CHAPTER 14 Mandibular Subperiosteal Implant Surgery
CAVEATS
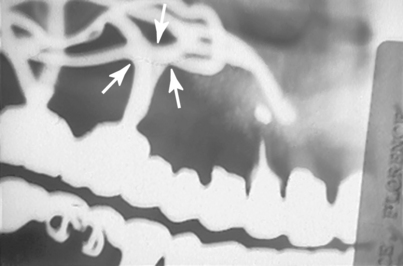
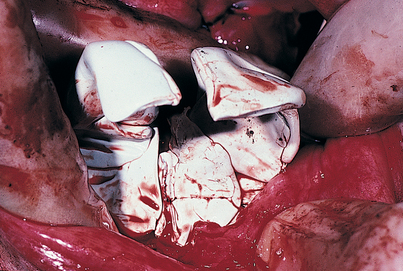
Some clinicians maintain that grooves can be cut into the crest of the ridge (i.e., “witness marks”) to allow countersinking of primary struts. However, this should never be done, because it may threaten the prognosis of the implant. Bone has plastic memory, and if it is altered by cutting a groove or mortise form to seat a component of the infrastructure, it almost immediately begins to undergo resorption. Within weeks, what might begin as an intimate metal to bone relationship can become a growing, rounded radiolucency. This phenomenon, which takes place beneath the abutments, can be the first sign of a cascade of events leading to implant failure (Fig. 14-1).
COMPLETELY EDENTULOUS DESIGNS
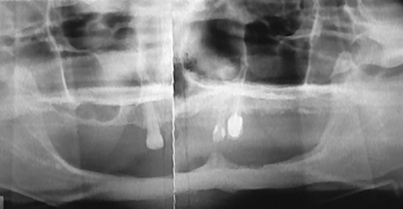
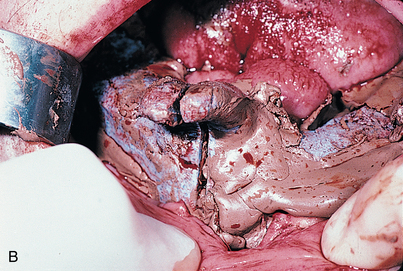
Preventing injury to mental or dehiscent mandibular nerves is important. The implant design should be selected with care in advance (Fig. 14-2), and if any question of dehiscence arises, a tripodal infrastructure (discussed later in the chapter) should be planned.
Procedure
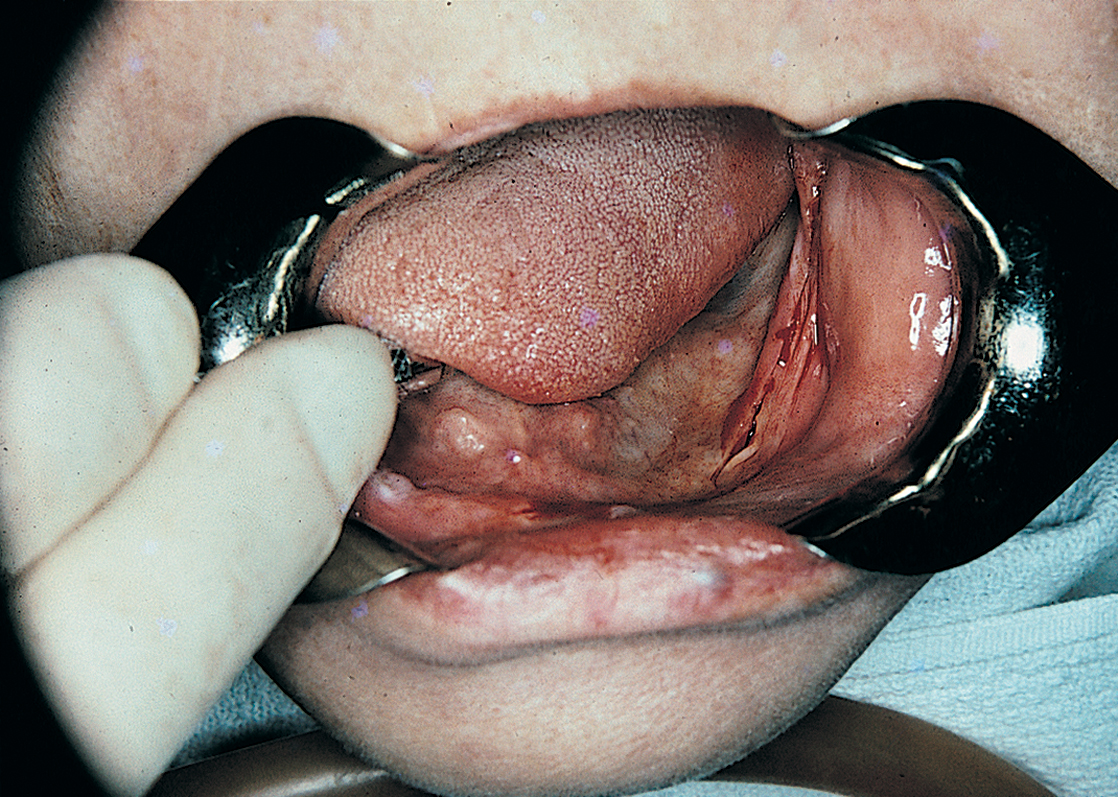
Before beginning surgery, the surgeon should examine the intact mucosa that covers the mandible. The sublingual adnexa are palpated (i.e., sublingual glands, mylohyoid and genioglossus muscles, plicae sublinguales, Wharton’s ducts). These adnexa usually lie above the ridge crest. The vestibules often are ill defined, and a mucosal linea alba is seen at the ridge crest (Fig. 14-3).
