Relationship between Restorative Treatment and Periodontal Health
Surgical Clinical Crown Lengthening
Overview
Osseous surgery aims to reshape the alveolar bone to remove any anatomic discrepancy between the soft tissues and the underlying bone so that it can heal with a normal physiologic gingival architecture (Figure 13-1). The different types of bone lesions can be treated with three approaches.
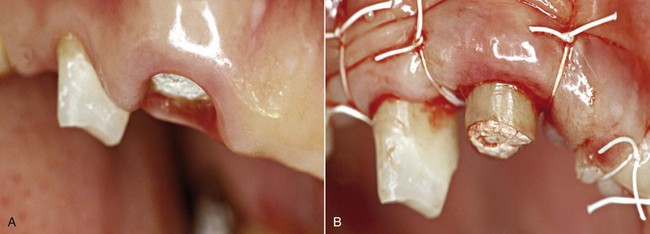
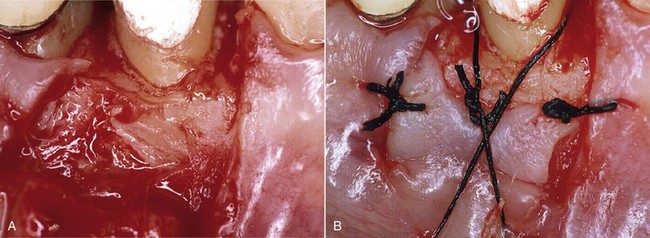
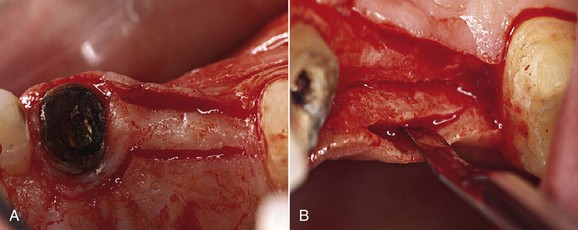
Figure 13-1 A, Clinical preoperative image. B, Flap positioned apically with the periosteal suturing technique.
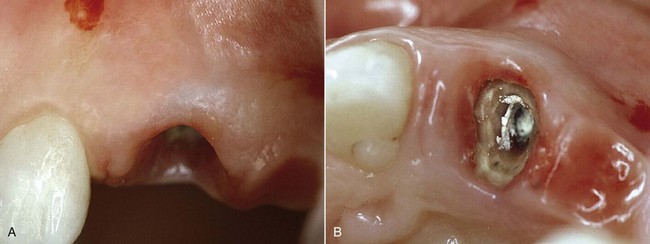
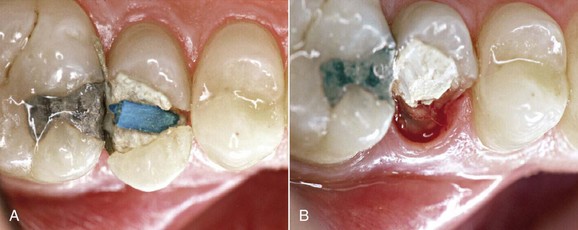
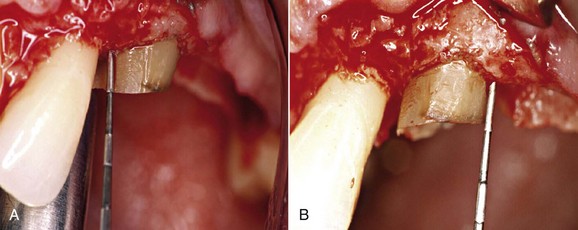
The pictures of the outcomes of clinical crown-lengthening procedures performed about 20 years ago (Figures 13-2 and 13-3) clearly show the cosmetic damage that at the time was considered inevitable for proper treatment of the disease.

Figure 13-2 Case of clinical crown lengthening performed 20 years ago. A, Preoperative status. B, Healing at 3 months.
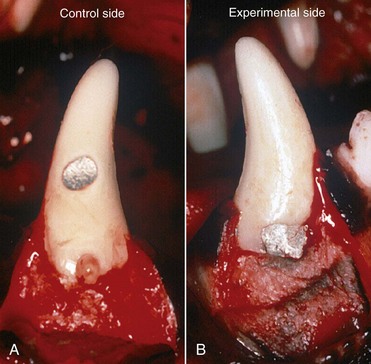
The first study that examined the healing process with insufficient biologic width was conducted on canine dentition by Parma Benfenati, Fugazzotto, and Ruben (1985). The protocol entailed creating cavities at different locations as follows:
• Control side: Class V amalgam restorations performed outside the biologic width, coronally to the bone crest, where a mark was placed for histologic purposes (Figure 13-4, A)
• Experimental side: Class V cavities filled with amalgam at the bony ridge level (Figure 13-4, B)
Esthetic needs greatly affect the choice of treatment. It should be remembered that osseous resective surgery with apical positioning of the flap changes the emergence profile of the tooth, which will be more apical and palatal with respect to its original position. This may greatly affect subsequent restoration treatment (Figure 13-5).
Treatment
Gingivectomy
The gingivectomy procedure can be performed with different types of incisions to permit the opening and repositioning of several types of flaps (Figures 13-6 and 13-7).
Coronal Fracture
Root fracture is the ideal indication for a clinical crown-lengthening procedure.
Fracture above the Gingival Attachment
In this case it is possible to perform a direct or indirect restoration without surgery.
Subgingival Caries
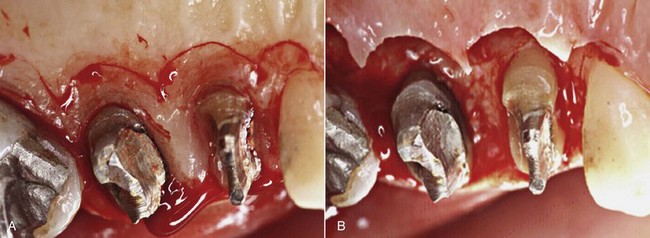
Figures 13-8 and 13-9 show a case of clinical crown lengthening I performed many years ago. Placement of the rubber dam is mandatory for this procedure in order to remove the decayed tissue (even if it is below the gingival margin) and to choose the most appropriate restoration for the specific case.
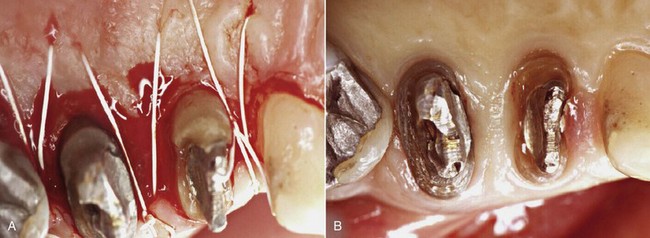
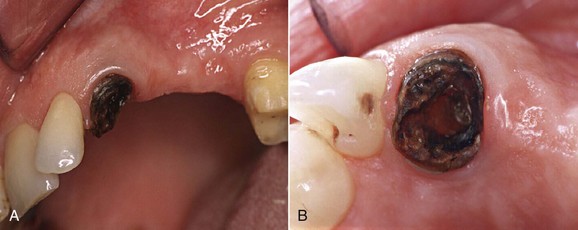
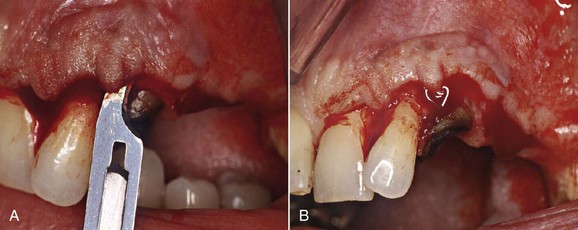
Fracture
Bleeding after removal of the tooth fragment confirms the diagnosis of fracture below the gingival attachment. In the clinical case treated over 20 years ago (Figures 13-10 and 13-11), the palatal cusp of the premolar was reduced to prevent further fracture.
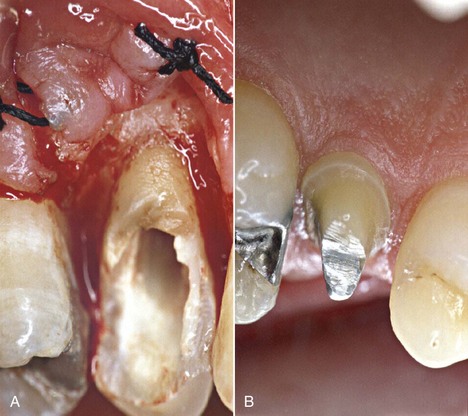
Figure 13-11 A, Suturing of the flap. B, Healing at 6 months.
Surgical Protocol
1. After administration of local anesthesia, an intrasulcular incision is performed in order to preserve the existing keratinized tissue, extending the incision into the grooves of two adjacent teeth and reducing the thickness of their mesial and distal papillae. A partial-thickness flap is then raised a few millimeters beyond the mucogingival junction, which makes the flap extremely mobile and permits the proper and desired apical positioning.
2. After probing, a palatal flap is created on the palatal side and is reduced in thickness by outlining the shape of the bony ridge. The shape of this flap is created with a scalpel blade no. 15C oriented perpendicular to the long axis of the tooth. The surgery begins with a paramarginal incision, which is more pronounced in the area of the tooth to be restored prosthetically. The incision then becomes intrasulcular, next to the mesial and distal ends of the adjacent teeth. This is followed by a series of incisions, placing the scalpel blade parallel to the long axis of the tooth in order to thin it out (primary palatal flap). After the desired apical extension has been achieved, a full-thickness incision is then performed apically, reaching the palatal bone structure only at this point.
3. After removal of the excess tissue (secondary palatal flap), all granulomatous tissue is removed with rotary or manual instruments. Root preparation is performed with a suitable diamond bur.
4. At this point the surgery requires removal of the bone support (ostectomy) from the interproximal areas with a CTG-O bone chisel, in order to reduce the bone by approximately 3 to 4 mm starting from the healthy tooth structure. The ostectomy is also performed on the palatal and vestibular aspect of the ridge with a Rhodes chisel and round-shaped diamond burs. This procedure produces the desired bone architecture: scalloped, with parabolic contours and physiologic in appearance. A universal curette can be used to remove small spicules of interproximal bone and residue of support bone that may affect the desired result. At the end of this surgical phase, the desired clinical crown lengthening—performed respecting the bone architecture—is assessed with a periodontal probe.
5. The flaps are then closed with e-PTFE sutures employing a mixed mattress suture technique: vertical, buccal periosteal, and palatal horizontal.
A surgical pack may be placed at the clinician’s discretion.
The case can be completed after the appropriate time required for the healing process (usually 6 to 9 months), fully satisfying the functional esthetic requirements of the clinician and patient alike (Case Report 1, Figures 13-12 to 13-17, and Case Report 2, Figures 13-18 to 13-27).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses