Available Bone and Dental Implant Treatment Plans
Carl E. Misch
Long-term success in implant dentistry requires the evaluation of more than 50 dental criteria, many of which are unique to this discipline.1 However, the doctor’s training and experience and the amount and density of available bone in the edentulous site of the patient are arguably primary determining factors in predicting individual patient success. In the past, the available bone was not modified and was the primary intraoral factor influencing the treatment plan. Today the prosthodontic needs and desires of the patient should be first determined, relative to the number and position of missing teeth. After the intended prosthesis and key implant positions are designed, the patient force factors and bone density are then evaluated to determine the additional implant number and size. After these factors are considered, the most important element in the implant region to fulfill the ideal treatment plan is the available bone. Greenfield already appreciated its importance in implant dentistry in 1913.2 This chapter describes the three-dimensional concept of available bone and the implant treatment options for each type of bone anatomy.
Literature Review
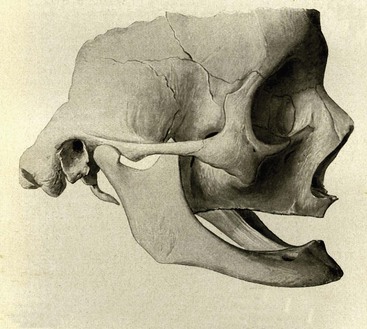
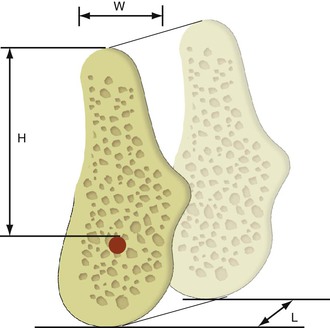
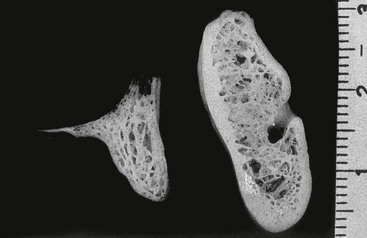
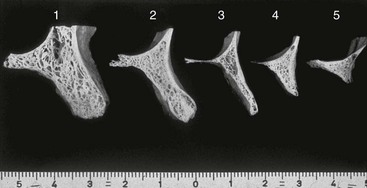
The process of bone volume atrophy after tooth loss and its effect on dentures was reported as early as 1922 by J. Misch3 (Figure 14-1). Since that time, many researchers and clinicians have studied its process and effect on dentistry.4–17 Characteristic bone volume changes after tooth loss were evaluated in the edentulous anterior mandible by Atwood in 19634–6 (Figure 14-2). The five residual ridge stages are beneficial to appreciate the shapes and range of bone loss. Tallgren reported the amount of bone loss occurring the first year after tooth loss is almost 10 times greater than the following years.7 Other more recent studies in complete denture wearers have confirmed the higher rate of resorption in the first year of edentulousness.10,11 Karkazis et al. found, in the mandibular symphysis, that women present higher total reduction and more rapid bone loss during the first 2 years.9 The posterior edentulous mandible resorbs at a rate approximately four times faster than the anterior edentulous mandible.8

The edentulous anterior maxilla appears to resorb in height slower than the anterior mandible. However, the original height of available bone in the anterior mandible is twice as much as the anterior maxilla. Therefore, the resultant maxillary atrophy in height, although slower, affects the potential available bone for an implant patient with equal frequency. The changes in the edentulous anterior maxillary ridge dimension can be dramatic in height and width (up to 70%), especially when multiple extractions are performed.12 In addition, many patients lose additional bone by simultaneous alveolectomy procedures after tooth extraction before the delivery of a maxillary denture.13 Although slight differences exist between different alveolectomy techniques, all are detrimental to the ridge volume.14