Incision
A Bard-Parker (BP) No. 15 blade is used to trace the linea alba, a fine white scar on the crest of the ridge that results from the trauma of past extractions and denture wearing. The incision starts at one retromolar pad and proceeds around the arch to the contralateral side (Fig. 14-4). If the radiograph shows that the mental foramina are at or near the crest of the ridge, the incisions are curved slightly lingually to avoid injuring the emerging neurovascular bundles. In addition, a vertical relieving incision is made just lateral to the labial frenulum. Incisions are made directly to bone so that they need not be retraced.
Reflection
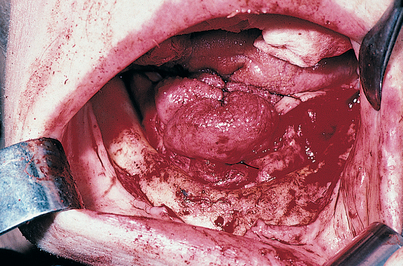
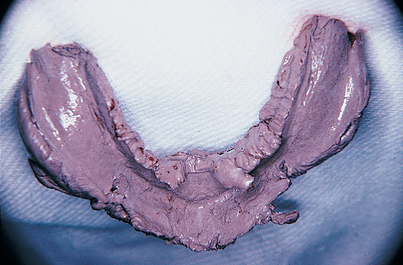
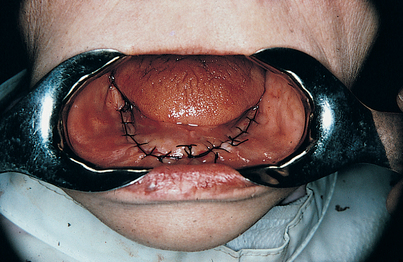
After vital anatomic structures have been exposed, the two lingual flaps are sutured to each other with 2-0 black silk sutures, which are brought across the dorsum of the tongue. If the tongue slips from beneath these shoestring ties, its lateral border is included on either side in the suturing process. These sutures are tied tightly so that the tongue, floor of the mouth, and lingual flaps are bundled compactly together in the midline and the mandible is well exposed for impression making (Fig. 14-5). The exposed bone is protected with saline-moistened sponges; this creates hemostasis and prevents dehydration of the tissues.
Impression Making
Surgical Jaw Relationship: Centric Recording
The patient’s acceptable maxillary denture prosthesis or a prefabricated, properly adjusted wax rim is placed on a base plate, and a thick roll of Optosil putty or a prefabricated bite rim is used to establish centric and vertical relationships. The elastomer is pressed and molded to the bone while the patient is guided to closure in a natural mandibular position (Fig. 14-9). The Optosil is removed after it has set; the wound is reinspected and irrigated again with saline, and the retraction sutures are removed from the tongue and buccal flaps. An impression of the upper denture, which should have been made previously, serves as a countermodel.
Closure
Implant Design
Implant Insertion
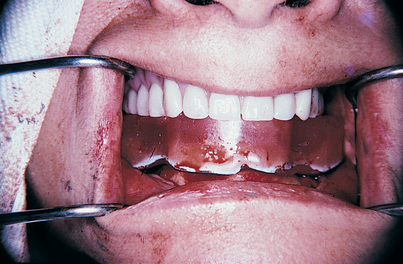
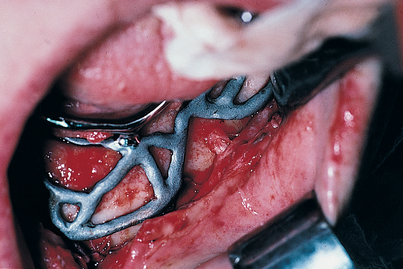
If a two-stage “immediate” 12- to 24-hour insertion is planned, regional anesthesia is more difficult to achieve. When the silk sutures are removed, the tissues fall open with ease (which is an advantage of the 1-day procedure). The host site is irrigated with care, and all residual clots and debris are removed. A Poole or Frazier plastic suction tip is used rather than a metal one. The sterilized, passivated implant (see Appendix E) is seated in the host site. It is tapped firmly into place with an orangewood stick and a mallet, with care taken that the flaps are not caught beneath the peripheral struts. Accurate adaptation and primary retention must be verified (Fig. 14-13).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses