15
Vertical Root Fractures: Radiological Diagnosis
Introduction: Vertical Root Fracture (VRF) Incidence and Consequences
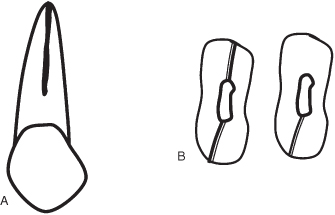
A true VRF is a longitudinal fracture confined to the root that usually initiates on the internal canal wall and extends toward the root surface (Figure 15.1). This is different from a cracked tooth, in which the tooth’s structural discontinuity is incomplete in nature. A crack usually runs mesiodistally from the occlusal surface toward the cervical aspect of the tooth and eventually progresses apically to the root (“split root”). The incidence of VRF is more commonly found in endodontically treated teeth (Pitts et al., 1983; Yang et al., 1995), though it has been reported in nonendodontically treated teeth with intact crowns and no/minimal restoration (Chan et al., 1998; Yeh, 1997). Clinically, VRF in teeth is most commonly found in the buccolingual direction. The mesiodistal fractures of the root are considered less common. It may involve the whole length of the root or a portion of the root in the sagittal plane. Along the cross-sectional plane, it may be complete (extending from the facial/lingual surface and includes the root canal wall) or incomplete (initiating from the root canal or the external surface but not involving the opposite surface). Most VRFs are complete in nature (Walton et al., 1984).
Figure 15.1 Schematic diagram showing the extension of vertical root fracture (a) in the apical to coronal direction on the buccal surface, and (b) complete and incomplete vertical root fracture in the cross-sectional plane.
The prevalence of VRF has not been well established to date. Different clinical surveys and follow-ups of endodontically treated teeth suggest a prevalence of 2% and 5% (Bergman et al., 1989; Morfis, 1990; Moule and Kahler, 1999; Testori et al., 1993; Torbjorner et al., 1995). However, determining the prevalence of VRF from studies primarily conducted to examine the causes of extraction of endodontically treated teeth may be erroneous. Some VRF cases in these studies could be diagnosed mistakenly as root canal treatment failure or progressive periodontal disease (Tamse et al., 2006). Interestingly, a prevalence of 11% and 20% was reported in root-filled teeth that were referred for extraction (Fuss et al., 1999; Coppens, 2003). This inconsistency in the reported prevalence may be attributed to the difficulty in diagnosing VRF. Diagnosis of VRF is a difficult and challenging experience for clinicians. The current methods used to diagnose VRF are transillumination, radiographs, periodontal probing, staining, surgical exploration, bite test, direct visual examination, and examination with operative-microscope. However, all these methods have limited success in clinical diagnosis. Evidence-based findings concerning the diagnostic accuracy and effectiveness of clinical and radiographic assessments for the diagnosis of VRF are lacking (Tsesis et al., 2010). There is often no single clinical feature that indicates the presence of VRF; and most of these signs/symptoms may be related with pulpal necrosis or failing root canal therapy. For that reason, those signs and symptoms, although helpful in arriving at a diagnosis of VRF, are generally not sufficient to diagnose VRF. In a study conducted on 92 endodontically treated teeth, it was concluded that general practitioners correctly diagnosed VRF in only 31% of the cases (Tamse et al., 1999a).
Identification of the teeth or roots that are susceptible to fracture is very important. A complete history and clinical examination of the susceptible tooth is mandatory. During clinical examination, periodontal probing is recommended to detect any osseous defects, especially on the buccal aspect of the root. Deep probing in two positions on opposite sides is almost pathognomonic for the presence of VRF. These sinus tracts are located close to the gingival margin in teeth associated with VRF, opposed to the sinus tracts in failed root canal-treated teeth that are generally located more apically. A sinogram may be useful to trace the sinus tract parallel to the periodontal space. The possibility of fracture is high if the pocket extends to the mid-root level rather than to the root apex. The presence of two sinus tracts at both buccal and lingual sides strongly suggests VRF (Moule and Kahler, 1999; Pitts et al., 1983). An in vitro study evaluated the accuracy of three electronic apex locators (Root ZX, Foramatron D10, and Apex NRG) for the detection of simulated horizontal and VRFs. Based on this study, it was concluded that the three electronic apex locators tested were accurate and acceptable in detecting horizontal root fractures. However, they were unreliable in detecting the positions of VRFs (Ebrahim et al., 2006). Inspection of VRF, either by nonsurgical or surgical procedures, is a useful step for the absolute confirmation of the diagnosis. Undiagnosed VRF may lead to perplexing clinical situations and inappropriate endodontic treatment.
Mechanisms and Risk Factors for VRF
VRF in teeth is unpredictable and is considered to be due to multifactorial causes. It is imperative to realize that most of the time, one factor does not always result in increased fracture susceptibility. Instead, many factors interact to influence the susceptibility of a tooth to fracture. Yet at a given time, any one factor can easily predominate over the rest. The factors that predispose teeth to VRF can be categorized as (1) non-iatrogenic and (2) iatrogenic causes (Kishen, 2006).
Non-Iatrogenic Causes
A tooth structure, during chewing, flexes and subsequently experiences bending stress distribution (Kishen and Asundi, 2002). Significant loss of healthy dentin structure due to the disease process or trauma and the presence of anatomical variations may significantly alter the functional stress distribution within the remaining tooth structure, increasing its predilection to VRF. Anatomical variations such as narrow mesiodistal root width and severe root curvature are reported to be risk factors for VRF in non-endodontically treated posterior teeth in a Chinese population (Chan et al., 1998; Yeh, 1997). Age changes in dentin are also considered as a risk factor that increases fracture predilection in teeth. Alteration of normal dentin to form transparent dentin is a common age-induced process. The dentinal tubules in transparent dentin are gradually filled up with minerals over time, beginning at the apical end of the root and often extending into the coronal dentin. The fracture toughness in transparent dentin is approximately 20% lower and their stress–strain response is characteristic of brittle material (Kinney et al., 2005). It has been reported that the tensile strength of aged dentin is lower than young dentin (Tonami and Takahashi, 1997). Hence, endodontic or restorative procedures in aged individuals might require modification to accommodate the reduced fracture toughness of dentin tissue. Abnormal parafunctional habits such as bruxisms, clenching of teeth, or chewing on hard objects, may generate large forces on the tooth surfaces. This may also contribute to microcracking in dentin and tooth fracture at a later date. Destructive parafunctional habits have been reported to be a cause of VRF in teeth with vital pulp (Cohen et al., 2003).
Iatrogenic Factors
Root Canal Treatment Procedures
The ultimate strength of a tooth is directly related to the amount of remaining tooth structure. Therefore, preservation of the tooth structure is very crucial in the successful management of structurally compromised teeth. The stress distribution pattern in post-core restored, root-filled teeth is distinctly dissimilar to that of an intact tooth. Excessive removal of healthy dentin during root canal enlargement, especially in curved and narrow roots, is one of the important predisposing factors for VRF (Kishen, 2006). Endodontic procedural errors that create sharp notches or crack(s) on the root canal wall would lead to a localized increase in stress concentrations, which could predispose the root to VRF. Unfortunately, access cavity preparation by itself compromises the mechanical integrity offered by the roof of the pulp chamber. Any compromise in the mechanical integrity offered by the roof of the pulp chamber would allow greater flexure of the tooth during function (Gutmann, 1992). Endodontic procedures have been shown to reduce the relative tooth stiffness by 5%. However, this value is less than that of an occlusal cavity preparation, which reduces the relative tooth stiffness by 20%. The largest loss in stiffness was associated with the loss of marginal ridge integrity and mesio-occluso-distal cavity preparation, which resulted in 63% loss of relative tooth stiffness (Reeh et al., 1989).
Many studies have highlighted the deleterious effects of endodontic irrigants and medicaments on the mechanical properties of dentin. Sodium hypochlorite is a very reactive chemical, and when applied in high concentration for a long period, along with its desired therapeutic effects, produces undesired effects on the root dentin. There have been several reports of the adverse effects of sodium hypochlorite on the physical properties of dentin such as flexural strength, elastic modulus, and microhardness (Goldsmith et al., 2002; Grigoratos et al., 2001). Ethylenediaminetetraacetic acid (EDTA) is also an endodontic irrigant utilized to remove the smear layer formed after root canal preparation. The microhardness of root canal dentin irrigated with 5.25% NaOCl, 2.5% NaOCl, 3% H2O2, 17% EDTA, and 0.2% chlorhexidine gluconate for 15 minutes each was studied. Except for chlorhexidine, all irrigants were found to reduce the surface hardness of the dentin. Mechanical testing of dentin specimens treated with calcium hydroxide, mineral trioxide aggregate, and sodium hypochlorite for 5 weeks demonstrated a 32% mean decrease in the strength, while calcium hydroxide treatment produced a 33% decrease (Calt and Serper, 2002). The chemically affected radicular dentin can be a potential source for microcracking, and subsequent fatigue failures. Obturation techniques that generate heavy apical forces, such as lateral condensation, may also predispose the tooth to VRF (Holcomb et al., 1987). Clinically, it should be noted that the risk of VRF increases from the beginning of endodontic therapy. In endodontically treated teeth, the average time between root filling and the appearance of a VRF has been estimated to be between 39 months (Meister et al., 1980) and 52.5 months (Gher et al., 1987), with a range of 3 days to 14 years.
Restorative Treatment Procedures
In restored root-filled teeth, the mismatch between the elastic modulus of the post-core crown system and the remaining tooth structure would lead to altered stress distribution patterns, which in turn may predispose the tooth to fracture. Generally, the anatomy of the tooth, shape and stiffness of post, length of the post within the root canal, direction and magnitude of external forces, and the amount of remaining tooth structure will determine the nature and pattern of the final tooth fracture (Kishen, 2006). Excessive post space preparation leaving behind thin dentin walls, improper selection of post, excessive pressure application during intracanal restorations or cementation, and poor tooth selection as a fixed bridge abutment may all influence the susceptibility of teeth to VRF (Tjan and Whang, 1985).
Different studies have highlighted the dangers of using tapered cast-posts (Isidor and Brondum, 1992; Isidor et al., 1996). Although it is believed that the parallel-sided posts can distribute functional loads passively to the remaining tooth structure (Cooney et al., 1986; Sahafi et al., 2004), some studies have observed only minimal advantages with the parallel-sided posts when compared to the tapered posts (Freeman et al., 1998; Hu et al., 2003). However, the most important factor for preventing fractures is not the post design, but the final crown restoration (Hoag and Dwyer, 1982). Studies have also shown that the bonded posts resulted in less stresses within the dentin than nonbonded posts (Asmussen et al., 2005). There are many prefabricated post systems available in the market today. The disadvantage of the prefabricated posts is that the root canal is designed to receive the post rather than the post being designed to fit within the root canal. Active, threaded posts have the greatest retention; nonetheless, due to the threads indenting into the dentin, these posts can induce localized stress concentrations in the root dentin. This could lead to crack initiation and fatigue root fracture at a later time. Anatomical location of the tooth in the mouth influences predilection to fracture in root-filled teeth. Intact root-filled anterior teeth that have not lost further tooth structure beyond the endodontic access preparation are at minimal risk for fracture. On the other hand, posterior teeth bear greater occlusal loads than the anterior teeth during mastication, and adequate restorations must be planned to protect these teeth from VRF (Kishen, 2006).
Radiographic Appearance of VRF
The radiographic appearance of VRF is highly variable and is influenced by the direction of fracture, whether or not a root filling and post are present, and the time since the crack was initiated. Unless separation of the root segments has occurred, the fracture line is generally very difficult to detect. An angle shift is not likely to resolve this difficulty despite recommendations for radiographs at different horizontal angles (Tamse, 2006). This is because the fracture line is obscured if the direction of the X-ray beam diverges from the line of fracture by more than 4° (Kositbowornchai et al., 2001). The superimposition of other anatomical structures further complicates the picture. Because the fracture line is visible on radiographs in only a minority of cases (25–45%), the appearance of the surrounding bone also needs to be evaluated carefully for signs consistent with root fracture (Tamse, 2006; Tsesis et al., 2010). Although the pattern of bone loss may be indicative of VRF, it is very variable and should not be considered pathognomonic. Diagnosis can only be confirmed by direct visual inspection of the root surface or unequivocal evidence from the radiograph.
Cracked/Split Tooth
The cracked and split teeth normally fracture in a mesiodistal direction. Therefore, the crack line is almost never visible on radiographs. The diagnosis is more likely made based on the patient’s history, presenting signs, and clinical assessment, especially when the fracture is incomplete. The radiographic appearance of surrounding bone may provide supporting evidence, including a lateral lesion rather than a periapical lesion if the crack is incomplete (Figure 15.2). Sometimes an unusual and complex pattern of bone loss that includes the furcation area of molars may also be seen radiographically (Figures 15.3 and 15.4).
Figure 15.2 A mesiodistal crack in an otherwise intact mandibular molar. The crack is not visible on the radiograph because the direction of the crack is p/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