The residual ridge resorbs in a palatal direction in the maxilla and lingually in the mandible as related to tooth position at the expense of the buccal cortical plate in all areas of the jaws regardless of the number of teeth missing.15–19 However, after the initial bone loss, the maxilla continues to resorb toward the midline, but the mandibular basal bone is wider than the original alveolar bone position and results in the late mandible resorption progressing more facially (Figure 14-3). This, in addition to a marked change in mandibular position, leads to the classical appearance of the denture wearer with a protruding chin and mandibular lip (e.g., especially when restored at a closed vertical dimension).20
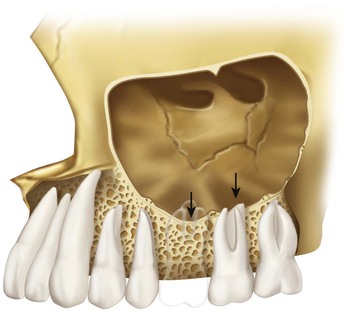
The posterior maxilla loses bone volume faster than any other region. Not only does periodontal disease cause initial bone loss before the loss of teeth, but the crestal bone loss is also substantial after tooth extraction. In addition, the maxillary sinus after tooth loss expands toward the crest of the edentulous ridge (Figure 14-4). As a result, the posterior maxilla is more often indicated for bone augmentation compared with any other intraoral location.
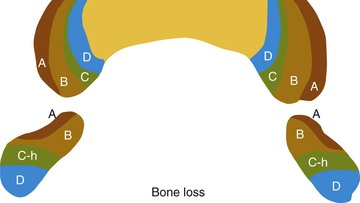
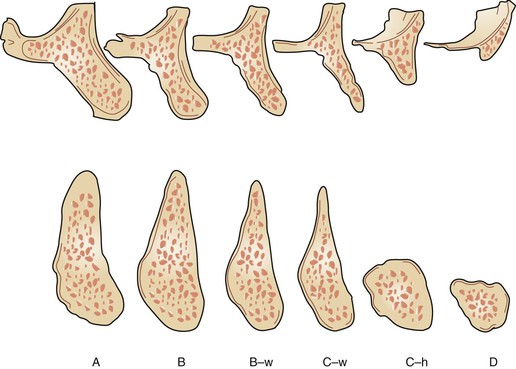
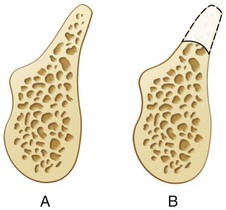
Weiss and Judy developed a classification of mandibular atrophy and its influence on subperiosteal implant therapy in 1974.21 Kent presented a classification of alveolar ridge deficiency designed for alloplastic bone augmentation in 1982.22 Another bone volume classification for the anterior regions of the jaws was proposed by Lekholm and Zarb in 1985 for residual jaw morphology related to the insertion of Brånemark fixtures.23 They described five stages of anterior jaw resorption, ranging from minimal to extreme (Figure 14-5). The mandibular resorption was only described in loss of height. All the five stages of resorption in either arch used the same implant modality, surgical approach, and type of final prosthesis. In addition, as the bone volume decreased, the implants became shorter and the number of implants reduced to support a cantilevered fixed prosthesis. The classifications of Atwood and Zarb and Lekholm do not describe the actual resorption process of the bone in chronological order and are more descriptive of the residual ridge by clinical appearance.
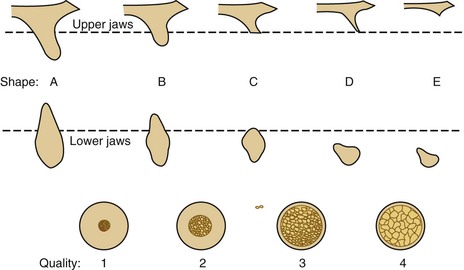
A maxillary alveolar process of resorption after tooth loss following Atwood’s description for the anterior mandible was presented by Fallschüssel in 1986.24 The six resorption categories of this arch ranged from fully preserved to moderately wide and high, narrow and high, sharp and high, wide and reduced in height, and severely atrophic. The Fallschüssel classification is more anatomically correct.25 Another bone resorption classification, which included the expansion of the maxillary sinuses, was proposed by Cawood and Howell in 1988.26 As a consequence, it is more descriptive of the posterior maxilla and is similar to the other classifications relative to the bone volume changes.
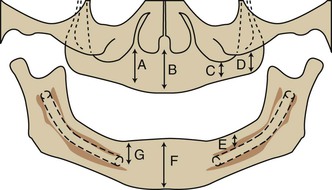
In 1985, Misch and Judy established four basic divisions of available bone for implant dentistry in the edentulous maxilla and mandible, which follow the natural bone resorption phenomena of each region, and determined a different implant approach to each category.27–33 The angulation of bone and crown height were also included for each bone volume because they affect the prosthetic treatment. These original four divisions of bone were further expanded with two subcategories to provide an organized approach to implant treatment options for surgery, bone grafting, and prosthodontics34 (Figure 14-6).
The ability to organize the available bone of the potential implant site into specific related categories of common treatment options and conditions is of benefit to both beginning and experienced clinicians. Improved communication among health professionals and the collection of relevant specific data for each category are also beneficial. The Misch–Judy bone classification has facilitated these processes during the past 2.5 decades within the profession, universities, implant programs, and international implant societies.
Available Bone
To develop an ideal implant treatment plan, the category and design of the final prosthesis and key implant positions are first determined after a patient interview and evaluation of existing medical and dental conditions. The patient force factors and bone density are of particular note to help determine the additional implants required to support the intended prosthesis. The implant abutments necessary to support the restoration are established in position, number, and size and without initial regard to the available bone conditions. The available bone is then evaluated to determine the surgical approach necessary (i.e., bone augmentation, implant insertion, or both) to support the ideal treatment plan.
Available bone describes the amount of bone in the edentulous area considered for implantation. It is measured in width, height, length, and angulation. In addition, the crown height space (CHS) is considered in relation to the remaining bone (Figure 14-7). Historically, the available bone was not modified and dictated the implant position, number, and size. Today, if the bone is inadequate to support an ideal abutment for the intended prosthesis, a bone graft is considered in the ideal site(s) or alternative sites may be considered when additional implant numbers are necessary.
Manufacturers describe the root form implant in dimensions of width and length. The implant length corresponds to the height of available bone. Therefore, this text refers to root form implant height or length. The width of a root form implant is most often related to its diameter because most root form implants are round. This dimension also corresponds to the mesiodistal length of available bone. Many manufacturers design implants with a crest module wider than the implant body dimension. Yet the often stated dimension of the manufacturer is the smaller implant body width. For example, the Nobel Biocare 3.75-mm-diameter implant has a 4.1-mm crest module. The clinician should be aware of all the implant dimensions, especially because the wider implant crest module is positioned next to an adjacent tooth or at the crestal dimension of bone and is usually the dimension responsible for cervical esthetics or the narrowest width region of the available bone.
As a general guideline, at least 1.5 to 2 mm of surgical error is maintained between the implant and any adjacent or opposing landmark. This is especially critical relative to implant length when the opposing landmark is the mandibular inferior alveolar nerve. However, the implant may often be placed without complication through the cortical plate of the posterior region of the maxillary sinus or inferior border of the anterior mandible. The 1.5- to 2-mm or more guideline is also suggested relative to the width of the implant adjacent to a natural tooth. Otherwise, if the implant or tooth should lose crestal bone or become mobile or affected by periimplant disease, the adjacent structure may be adversely involved.
All natural teeth are not equal when considered as abutments for a prosthesis. Restoring dentists know how to evaluate the surface area of the natural abutment roots. A healthy maxillary first molar with more than 450 mm2 of root surface area constitutes a better abutment for a fixed prosthesis than a mandibular lateral incisor with 150 mm2 of root support. The larger-diameter teeth correspond to the regions of the mouth with greater bite force. Likewise, not all implant body sizes are similar to each other when supporting a prosthetic load. The existing bone volume is necessary to determine, but this dimension alone should not determine the ideal implant size. The previous chapter addressed implant size related to function andesthetics. When the ideal implant size cannot be inserted into the existing available bone, bone augmentation, additional implant numbers, or both are considered.
