Radiation Safety and Production of X-Rays
Learning Objectives
1 Pronounce, define, and spell the Key Terms.
2 Explain the uses of dental radiology.
3 Describe the properties of x-rays.
4 Explain the differences between somatic and genetic effects of x-rays.
5 Discuss the methods used to protect patients from radiation.
6 Explain the ALARA principle.
7 Describe how filters and collimators influence the amount of radiation the patient receives.
9 Describe how the use of film-holding devices limits the amount of exposure the patient receives.
11 Identify the parts of an x-ray machine.
12 Define radiopaque and radiolucent.
13 Explain the factors that affect the density and contrast of a dental radiograph.
Key Terms
Absorbed Dose
Acute Radiation Exposure
ALARA Principle
Anode
Background Radiation
Cathode
Cervical Collar
Chronic Radiation Exposure
Collimation
Collimator
Contrast
Control Panel
Cumulative Effects
Density
Dose Equivalence
Filter
Filtration
Focusing Cup
F-Speed Film
Genetic Changes
Ionization
Latent Period
Leakage Radiation
Maximum Permissible Dose (MPD)
Object-Film Distance (OFD)
Photon
Position Indicator Device (PID)
Primary Radiation
Radiation Monitoring
Radiolucent
Radiopaque
Scatter Radiation
Secondary Radiation
Somatic Changes
Source-Film Distance
Tubehead
Dental images are essential in the practice of dentistry. These images may be produced on conventional x-ray film or by digital technology. Regardless of the technique used, a quality image is necessary to identify and diagnose conditions that otherwise may go undetected.
Dental images, commonly known as x-rays, are part of the patient’s permanent dental record. Radiation, which is used to produce dental images, has the ability to cause damage to all types of living tissue. Any exposure to radiation, no matter how small, has the potential to cause harm to the operator and the patient.
The benefits of using x-rays in dentistry certainly outweigh the risks when proper safety procedures are followed (Box 15-1). This chapter discusses radiation hazards, production of x-rays, and methods used to protect the patient and the operator from the harmful effects of exposure to radiation.
Radiation Physics
An understanding of the basic principles of radiation physics and how x-rays are produced will help you to practice safely and produce high-quality images.
Definition
X-rays can be defined as weightless bundles of energy (photons) without an electrical charge that travel in waves at the speed of light.
Atomic Structure
The basic anatomic structure of matter is important because it relates directly to the ways in which x-rays are produced, emitted (given off) from the machine, and absorbed by the patient’s and the operator’s body tissue.
All matter is made of atoms. Atoms are extremely minute and are composed of (1) an inner core, or nucleus, which possesses a positive electrical charge; and (2) a number of negatively charged particles called electrons that orbit around the nucleus. The nucleus of an atom is composed of positively charged subatomic particles called protons and subatomic particles called neutrons that have no charge.
The arrangement within the atom is similar to that of the solar system. The atom has a nucleus as its center, like the sun, and the electrons revolve around it like planets (Figure 15-1). The electrons remain stable in their orbit unless disturbed or removed.
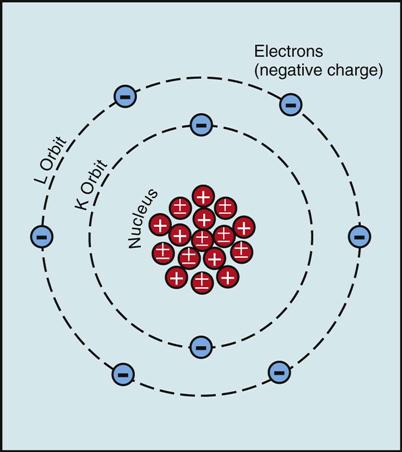
In the neutral or stable atom, the number of orbiting electrons (−) equals the number of protons (+) in the nucleus; hence the atom is electrically neutral.
Atoms in turn join to form molecules. A molecule is the smallest particle of a substance that retains the property of the original substance.
Ionization
Ionization is the harmful effect of x-rays in humans that results in disruption of cellular structure and causes permanent damage to living cells and tissue. When x-rays strike a patient’s tissue, ionization results.
During ionization, electrons are removed from electrically stable atoms by collisions with photons. (A photon is a minute bundle of pure energy that has no weight or mass.) The atoms that lose electrons become positive ions. Negative electrons become negative ions. As such, they are unstable structures capable of interacting with (and damaging) other atoms, tissue, or chemicals.
Properties of X-Rays
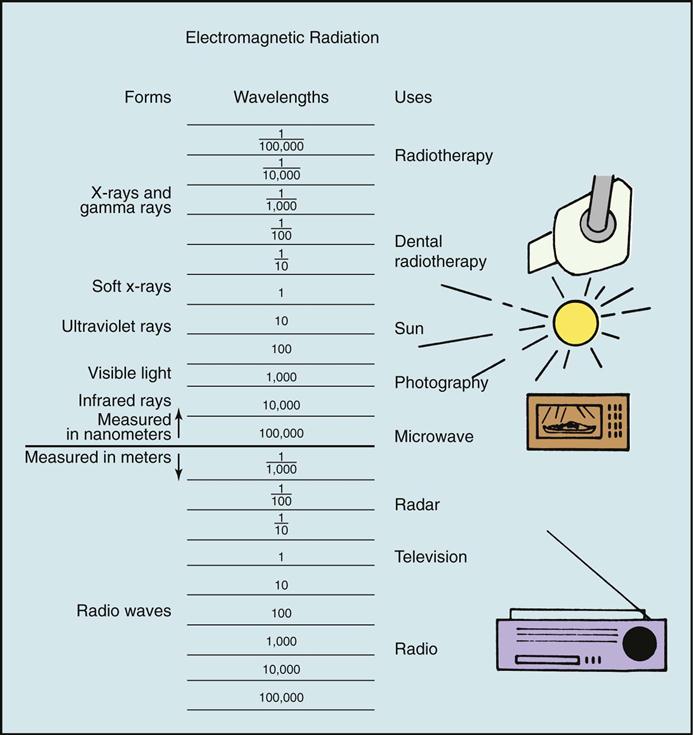
X-rays are a form of energy that can penetrate matter and have unique properties (Table 15-1). Like visible light, radar, radio, and television waves, x-rays belong to a group called electromagnetic radiation (Figure 15-2).
TABLE 15-1
| Property | Comment |
| Appearance | Invisible |
| Mass | No mass or weight |
| Charge | No charge |
| Speed | Travel at the speed of light |
| Path of travel | Travel in a straight line but can be deflected or scattered |
| Focusing ability | Cannot be focused |
| Penetrating ability | Penetrate solids, liquids, and gases |
| Absorption | Can be absorbed by matter |
| Ionization ability | Do cause ionization |
| Fluorescence | Can cause certain substances to fluoresce (glow) |
| Effect on film | Produce an image on photographic film |
| Effect on living tissue | Cause biologic changes in living cells |
Electromagnetic radiation is made of photons that travel through space at the speed of light in a straight line with a wavelike motion.
The shorter the wavelength of radiation, the greater its energy. Because of the high energy of short wavelengths, they are able to penetrate matter more easily than longer wavelengths. The unique properties of x-rays make them especially valuable in dentistry.
Types of Radiation
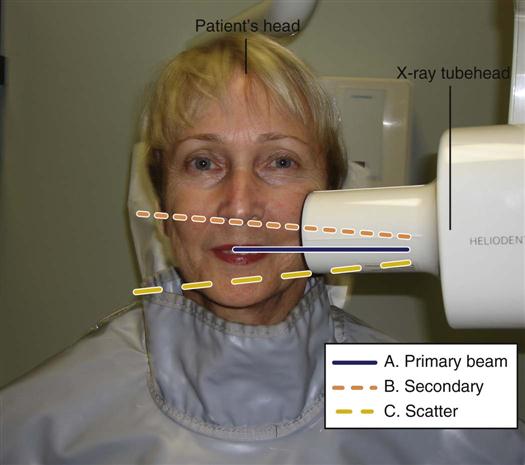
Primary radiation, also known as the central ray or primary beam, is the stream of radiation as it is emitted from the x-ray unit. The primary beam travels in a straight line and contains powerful short waves. It is the short waves in the dental ray that produce diagnostically useful radiographs (Figure 15-3, A).
Secondary radiation in dentistry is given off after the primary beam comes into contact with the soft tissue of the head, the bones of the skull, and the teeth. Secondary radiation is less penetrating than primary radiation because the rays become weaker after they contact the tissue; however, the patient still may absorb these rays (see Figure 15-3, B).
Scatter radiation is a form of secondary radiation that occurs when an x-ray is deflected from its path during impact with the patient. (Deflected means turned aside.)
Scatter radiation travels in all directions and is impossible to confine. Without adequate protective barriers, the operator and others nearby may be affected by exposure to scatter radiation (see Figure 15-3, C).
Leakage radiation is radiation that escapes in all directions from a faulty x-ray head. Equipment should be checked frequently and repaired immediately when necessary.
Radiation Measurement
Just as distance can be measured in miles or kilometers, and time can be measured in hours or minutes, radiation is also measured. Two sets of systems are currently used to define the way radiation is measured. The older system is referred to as the traditional, or standard system. The newer system is the metric equivalent known as the SI or Système Internationale d’Unités.
Traditional units of radiation measurement include:
Both systems are presented here, and the units are compared in Table 15-2.
TABLE 15-2
Equivalent Traditional and SI Units of Radiation Measurement
| Measurement | Traditional System | SI System |
| Radiation exposure | 1 roentgen (R) | 1 coulomb per kilogram (C/kg) |
| Absorbed dose | 100 radiation absorbed doses (rad) | 1 gray (Gy) |
| Dose equivalence | 100 roentgen equivalents (in) man (rem) | 1 sievert (Sv) |
Radiation Exposure
The term radiation exposure refers to the amount of radiation a person is exposed to and is measured in SI units as coulombs per kilogram (c/kg). The traditional term is the roentgen (R). One coulomb per kilogram (c/kg) equals 1 roentgen (R).
Absorbed Dose
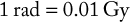
The amount of radiation energy actually absorbed by tissue is the absorbed dose. The SI unit of absorbed dose is called a gray (Gy). The traditional system used the term radiation absorbed dose (rad) as the unit of measurement. The conversions for rad and Gy are as follows:
< ?xml:namespace prefix = "mml" ns = "http://www.w3.org/1998/Math/MathML" />
Dose Equivalence
The dose equivalence measurement is used to compare the biologic effects of different types of radiation.
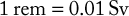
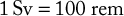
The SI unit of dose equivalence is the sievert (Sv). The traditional unit is a roentgen equivalent (in) man (rem). One sievert (Sv) equals 100 rem. Technically, there are some differences between the units of radiation measurement; however, in dental radiology, the units are virtually interchangeable. Conversions for the rem and sievert are as follows:
Radiation Hazards and Protection
We are exposed to radiation every day of our lives. Background radiation comes from natural sources, such as radioactive materials in the ground and cosmic radiation from space. Exposure from medical or dental sources is an additional risk. Because of their concern, patients frequently say, “I’ve heard x-rays are bad for me. Do you really have to take them?” The dental assistant must anticipate this patient reaction and be able to explain to the patient the risks and diagnostic benefits of dental radiation, the safety precautions used during radiographic exposure, and the benefits of detecting disease that might not otherwise be detected, which far outweigh the risks from receiving small doses of radiation.
Note: Two important concepts are basic to radiation protection. The first is the concept of maximum permissible dose, and the second is the ALARA principle.
Maximum Permissible Dose
The maximum permissible dose (MPD) is the exposure limit for those who are occupationally exposed to radiation when observing all safety practices. This amount of radiation to the whole body produces very little chance of injury.
The MPD for whole-body exposure for an occupationally exposed person (e.g., dental radiographer) is 0.05 Sv (5 rem).
Occupationally exposed women who are pregnant are allowed an MPD of only 0.005 Sv (0.5 rem) per year. This is the same dose limit that applies to the general population.
Dental personnel should strive for an occupational dose of zero by adhering to strict radiation protection practices.
ALARA Principle
The ALARA principle or concept states that all exposure to radiation must be kept As Low As Reasonably Achievable. Every possible method of reducing exposure to radiation should be used. The radiation protection measures detailed in this chapter can be used to minimize both patient and operator exposure.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses