14 Lasers in Major Oral and Maxillofacial Surgery
Greater soft tissue needs and fewer hard tissue needs differentiate OMS from other dental specialties. In addition, the use of lasers for skin procedures further complicates the choice of appropriate wavelength, technique, and postoperative care. As with any procedure, choosing the proper laser must be based on the intended target tissue and its absorption characteristics. With cosmetic procedures, the lateral thermal effects of a particular wavelength are important to the surgical goal while limiting lateral damage and scarring.1 Unlike in the oral cavity, this complication in skin is potentially devastating.
Choosing a Surgical Laser
Surprisingly, the primary laser used in major OMS and facial cosmetic surgery remains, after more than 25 years, the 10,600-nm CO2 laser.2 Its excellent water absorption, extinction length, depth of penetration, and consistency in soft tissue make it an excellent choice for most soft tissue procedures in the mouth. In addition, when used carefully and correctly, the CO2 laser can be used for cosmetic facial resurfacing, resulting in a predictable and substantial ablation of the epithelium and dermis.
The erbium-doped yttrium-aluminum-garnet (Er:YAG) and erbium, chromium–doped yttrium-scandium-gallium-garnet (Er,Cr:YSGG) lasers are also useful in major OMS, although they have not reached the level of popularity of the CO2 laser. Currently, most major hard tissue procedures (e.g., osteotomies) are too time-consuming when using these lasers. However, lesser osseous procedures (e.g., sinus lifts) are easily and quickly accomplished with these wavelengths. The Er:YAG has also been used for cosmetic facial resurfacing.3,4 Because of its reduced depth of effect in skin compared with the CO2, postoperative erythema and disability are greatly decreased with the Er:YAG laser. Unfortunately, the resurfacing effect and results are also greatly diminished, which has resulted in fewer surgeons using erbium lasers.
Borrowed from orthopedics and urology, the holmium:YAG laser is almost exclusively used in major OMS to perform endoscopic temporomandibular joint surgery. This wavelength has the ability to transmit through a water-filled environment such as a joint, while having soft tissue effects that mimic a CO2 laser (e.g., cutting, coagulating, ablating). This is done by perforating the joint with two hollow canulas, one for endoscopic visualization and one for the Ho:YAG laser fiber. The procedure is then done under video monitoring. The small-incision surgery leads to significantly decreased recovery time and complications.5
Solid-state lasers such as the diodes (810-1064 nm) have become very popular in general dentistry because of their small size, low cost, fiberoptic delivery, and ease of use for minor surgery of oral soft tissues.6 Unfortunately, for major OMS procedures, these lasers are very inefficient compared with the CO2 laser. Although hard tissue damage when using a CO2 laser is a justifiable safety concern, the diminished effect of the diode lasers makes them useful only for these minor oral surgical procedures.
The use of low-level diode lasers for noninvasive, athermal laser therapy is popular in European countries and has been studied in the United States, but generally has not proved effective for major surgical indications. Although studies confirm that low-level lasers have beneficial physiological effects, their specific advantages for OMS procedures remain unclear7,8 (Figure 14-1). (See Chapter 15.)
Intense pulsed light (IPL) sources use highly concentrated light waves to perform several procedures similar to lasers. Unlike true lasers, however, IPL sources are polychromatic and are neither collimated nor coherent (Figure 14-2). Because they generally have deeper tissue penetration and target tissue pigments and vascularity, primary uses include dermatological lesions and hair removal (targeting follicular pigmentation).9
Several lasers are also used in OMS for dermatological purposes. These wavelengths are highly specific for particular pigments or vascular tissues and include the copper vapor, gold vapor, flashlamp-pumped pulsed dye, pulsed Nd:YAG, and potassium titanyl phosphate (KTP) YAG lasers.10 The choice of wavelength must be based on individual patient needs, patient age, lesion color and depth, and laser availability.11
Safety and Anesthesia Considerations
The laser beam is a high-intensity light that, if directed at a reflective surface, can change its intended path while maintaining its focal properties. This can result in a reflected beam striking unintended targets with full power. Objects most vulnerable to this misdirected beam are eyes, skin, and nearby flammable objects.12 Appropriate warning signs should be posted outside the operating suite indicating the type of laser being used, the risk class of the laser, and the required personal safety equipment13 (Figure 14-3). Protective eyewear with eye shields must be worn at all times by the patient and personnel to avoid ophthalmic injury. Each laser has a specific type of eyewear that will absorb its particular wavelength.
Flammable patient drapes, including standard paper and plastic drapes used in the operating room (OR), are a source of ignition and should not be used. Instead, laser-resistant drapes or cloth drapes saturated in water should be used around the surgical field.13 Alcohol preparation of the field should also be avoided, because this can serve as a potential ignition source if not allowed to vaporize completely before laser use.
Three main techniques are available to prevent the potential fire hazards associated with the use of conventional endotracheal (ET) tubes during laser surgery14: (1) no airway, (2) protection of the surface of a conventional tube, and (3) use of a noncombustible tube. Many OMS procedures, whether done in the office or operating suite, can use total intravenous (IV) anesthesia technique while “chinning” the patient (using chin thrust as for CPR) or using a nasal airway. The Rousch red-rubber nasal airway has been found to be safe for laser procedures.15
The previous method, however, is not always practical for procedures of long duration in which case a definitive airway is necessary, such as a conventional ET tube with a protective material on its external surface. The materials of choice are metallic foil wrapped around the tube or silver anode sheet that adheres to the tube.13 The foil is often cumbersome and can result in exposure of the tube when manipulated, whereas the silver anode sheet adheres to the tube and is less likely to lead to exposure.
Two types of noncombustible ET tubes are currently available: the metallic tube, which contains no combustible material, and the ceramic-coated tube (Xomed)13 (Figure 14-4). The metallic tube, however, cannot be used for nasal intubation and does not come with a cuff, which prevents the use of a normal anesthesia circuit.
Flammable gases must be avoided during laser surgery. Most inhalational anesthetics used in ORs today are not flammable and include sevoflurane, isoflurane, enflurane, and halothane. Ether and cyclopropane, which are not used by most anesthesiologists, are combustible and should not be used.13
The concentration of oxygen with inhalational agents should also be addressed. Ideally, the lowest concentration possible is used while maintaining an acceptable oxygen saturation level. To accomplish this, the oxygen is diluted with regular compressed air or with helium, both of which reduce flammability (Figure 14-5). Nitrous oxide mixed with oxygen, however, possesses the same flammability as oxygen alone and is avoided.12
Tumor Resective Surgery (Excision vs. Ablation)
The laser is a versatile surgical instrument that can be used in three basic ways: excision/incision, ablation/vaporization, and hemostasis/coagulation.16 The technique used is based on the clinical situation and three parameters controlled by the surgeon: power, spot size, and time.
Excision
When used for excisional purposes, the laser is basically a “light scalpel” producing precision cuts without the bleeding of traditional scalpel surgery. For optimal results, the spot size should be kept as small as possible with the particular laser used (usually 0.1-0.5 mm), which is accomplished by keeping the handpiece at its focal length from the tissue.17 This is known as the focused mode. The focal length is also variable depending on the handpiece, ranging from 1 mm to 1 cm from the end of the handpiece to the tissue.
The technique for excision of a lesion remains the same regardless of the laser system used. It is recommended first to outline the intended incision line by using an intermittent, gated, or pulsed mode with the laser set at a lower power. This will provide superficial guiding marks while avoiding deep penetration into the tissue, allowing the surgeon to adjust the location of the margins if necessary. Of note, when performing an excisional biopsy, an additional 0.5 mm should be added circumferentially to the margin to account for the lateral zone of thermal necrosis associated with the laser.13
Ablation
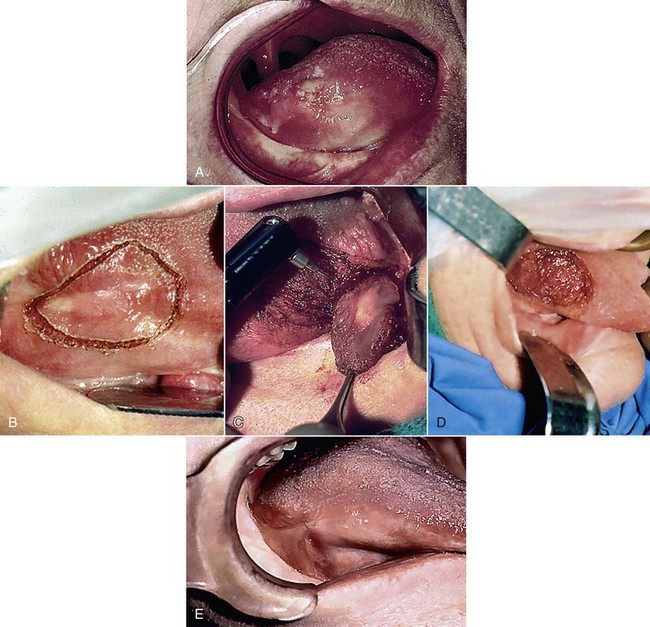
The technique for ablation begins with the same outlining procedure described for the excisional technique. Next, the laser is defocused by moving the handpiece farther from the tissue, thereby widening the laser beam and increasing the spot size. Spot sizes ranging from 1.5 to 3.0 mm are typically used. The now-defocused beam is traversed along the lesion in multiple side-by-side strokes, creating multiple “U”s (Figure 14-6).
Premalignant Lesions
Premalignant lesions come in the form of leukoplakia, erythroplakia, or a mixed form of the two known as erythroleukoplakia. The possibility of malignant transformation of these lesions is 36.3% to 43.0% in the presence of epithelial dysplasia, and 23.4% to 38.0% without epithelial dysplasia.18 Also, patients with these conditions have a 50- to 60-fold greater risk of developing oral cancer than patients without the lesions. Traditional treatment has involved surgical excision with a scalpel, which has many disadvantages compared with laser excision or ablation procedures. The advantages of using a laser include better control of bleeding, less surgical time, more precise tissue removal, less morbidity and complications, and excellent healing with virtually no scarring.19 Many surgeons also believe that the cauterization effect of the laser on blood vessels and lymphatic channels decreases the amount of hematogenous and lymphatic seeding, thereby lowering recurrence rates.20,21
Laser treatment of premalignant lesions is through excision or ablation. Both procedures begin with outlining the lesion, as discussed earlier, with the depth of the cut being deep to the lesion itself, usually 4 to 9 mm.22 If excision is to be performed, the affected tissue is elevated at one end and undermined, with the laser acting as a cutting tool. If ablation is chosen (usual treatment of choice), the laser is defocused and the tissue removed in the multiple side-by-side U pattern described earlier.
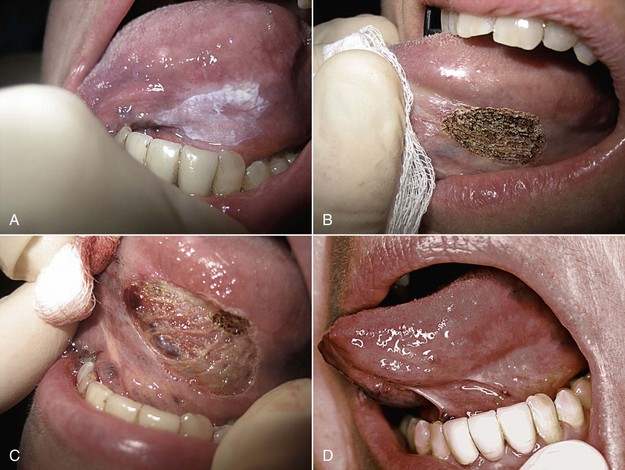
Figure 14-7 illustrates ablation of a leukoplakia on the ventrolateral surface of the tongue. Multiple passes are usually required until removal is complete. With the bloodless surgical field produced by the laser, visual confirmation of complete removal is much easier than with scalpel surgery. The area is then left to re-epithelialize by secondary intention, avoiding sutures and the possible distortion and scarring.
Roodenburg et al.18 followed 70 patients with 103 oral leukoplakias treated with laser ablation for a mean of 5.3 years and found a cure rate of 90%. Similarly, Thompson and Wylie23 reviewed 57 consecutive patients with laser-treated oral dysplastic lesions. After 44 months, 76% of the patients had no recurrence. These results are comparable to the 80% success rate seen with conventional scalpel surgery.
Malignant lesions and Aggressive Benign Lesions
The laser is an accepted and useful surgical tool for the treatment of malignant and aggressive benign lesions of the larynx, pharynx, oral cavity, and lips. Its use offers many advantages not seen with conventional scalpel surgery. Aside from the bloodless surgical field, shorter surgical time, and decreased patient morbidity, there are advantages specific to these potentially lethal conditions. First, lasers seal lymphatic vessels at the surgical margins, which reduces seeding of malignant cells and potential metastasis.24 Second, more nondiseased tissue adjacent to the lesion is preserved. Typical cancer margins are 1.5 to 2 cm beyond any visual or palpable tumor.13 Better visualization, with a bloodless field, allows the surgeon to remove tissue more precisely without sacrificing unnecessary tissue.