Available Bone Height
The available bone height is first estimated by radiographic evaluation in the edentulous ideal and optional regions, where implant abutments are required for the intended prosthesis. A panoramic radiograph is the most common method for the preliminary determination of the available bone height when multiple adjacent teeth are missing. A periapical radiograph is most often sufficient for this height estimation of one or two adjacent teeth missing.
The height of available bone is measured from the crest of the edentulous ridge to the opposing landmark. The anterior regions are limited in the maxilla by the floor of the nose or in the mandible by the inferior border (Figure 14-8). The anterior regions of the jaws have the greatest height because the maxillary sinus and inferior alveolar nerve limit this dimension in the posterior regions. The maxillary canine eminence region, just lateral to the lateral periform rim of the nose, often offers the greatest height of available bone in the maxillary anterior.35
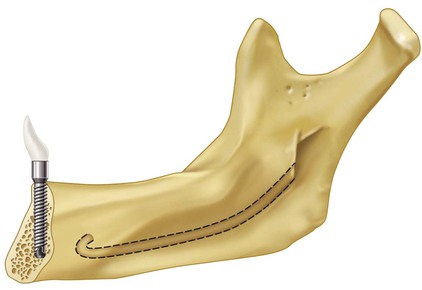
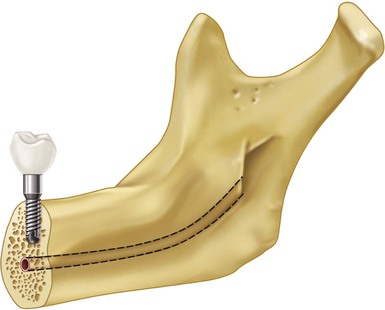
As a general rule, the anterior mandible has the greatest bone height. There is more bone apical to the mandibular anterior teeth than any other region. Hence, even after the resorption of the residual ridge after tooth loss, there is adequate bone to insert dental implants (Figure 14-9). However, the crown height of the prosthesis may be extensive. Therefore, this region often has the most available bone but also may have the greatest CHS.
The anterior bone region in the mandible extends between the mental foramen. The foramen is most often found between (and below) the apices of the two premolars. Hence, the anterior region of bone extends beyond the canines and to the first premolar region most often. The presence of available bone in implant dentistry involves the existing anatomy of the edentulous mandible and maxilla. The initial mandibular bone height is influenced by skeletal anatomy, with angle class II patients having shorter mandibular height and angle class III patients exhibiting the greatest height.
The opposing landmarks for both the maxilla and mandible of the initial available bone height are more limiting in the posterior regions distal to the first premolar. In the maxillary posterior jaw region, there is usually greater bone height in the first premolar than in the second premolar, which has greater height than the molar sites because of the concave morphology of the maxillary sinus floor. As a consequence, the existing bone anatomy of the implant patient often requires modification to enhance long-term implant success. For example, sinus grafts in the posterior maxilla permit the placement of posterior endosteal implants into restored bone height.
The posterior height of bone in the mandibular region is reduced because of the presence of the mandibular canal, situated approximately 12 mm above the inferior border of the mandible (Figure 14-10). The height of bone in a posterior mandible (before crestal bone loss) is similar to the height of bone in the anterior maxilla (Figure 14-11). On occasion, this premolar site may present a reduced height compared with the anterior region because the anterior loop of the mandibular canal (when present) passes below the foramen and loops superiorly and then distally before its exit through the mental foramen (see Figure 14-9).
As a result, in the areas where greater forces are generated and the natural dentition has wider teeth with two or three roots, shorter implants, if any, are often used and often in insufficient number because of the anatomical limiting factors.36 Oikarinen et al. found that more than 6 mm of bone height is found in less than 50% of posterior mandibles and 40% of posterior maxillae in partially edentulous patients.36 The author observed more than 6 mm of bone is found in less than 20% of posterior mandibles and 10% of posterior maxillae when the patient has been fully edentulous more than 5 years.
The suggested minimum bone height for predictable long-term endosteal implant survival approaches 12 mm. Failure rates reported in the literature for implants shorter than 9 mm tend to be higher independent from the manufacturer design, surface characteristic, and type of application.37–52 The inexperienced dentist may wish to have 14 mm of bone height to place a 12-mm-long implant body before proceeding with the surgery. This precaution allows 2 mm of surgical error or permits an osteoplasty to gain additional width of bone. The 12-mm height minimum applies to most screw-shaped endosteal implant designs in good density (D2, D3) bone. This minimum implant height requirement may be reduced in the very dense bone (D1) in the symphysis of an atrophic mandible when the prosthesis has fewer forces (as an overdenture) or when the shorter dimension can be compensated by implant number, width, or design.53–55
The available bone height in an edentulous site is the most important dimension for implant consideration because it affects both implant length and crown height. Crown height affects force factors and esthetics. In addition, bone augmentation is more predictable in width than height, so even when the width is inadequate for implant placement, bone grafting may be used to create a site ideal for restorative and implant insertion requirements.
Available Bone Width
The width of available bone is measured between the facial and lingual plates at the crest of the potential implant site. The crestal aspect of the residual ridge in the mandible is often cortical in nature and exhibits greater density than the underlying trabecular bone regions. This mechanical advantage permits immediate fixation of the implant, provided this cortical layer has not been removed by osteoplasty.
The crest of the edentulous ridge is most often supported by a wider base in the anterior mandible. In most mandibular situations, because of this triangular-shaped cross-section, an osteoplasty provides greater width of bone, although of reduced height (Figures 14-12).
It should be noted that crest reduction affects the location of the opposing landmark, with possible consequences for surgery, implant height selection, appearance, and the design of the final prosthesis. This is particularly important when a FP-1 prosthesis is planned, with the goal of obtaining a normal contour and proper soft tissue drape around a single tooth replacement.
Unlike the anterior mandible, the anterior maxilla often does not follow the triangular-shaped anatomy. The palatal plate of bone is more parallel to the facial plate in the maxilla (Figure 14-13). In addition, many edentulous ridges exhibit a labial concavity in the incisor area, with an hourglass configuration. As a result, osteoplasty does not increase the width of bone as much as in the mandible. As a consequence, bone augmentation for width is more often indicated in the maxilla.
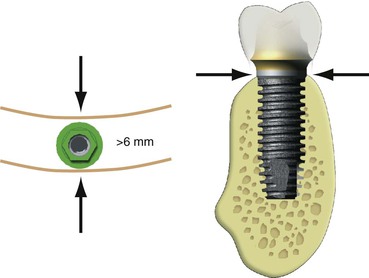
After adequate height is available, the next most significant criterion affecting the long-term survival of endosteal implants is the width of the available bone. Root form implants with crestal diameters of 4 mm usually require more than 6 mm of bone width to ensure sufficient bone thickness and blood supply around the implant for predictable survival. This dimension provides more than 1 mm of bone on each side of the implant at the crest. Because the bone usually widens apically in the mandible, this minimum dimension rapidly increases. For root form implants, the minimum bone thickness is located in the midfacial and midlingual contours of the crestal region exclusively (Figure 14-14).
Extraction sockets with more width of bone at the crest around the socket lose less bone during initial healing than sockets with minimum width of cortical plates on the facial or lingual of the extraction site. The initial width of available bone is also related to the amount of crestal bone loss after implant loading. Edentulous ridges that are greater than 6 mm in width have demonstrated less crestal bone loss than when minimum bone dimensions are available.
Available Bone Length
The mesiodistal length of available bone in an edentulous area is often limited by adjacent teeth or implants. As a general rule, the implant should be at least 1.5 mm from an adjacent tooth and 3 mm from an adjacent implant. This dimension not only allows surgical error but also compensates for the width of an implant or tooth crestal defect, which is usually less than 1.4 mm. As a result, if bone loss occurs at the crest module of an implant or from periodontal disease with a tooth, the vertical bone defect will not spread to a horizontal defect and cause bone loss on the adjacent structure.56 Therefore, in the case of a single-tooth replacement, the minimum length of available bone necessary for an endosteal implant depends on the width of the implant. For example, a 5-mm-diameter implant should have at least 8 mm of mesiodistal bone, so 1.5 mm is present on each side of the implant. A minimum mesiodistal length of 7 mm is usually sufficient for a 4-mm-diameter implant.
The diameter of the implant is also related to the width of available bone and, in multiple adjacent sites, is primarily limited in this dimension. For example, a width of bone of 4.5 mm without augmentation requires a 3.5-mm or smaller implant, with inherent compromises (e.g., as less surface area and greater crestal stress concentration under occlusal loads on abutment screw and marginal bone). Therefore, in the narrower ridge, it is often indicated to place two or more adjacent narrow-diameter implants (when possible) to obtain sufficient implant–bone surface area to compensate for the deficiency in width of the implant. Because the implants should be 3 mm apart and 1.5 mm from each tooth, 13 mm or more in available bone mesiodistal length may be required when the narrower implant dimensions are used to replace a posterior tooth.
The ideal implant mesiodistal width for single-tooth replacement is often related to the natural tooth being replaced in the site. The tooth has its greatest width at the interproximal contacts; is narrower at the cementoenamel junction (CEJ); and is even narrower at the initial crestal bone contact, which is 2 mm below the CEJ.57 The ideal implant diameter corresponds to the width of the natural tooth 2 mm below the CEJ if it also is 1.5 mm from the adjacent tooth. In this way, the implant crown emergence through the soft tissue may be similar to a natural tooth. For example, a maxillary first premolar is approximately 8 mm at the interproximal contact, 5 mm at the CEJ, and 4 mm at a point 2 mm below the CEJ. Therefore, a 4-mm-diameter implant (at the crest module) would be the ideal implant diameter if it also is at least 1.5 mm from the adjacent roots (2 mm below the CEJ). The ideal width of available bone for this 4-mm-diameter size implant is 6 mm or more, and the ideal bone mesiodistal length is 7 mm or more.
Available Bone Angulation
Bone angulation is the fourth determinant for available bone. The initial alveolar bone angulation represents the natural tooth root trajectory in relation to the occlusal plane. Ideally, it is perpendicular to the plane of occlusion, which is aligned with the forces of occlusion and is parallel to the long axis of the prosthodontic restoration. The incisal and occlusal surfaces of the teeth follow the curve of Wilson and curve of Spee. As such, the roots of the maxillary teeth are angled toward a common point approximately 4 inches away. The mandibular roots flare, so the anatomical crowns are more lingually inclined in the posterior regions and labially inclined in the anterior area compared with the underlying roots. The first premolar cusp tip is usually vertical to its root apex.
The maxillary anterior teeth are the only segment in either arch that does not receive a long-axis load to the tooth roots but instead are usually loaded at a 12-degree angle. As such, their root diameter is greater than the mandibular anterior teeth. In all other regions, the teeth are loaded perpendicular to the curves of Wilson and Spee.
Rarely does the bone angulation remain ideal after the loss of teeth, especially in the anterior edentulous arch. In this region, labial undercuts and resorption after tooth loss often mandate greater angulation of the implants or correction of the site before insertion.12,15,16 For example, in the anterior mandible, the implant insertion often engages the lingual cortical plate, rather than the inferior border of the mandible, as a consequence of the position of the incisal edge and the angulation of bone (see Figure 14-9). In the posterior mandible, the submandibular fossa mandates implant placement with increasing angulation as it distally progresses. Therefore, in the second premolar region, the angulation may be 10 degrees to a horizontal plane; in the first molar areas, 15 degrees; and in the second molar region, 20 to 25 degrees.
The limiting factor of angulation of force between the body and the abutment of an implant is correlated to the width of bone. In edentulous areas with a wide ridge, wider root form implants may be selected. Such implants may allow up to 30 degrees of divergence with the adjacent implants, natural teeth, or axial forces of occlusion with minimum compromise. The angled load to an implant body increases the crestal stresses to the implant components and bone, but the greater–diameter implant decreases the amount of stress transmitted to these structures. In addition, the greater width of bone offers some latitude in angulation at implant placement. The implant body may often be inserted so as to reduce the divergence of the abutments without compromising the permucosal site. Therefore, an acceptable bone angulation in the wider ridge may be as much as 30 degrees.
The narrow yet adequate width ridge often requires a narrower design root form implant. Compared with larger diameters, smaller-diameter designs cause greater crestal stress to the system (abutment screws, crestal bone) and may not offer the same range of custom abutments. In addition, the narrower width of bone does not permit as much latitude in placement regarding angulation within the bone. This limits the acceptable angulation of bone in the narrow ridge to 20 degrees from the axis of the adjacent clinical crowns or a line perpendicular to the occlusal plane.
Crown Height Space
The CHS is defined as the vertical distance from the crest of the ridge to the occlusal plane. It affects the appearance of the final prosthesis and may affect the amount of moment force on the implant and surrounding crestal bone during occlusal loading. Esthetically, the prosthesis is less likely to replace the sole anatomical crowns of natural teeth when a greater CHS is present.
The CHS may be considered a vertical cantilever. Any direction of load that is not in the long axis of the implant will magnify the crestal stresses to the implant–bone interface and to the abutment screws in the restoration. The greater the CHS, the greater the moment force or lever arm with any lateral force or cantilever (Figure 14-15).
The absence of a periimplant ligament means that the bone–implant stresses cannot be reduced by increasing the implant height. Therefore, as the CHS increases and a cantilever or a lateral load is planned on the restoration, a greater number of implants or wider implants should be inserted to counteract the increase in stress. For an ideal treatment plan, the CHS should be equal to or less than 15 mm under ideal conditions.
Divisions of Available Bone
Division A (Abundant Bone)
Division A abundant bone often forms soon after the tooth is extracted. The abundant bone volume remains for a few years, although the residual bone height is slowly reduced and the original crestal width is usually reduced by more than 30% within 2 years.12 Division A bone corresponds to abundant available bone in all dimensions.
The height of available bone for division A is 12 mm or more. It should be emphasized that the available bone height may be 20 mm for division A, but this does not mean the implant length must be equal to the bone height. Because the stresses to the implant interface in good-density bone are captured within the coronal two thirds of the implant, an implant of 12 mm has been shown to be without compromise for long-term success even though the implant does not engage the opposing cortical plate.
The width of available bone for division A is 6 mm or more. The division A width of more than 6 mm is predicated on an implant diameter of at least 4 mm at the crest module because abundant long term data have been published regarding this implant size. In abundant bone width of greater than 7 mm (A+ bone), a wider (5-mm-diameter) implant may be inserted, provided that at least 1 mm of bone remains around the buccal and lingual aspects of the implant. Osteoplasty may often be performed to obtain additional bone width in the mandible when a larger diameter implant is desired.
The mesiodistal edentulous span for division A bone is 7 mm or more. This is adequate for a 4-mm-diameter implant. The angulation of the bone in reference to the occlusal plane is within 30 degrees. Hence, even when an angled abutment is necessary to restore the patient, the direction of load is not excessive. The CHS for division A is less than 15 mm. This is an ideal dimension for a fixed implant prosthesis (Box 14-1).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses