undergoing invasive procedures, including non-medical procedures such as body piercing or tattooing.
When to offer prophylaxis
• Do not offer antibiotic prophylaxis against infective endocarditis to people undergoing dental procedures.
• Do not offer chlorhexidine mouthwash as prophylaxis against infective endocarditis to people at risk undergoing dental procedures.
Managing infection
• Investigate and treat promptly any episodes of infection in people at risk of infective endocarditis to reduce the risk of endocarditis developing.
• Favour more radical treatments to avoid potential sources of infection (e.g. extraction rather than pulp therapy).
Treatment planning
If the child and parent(s) are seen in infancy and effective preventive dental procedures are instituted, in theory operative dentistry should be unnecessary. In practice, the situation may be very different. Ideally, treatment in children should be carried out during short appointments so that cooperation is maximized. Other problems in these children may include prolonged bleeding following scaling or surgical procedures due to thrombocytopenia and anticoagulant medication. It is essential to check the platelet count and prothrombin time if dental extractions are planned. The patient’s prothrombin time is compared with the normal value, and the ratio is called the international normalized ratio (INR). No child with symptomatic cardiac problems should have any routine dental procedures until details of the condition have been obtained and the patient’s physician consulted.
Antibacterial prophylaxis recommendations are constantly updated and current guidance is based on NICE recommendations and revised as new scientific evidence and drugs become available. The latest British Cardiac Society guidelines and the British National Formulary should be checked.
16.3 Disorders of the blood
16.3.1 Bleeding disorders
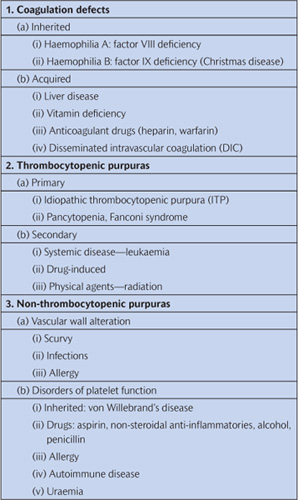
The blood is in a dynamic equilibrium between fluidity and coagulation, but the haemostatic mechanism is more complex than just alterations in this equilibrium. It involves local reactions of the blood vessels, platelet activities, and the interaction of specific coagulation factors that circulate in the blood. In early childhood many of the bleeding disorders have a genetic background, but with increasing age more become iatrogenic—usually due to anticoagulant medication. Patients who have had cardiac surgery for some congenital abnormality, those who have had a recent myocardial infarction, and those who have had cerebrovascular accidents may all be receiving long-term anticoagulant therapy. Table 16.2 gives a classification of bleeding disorders based on disorders of coagulation, bleeding problems due to decreased numbers of platelets, and disorders of bleeding where there are normal numbers of platelets. Many of these conditions are very rare and will not be considered further.
Haemophilia
Haemophilia A is an X-linked recessively inherited condition caused by a deficiency of factor VIII. The degree of severity is very varied but tends to be consistent within the same family. Children with over 25% of normal levels of circulating factor VIII can lead normal lives, those with between 1% and 5% are moderately to severely affected by minor trauma, etc., while those with under 1% have multiple bleeds into joints (haemarthroses) and may be severely physically handicapped as a result. Obviously, prevention of trauma to those who have this condition is extremely important, but the availability of factor VIII concentrates has revolutionized the quality of life of haemophiliacs. Unfortunately, in the past some of these blood replacement products have been contaminated with hepatitis, human immunodeficiency virus (HIV) and Creutzfeldt–Jakob disease (CJD), and therefore cross-infection control is a high priority. It was found that a number of patients who were thought to be haemophiliacs did not respond to replacement with factor VIII (anti-haemophiliac globulin) but were deficient in another factor—factor IX. This is known as Christmas disease or haemophilia B. This is also transmitted as an X-linked recessive trait with a wide range of clinical severity, but female carriers of this condition also have a tendency to bleed. (See Key Points 16.3.)
Table 16.2 Classification of bleeding disorders
von Willebrand’s disease
This is a dominantly inherited, complex, and variable condition characterized by a vascular abnormality of large irregular capillaries, defective platelets that do not adhere to each other, and decreased levels of factor VIII. Common clinical manifestations are nosebleeds and spontaneous gingival haemorrhage. von Willebrand’s disease is the most common inherited bleeding disorder, affecting one in every 1000 individuals in the USA and the UK.
Thrombocytopenia
Thrombocytopenia is caused by a reduction in the number of circulating platelets in the bloodstream. Normal levels are 150–400×109/L. The platelet count should be at least 50×109/L before surgery is attempted and continuous infusion of platelets may be required. Clinical signs are petechial haemorrhages into the skin and mucou/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Key Points 16.1
Key Points 16.1 Key Points 16.2
Key Points 16.2


 Key Points 16.3
Key Points 16.3