Figure 14-8 demonstrates excision of a T1N0M0 squamous cell carcinoma of the tongue. Laser microsurgery using a surgical microscope helps the surgeon distinguish between healthy and tumor tissue and preserve even more normal tissue by taking narrower margins.25 If local tumor recurrence were to occur, more re-treatment options are available than with conventional scalpel surgery.26
Verrucous carcinoma is a slow-growing, nonmetastasizing form of squamous cell carcinoma that is most frequently found in (but not limited to) the mouth.27 Clinically, this white, cauliflower-like lesion is found most often in elderly patients.28 The etiology is unknown, but heavy use of tobacco (snuff, chewing tobacco, or cigarettes) may be the primary factor.29,30 Some postulate that human papillomavirus is associated with verrucous carcinoma, but most studies have failed to prove this.31,32 Treatment of these lesions has traditionally been shave excision, cryosurgery, chemotherapy, or a combination, often requiring multiple treatments that may lead to scarring.33–35 The CO2 laser has proved to be an effective means of treating verrucous carcinoma by total excision in cutting mode. Vaporization can be performed on the premalignant form, proliferative verrucous leukoplakia.13
Vascular Lesions
Vascular lesions of the head and neck region are common in patients of all ages. These lesions are traditionally classified as acquired or congenital. Common acquired lesions include telangiectasias, spider and cherry angiomas, pyogenic granulomas, and venous lakes. Vascular lesions are characterized by varying degrees of blood vessel dilation.36 Congenital vascular lesions present as either hemangiomas or true vascular malformations.36,37 Histologically, hemangiomas show endothelial cell hyperplasia, whereas vascular malformations are characterized by normal endothelial cells with vessel dilation.38 Hemangiomas are the most common soft tissue tumors of infancy (5%-10% of 1-year-olds).39 Traditionally, hemangiomas spontaneously involute between ages 5 and 10 years.40 The most common vascular malformations are port-wine stains, which are present at birth (0.3%-0.5% of general population41) and do not spontaneously involute.36
The ultimate goal of laser treatment of vascular lesions is selective destruction of abnormal vessels by heating of the vessel wall through the absorption of light by hemoglobin.36 The wavelength chosen should be selectively absorbed by hemoglobin, and the pulse length should be short enough to confine heat to the blood vessels to prevent unwanted damage to adjacent tissue.10 The most common types used for removal of vascular lesions are the argon, KTP, Nd:YAG, and pulsed dye laser (PDL). In addition, IPL systems may also be used.
Telangiectasias are permanently dilated superficial vessels resulting in blue or reddish face.42 These common asymptomatic lesions are often a cosmetic nuisance to the presenting patient. The most common devices used to treat telangiectasias are the PDL and the IPL system. The PDL emits wavelengths of 585 to 600 nm and is better suited for more focal cutaneous lesions; the IPL source emits light in the range of 500 to 1200 nm and is better suited for more diffuse telangiectasias, such as seen with rosacea.36 The major drawback of the PDL vs. IPL system is the postoperative purpura for 7 to 10 days.10 The patient should be thoroughly prepared for this preoperatively, and makeup can be applied immediately after the procedure.36
Treatment of port-wine stains is similar to that for telangiectasias because both represent lesions of dilated superficial blood vessels. Port-wine stains typically occur in younger children and can have significant psychological effects during the child’s development if left untreated. The PDL is most often used for these lesions.39 Multiple treatments are usually required, and lesions partially resistant to the PDL may develop. Pence et al.43 used the frequency-doubled Nd:YAG laser (532 nm) to treat 89 patients with port-wine stains of the head and neck for 1 to 12 sessions, with no treatment failures and 1% to 2% with adverse side effects (e.g., transient hyper/hypopigmentation, hypotrophic scarring). Therefore, combination therapy, with the PDL initially, then the Nd:YAG laser for deeper, more resistant lesions, is likely to produce the best results.
Superficial hemangiomas appear flat and red, whereas deeper lesions appear blue.10 All hemangiomas eventually involute, but delaying treatment can leave lasting cosmetic and psychological scars. Laser treatment of hemangiomas on the skin is similar to that for port-wine stains. The PDL is typically used for hemangiomas with a superficial presentation, whereas the Nd:YAG laser provides the best results for deeper lesions.44 The PDL and Nd:YAG lasers may be used in combination for hemangiomas with superficial and deep components.39
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses