Pain and Anxiety Control
Learning Objectives
1 Pronounce, define, and spell the Key Terms.
2 Discuss the importance of pain and anxiety control in dentistry.
3 Describe the composition and application of topical anesthetics.
4 Describe the composition and application of local anesthetics.
5 Discuss nitrous oxide/oxygen sedation and its use in dentistry.
6 Identify specific safety precautions when using nitrous oxide/oxygen.
Key Terms
Analgesia
Anesthetics
Duration
Induction
Nitrous Oxide/Oxygen
Sedation
Syringe
Vasoconstrictors
An extensive range of anxiety and pain control procedures allow the dental profession to provide oral healthcare to millions of individuals who would otherwise remain untreated because of their fear of pain. Pain and anxiety control is defined as the practice of various chemical, physiologic, and psychological approaches to prevent and treat preoperative, operative, and postoperative pain and anxiety. Many different methods of pain and anxiety control are used in the general and specialty areas of dentistry (Box 14-1).
For most patients receiving dental treatment, pain control can be accomplished with the use of a local anesthetic. Some patients become apprehensive about receiving dental treatment and will require additional means to help control their anxiety. Administration of nitrous oxide/oxygen and/or antianxiety drugs may be the added element that will provide relief to the patient when receiving dental care.
Use of intravenous (IV) sedation or general anesthesia would be prescribed for a patient with the need for invasive or extensive amounts of dental treatment, or for one who is medically or physically compromised.
The dental assistant must be familiar with the procedure, types of equipment, and the variety of anesthetics used in all areas of dentistry.
Topical Anesthesia
Topical anesthesia is a procedure when a highly concentrated anesthetic agent is applied topically to the area where a local anesthetic injection is to take place. This provides a temporary numbing effect on the nerve endings on the surface of the oral mucosa. Topical anesthetic agents are available in the form of ointments, liquids, sprays, and patches (Figure 14-1).
Topical Anesthetic Ointment
Topical anesthetic ointment, can lessen or even eliminate that initial “pinch” from an injection. For maximum effectiveness, the topical anesthetic is applied to the dried mucosal surface at the site of the injection with a cotton-tip applicator for 2 to 5 minutes.
Local Anesthesia
Local anesthesia is a procedure that was first introduced in the mid-1800s. This type of anesthesia provides a safe, effective, and dependable method for a suitable duration in virtually all forms of dental treatment.
Local Anesthetic Agents
Local anesthetic agents are the most frequently used form of pain control in dentistry and is the drug of choice to reduce or relieve any associated pain that may take place during and immediately following a dental procedure.
The chemical makeup of these anesthetics blocks the ability of the nerve membrane to generate an impulse. Because of this block, the impulse does not transmit to the brain to feel pain. To receive local anesthesia, the agent is injected near the nerve that specifically affects the tooth receiving dental treatment.
Local anesthetics are broadly classified under two chemical groups: amides and esters. The amides were first introduced to clinical practice in the 1940s and provide the standards by which all other local anesthetics are measured. The amide local anesthetics are metabolized by the liver.
Induction and Duration of an Anesthetic
Induction is the time frame from when the injection is given to the complete effective numbing sensation. Duration is the time frame from when the injection is given until the numbing sensation is gone. This will vary from patient to patient. Local anesthetics include:
Vasoconstrictors
Vasoconstrictors are drugs that have been added to the local anesthetic agent to slow down the intake of the anesthetic agent and increase the duration of action. The action of a vasoconstrictor can:
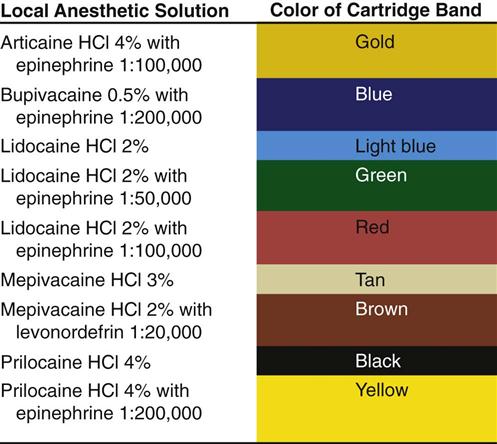
The most common vasoconstrictors used are epinephrine, levonordefrin, and neo-Cobefrin. The ratio of vasoconstrictor to anesthetic solution is supplied as: 1 : 50,000, 1 : 100,000, or 1 : 200,000. A concentration of 1 : 100,000 indicates that one part of the vasoconstrictor is diluted in 100,000 parts of anesthetic solution. The lower the second number, the larger the amount of epinephrine in the solution.
Health Status of the Patient
Local anesthetics and vasoconstrictors are considered very safe drugs when administered properly. Certain health conditions may affect the dentist’s choice in the type of anesthetic solution and whether or not that solution contains a vasoconstrictor. Health conditions are noted in the patient’s medical history, and the dentist must be alerted to them when selecting a local anesthetic (Box 14-2).
Local Anesthesia Methods
The location and the nerves of the tooth, or teeth, to be anesthetized determine the type of injection method to be used. The two principal methods used in dentistry are infiltration anesthesia and block anesthesia.
Infiltration Anesthesia
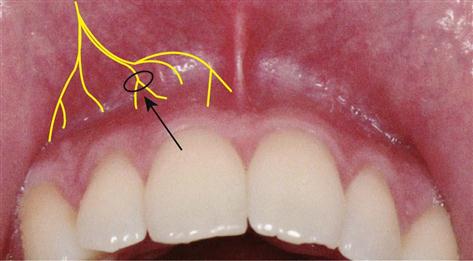
Infiltration anesthesia involves injecting the anesthetic solution into the tissue near the apices of the tooth to be treated (Figure 14-2). It is possible to infiltrate a maxillary tooth because the alveolar cancellous bone is porous and allows the solution to diffuse through the bone and reach the nerve at the apices of the tooth.
Periodontal Ligament Injection
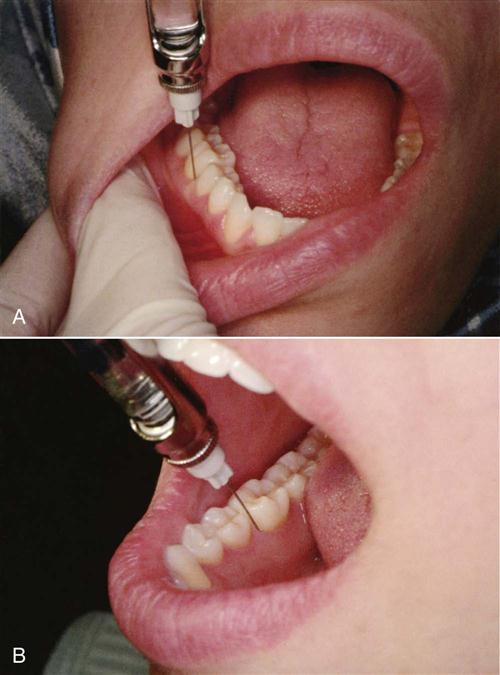
An alternative infiltration technique involves injection of the anesthetic solution under pressure directly into the periodontal ligament and surrounding gingival tissue (Figure 14-3). This type of injection can be completed by the use of a conventional syringe or a specialized periodontal ligament injection syringe.
Block Anesthesia
Block anesthesia involves injecting the anesthetic solution around a larger nerve, which means numbing a larger area (Figure 14-4). Because the mandibular bone is denser and the nerve system is designed differently from that of the maxillary bone, the anesthetic is injected into a nerve trunk.

Mandibular nerve block is obtained by injecting into the inferior alveolar nerve, which numbs the half of the lower jaw including the teeth, tongue, and lip.
Buccal nerve block provides anesthesia to the buccal soft tissues closest to the mandibular molars.
Incisive nerve block is given at the site of the mental foramen, numbing the anterior teeth.
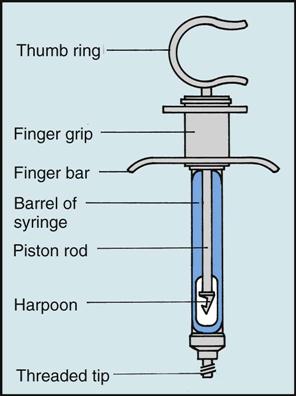
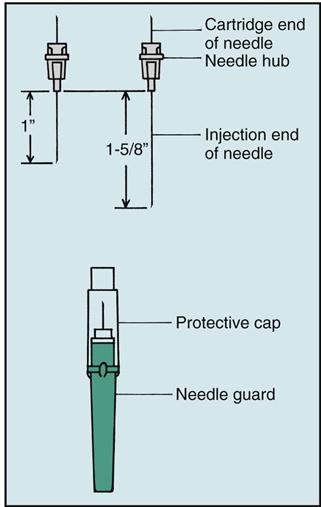
Assembling the Anesthetic Syringe
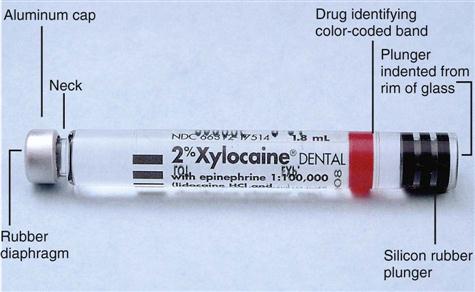
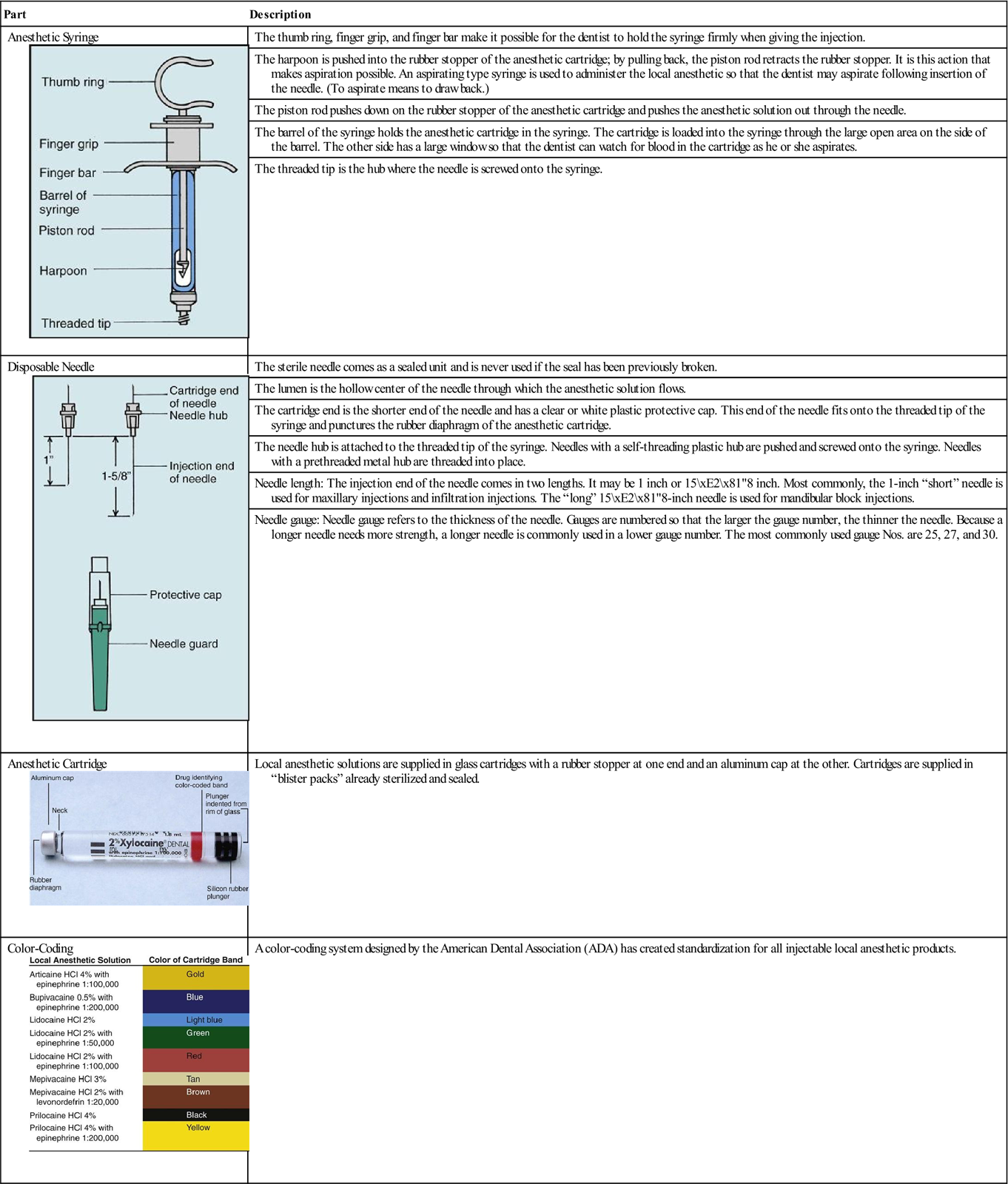
When gathering the appropriate setup (Table 14-1) to assemble the anesthetic syringe, you will need to know a few details before assembly: (1) the type of anesthetic and (2) the needle length and needle gauge.
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
From Malamed SF: Handbook of local anesthesia, ed 6, St Louis, 2013, Mosby.
See Procedure 14-2: Assembling the Local Anesthetic Syringe.
Transferring the Anesthetic Syringe
The transfer of a syringe can take place in the transfer zone just below the patient’s chin or behind the patient’s head. If the patient is apprehensive or if the dentist is anesthetizing a child, the transfer behind the patient’s head is more suitable.
Always be alert to infection control and protocol. The transfer of a sterile syringe is appropriate, but once the syringe has been used, it becomes contaminated, and the dentist will need to recap and retrieve the syringe for additional injections.
See Procedure 14-3: Assisting in the Administration of Local Anesthesia.
Local Anesthetic Cautions
Needle stick injuries are serious, and care must be taken to prevent such accidents when handling a contaminated syringe. An important precautionary directive from the Centers for Disease Control and Prevention (CDC) states that contaminated needles used in dental procedures should be recapped by a/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses