Chapter 15 The Completely Edentulous Mandible: Treatment Plans for Fixed Restorations
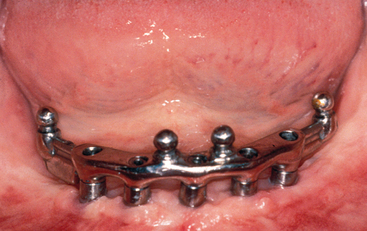
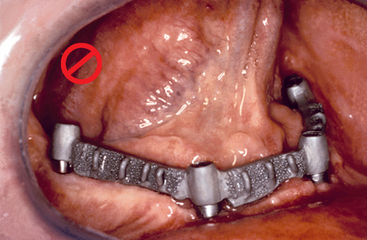
Twenty million adults in the United States have completely edentulous mandibular arches.1 Over the last 15 years, many of these patients have been treated with an implant overdenture, which is a vast improvement compared with a complete denture. Many of these same patients might have preferred a fixed prosthesis, but often for financial considerations they chose to have a removable prosthesis fabricated. Maxillary implant-supported removable prostheses may provide advantages over full-arch fixed restorations, such as upper lip support for esthetics and ease of daily maintenance of a removable prosthesis. However, unlike a maxillary denture, the labial flange of a mandibular overdenture rarely is required for esthetics. The laboratory and component costs for a hybrid fixed restoration are often similar to those for a fully implant-supported overdenture (RP-4). The chair time required to fabricate an overdenture and bar is similar to that for an implant-supported fixed prosthesis. Yet because dentures and partial dentures typically cost several times less than fixed restorations on teeth, the doctor often charges half the fee for an implant overdenture and bar compared with a fixed restoration. However, the laboratory fees, component fees, and chair time are similar for these two types of prostheses. If the fees for these two restorations were similar, many patients would opt for a fixed prosthesis (Figures 15-1 and 15-2).
COMPARING FIXED VERSUS REMOVABLE IMPLANT PROSTHESES
Removable implant overdentures require greater maintenance and exhibit more frequent prosthetic-related complications than fixed restorations. Walton and McEntee2 noted that there were three times more maintenance and adjustments for removable prostheses compared with fixed restorations. Implant overdentures (IODs) often require attachments to be changed or modified every 6 months to 2 years, and denture teeth often wear, requiring a new prosthesis to be fabricated every 5 to 7 years.2–7 In a review of literature by Goodacre et al., IODs have retention and adjustment problems 30% of the time, relines 19%, clip or attachment fracture 17%, and fracture of the prosthesis 12% of the time. Fixed prostheses need less repair and less maintenance and often last the life of the implant support. Although porcelain fractures with a fixed restoration may be costly to repair, over a lifetime, the implant-supported removable prosthesis may be more expensive.
A mandibular overdenture often traps food below its flanges, similar to a denture. Dentures are border-molded to the muscle attachment level to allow the floor of the mouth to raise during swallowing. As a consequence, food accumulates below the denture flange while the muscles are at rest and then is compressed under the restoration during deglutition. The contour of a fixed restoration is less prone to food entrapment (Box 15-1). The daily care for a bar implant overdenture (RP-4) is similar to that for a fixed mandibular restoration because ridge lap pontics are not required for esthetics or speech, as with some maxillary fixed prostheses.
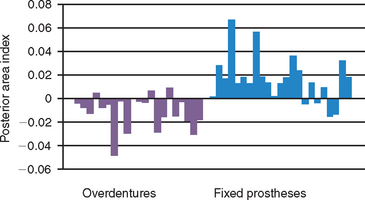
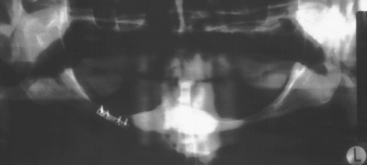
A more recent clinical study by Wright et al. has evauated posterior mandibular bone loss in implant overdentures (RP-5) compared with cantilevered fixed prostheses from anterior implants.8 The annual bone loss index observed in the RP-5 overdentures ranged from +0.02 to −0.05 with 14 of 20 patients losing bone in the posterior regions. On the other hand, the fixed prostheses group had a range from +0.07 to −0.015 with 18 of 22 patients gaining posterior bone area (Figure 15-3). Reddy et al. also found a similar clinical observation in 60 consecutively treated cantilevered fixed prostheses supported by five to six implants placed between the foarminae.9 The mandibular body height was measured 5, 10, 15 and 20 mm distal to the last implant. The baseline measurements up to 4 years after function increased from 7.25 ± 0.25 mm to 8.18 ± 0.18 mm. Nearly all of the bone growth occurred during the first year of function. Therefore an important role for the presence of a complete implant-supported restoration is the maintenance and even regeneration of posterior bone in the mandible. This is especially important because posterior bone loss in this region may lead to paresthasia and even mandibular body fracture (Figure 15-4).
Too often, the dentist offers overdentures as the only option for edentulous patients, rather than including fixed treatment options. The advantages of a fixed restoration over an overdenture warrant most all edentulous patients to be given an option for a fixed prosthesis. This chapter discusses fixed treatment planning options for the completely edentulous mandibular arches.10
FORCE FACTORS
The amount of force transmitted to an implant-fixed prosthesis is similar to that of a completely implant-supported overdenture (RP-4). In one aspect then, the number of implants to support either prosthesis type should be similar. Mandibular overdentures may be removed at night to decrease the risk of nocturnal parafunctional overload. However, most mandibular edentulous patients also have an edentulous maxilla. Therefore if the patient is willing to remove the maxillary denture at night, the risk of nocturnal parafunction also may be eliminated for patients with mandibular fixed prostheses. As a consequence, the number of implants required to restore a fixed prosthesis may be similar to a fully implant-supported overdenture.
MANDIBULAR DYNAMICS
Medial Movement
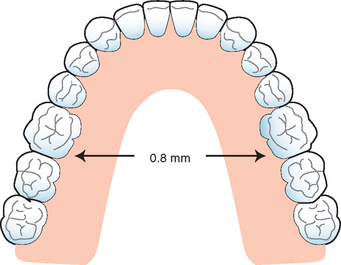
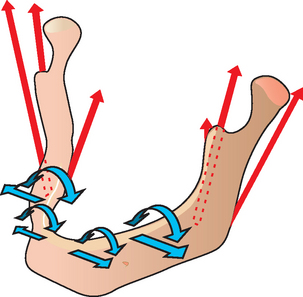
Many reports have addressed the dimensional changes of the mandible during jaw activity as a result of masticatory muscle action.11–19 Five different movements have been postulated.18 Medial convergence is the one most commonly addressed.19 The mandible between the mental foraminae is stable relative to flexure and torsion. However, distal to the foraminae, the mandible exhibits considerable movement toward the midline on opening.15–16 This movement is caused primarily by the attachment of internal pterygoid muscles on the medial ramus of the mandible. The distortion of the mandible occurs early in the opening cycle, and the maximum changes may occur with as little as 28% opening, or about 12 mm of mandibular movement.11 This flexure has also been observed during protrusive jaw movements.20,21 The greater the active opening and protrusive movements, the greater the amplitude. The amount of movement varies among individuals and depends on the density and volume of bone and the location of the site in question. The amplitude of the mandibular body flexure toward the midline has been measured to be as much as 800 μm in the first molar to the first molar region to as much as 1500 μm in the ramus-to-ramus sites (Figure 15-5). In a study by Hobkirk on deformation of the mandible in subjects with fixed dental implant prostheses, medial covergence up to 41 μm was observed.20
Torsion
Torsion of the mandibular body distal to the foraminae has also been documented in animal and human studies.22–26 Hylander evaluated larger members of the rhesus monkey family (macaque) and found the mandible twisted on the working side and bent in the parasagittal plane on the balancing side during the power stroke of mastication and unilateral molar biting.25 Parasagittal bending of the human jaw during unilateral biting was confirmed by Marx,26 who measured localized mandibular distortion in vivo in humans by using strain gauges on screws attached to cortical bone in the symphyseal and gonial regions. Hobkirk et al. confirmed the mandible of patients with implant prostheses measured up to 19 degrees of dorsoventral shear.22 The torsion during parafunction is caused primarily by forceful contraction of the masseter muscle attachments (Figure 15-6). Therefore parafunctional bruxism and clenching may cause problems in the implant support system and prosthesis when the mandibular teeth are splinted from molar to molar.
The posterior bone gain in edentulous patients restored with cantilevered prostheses from anterior implants may be a consequence of the mandibular flexure and torsion. Because the bite force may increase 300% with an implant prosthesis compared with a denture, the increased torsion may stimulate the posterior mandibular body to increase in size, as reported by Reddy et al.9 and Wright et al.8
The most common position of the mental foramen is between the first and second premolar teeth; therefore when splinting teeth distal to the bilateral premolar position, mandibular dynamics should be considered.27 A study by Miyamoto et al. identified jaw flexure as the primary cause of posterior implant loss in full- arch mandibular prostheses.28 The more distal the rigid splint from one side to the other, the greater the risk that mandibular dynamics may influence the implants or prosthesis prognosis. In addition, the body of the mandible flexes more when the size of the bone decreases. As a result, the Division C minus height (C–h) or D mandible flexes or exhibits torsion more than the Division A mandible, all other factors being similar.
As a consequence, posterior rigid, fixated implants splinted to each other in a full-arch restoration are subject to a considerable buccolingual force on opening and during parafunction.27–29 The difference in movement between an implant and a tooth has been addressed as a concern for dentists. The natural tooth movement ranges from 28 μm apically and 56 to 108 μm laterally. In contrast, the rigid implant has movement up to 5 μm apically and 10 to 60 μm laterally, yet the mandibular flexure and torsion may be more than 10 to 20 times the movement of a healthy tooth. Therefore the flexure and torsion of the mandibular body are more critical in the patient evaluation compared with whether an implant should be joined to the natural dentition.
Past authors have suggested four implants in the mandible with a full-arch splinted fixed restoration—two in the first molars and two in the canine regions30 (Figure 15-7). Additional implants have been used with this full-arch splinted restorative option, with up to four other implants in the premolar and the incisor regions.31 However, complete cross-arch splinting of posterior, molar rigid, fixated implants should be reconsidered in the mandible. The flexure of the mandible is thwarted by the prosthesis,22,27,29,32–34 but this introduces lateral stresses to the implants. These implant positions place the molar implants, screws, and bone at increased risk because of the mandibular flexure and torsion previously addressed.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses