Facial pain
14.1 Assessment of a patient suffering from orofacial pain
• the nature of the pain: encourage the patient to describe the pain in their own words by the use of open questions rather than supplying them with a list of descriptors of pain from which to select; the latter can be useful if a patient is finding it particularly difficult to describe their pain. The use of a 0 to 10 scale can assist patients in expressing the severity of their pain with 0 being pain free and 10 representing the worst pain that the patient has ever experienced
• the duration of each episode of pain
• the frequency of the painful episodes: how often do episodes of pain occur; what is the longest and shortest time the patient has been symptom free
• the site(s) affected: ask the patient to point to the source of the pain and/or outline the area affected by it; does the pain radiate to other areas? Is it confined to the distribution of a particular nerve(s) or does it cross anatomical boundaries, for example the midline?
• initiating factors: anything that the patient remembers occurring immediately before or at the same time as the start of their symptoms
• precipitating factors: anything which now seems to induce the patient’s symptoms
• exacerbating factors: anything which makes the patient’s symptoms worse
• ameliorating factors: anything which relieves, either partially or totally, the patient’s symptoms
A thorough extraoral (including the temporomandibular joint and muscles of mastication) and intraoral examination (see Chapter 2) is obviously mandatory. Additional components of the examination procedure may be required depending on the differential diagnosis, for example assessment of cranial nerve function in patients presenting with symptoms of trigeminal neuralgia. The differential diagnosis will be based on a combination of the outcome of the examination and history. The special investigations that are carried out (these may not always be necessary) will be aimed at clarifying the differential diagnosis and should be carefully tailored to fulfil this purpose, not used as a general screening procedure.
14.2 The neuralgias
Trigeminal neuralgia
Clinical presentation
Age: Predominantly affects individuals over the age of 50 years. This is significant, as its presence in younger individuals is suggestive of STN
Nature: A sharp, stabbing, episodic, electric shock-like pain. Often the pain is so intense that the patient has to stop what they are doing.
Duration: Usually of seconds duration but may last for up to 2 minutes. Occasionally a dull pain persists in the background after the sharp pain has resolved. In severe cases, the episodes of pain may be so close together that they seem continuous, but this is unusual. Spontaneous remission of symptoms can occur, but both this and their recurrence are unpredictable.
Site: The pain is localised to one or more divisions of the trigeminal nerve, most commonly the second and third division. The patient outlines the distribution of the appropriate division(s) when asked to indicate the area affected by the pain. The pain does not usually cross the midline. Bilateral TN is unusual and suggestive of STN.
Initiating factors: The pain may be induced when a particular area of the skin or mucosa is stimulated, the so-called ‘trigger zone’ but this is not invariably the case. Activities of daily living, for example washing the face, shaving, putting on make-up, eating, speaking and exposure to cold may all induce pain.
Associated signs and symptoms: The absence of associated signs and symptoms of sensory or motor deficit is important. Neurological assessment can play a significant role in differentiating between CTN and STN. Trigeminal sensory deficits may be a feature of the latter. The patient’s medical history may already have revealed the existence of a structural abnormality
Glossopharyngeal neuralgia
Glossopharyngeal neuralgia is an extremely uncommon condition.
Clinical presentation
Nature: There is sharp, stabbing, episodic, electric shock-like pain. Pain may be so severe that the patient tries to keep their tongue still and avoids swallowing.
Duration: Usually of seconds duration. Spontaneous remission of symptoms can occur but both this and their recurrence are unpredictable.
Site: The pain is localised to the posterolateral tongue and fauces but felt within the ear on the affected side.
Initiating factors: The pain is induced by stimuli such as eating, drinking, swallowing, speaking and coughing.
Associated signs and symptoms: The absence of associated signs and symptoms of sensory or motor deficit is important. Neurological assessment is mandatory to ensure that the symptoms of glossopharyngeal neuralgia are not the result of a lesion (neoplastic or non-neoplastic) within the posterior cranial fossa or jugular foramen. The patient’s medical history may already have revealed the existence of such a lesion.
Preherpetic neuralgia
Development of the classic vesicles of herpes zoster (Chapter 11; Fig. 14.1) is, in some cases, preceded by facial pain. This leads to the diagnosis being made retrospectively in many cases.
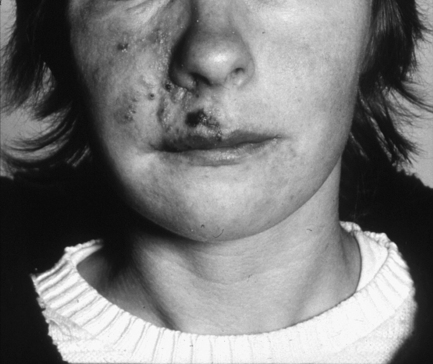
Fig. 14.1 Vesicles of herpes zoster.
Clinical presentation
Postherpetic neuralgia
Clinical presentation
14.3 Pain of vascular origin
Migraine
Site: The pain is usually unilateral but may not always affect the same side of the head. Certain variants are centered on the eye.
Special investigations
CT and MRI do not contribute directly to the diagnosis of migraine but, where signs and symptoms are atypical, are important in excluding the presence of intracranial lesions.
Cluster headaches
Duration: Typically, there are intermittent episodes of pain of between 15 and 180 minutes’ duration on a daily basis for several weeks, interspersed with pain-free periods of months rather than days in duration.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


